Conservative Management of Large Spontaneous Vaginal Hematoma in the Puerperium
* Sanusi HA;
Das S;
Khan K;
-
* Sanusi HA: Specialty Registrar, Obstetrics and Gynecology Department, Bolton NHS Foundation Trust, BL4 0JR, United Kingdom.
-
Das S: Consultant, Department of Obstetrics and Gynecology, Bolton NHS Foundation Trust, BL4 0JR, United Kingdom.
-
Khan K: Consultant, Department of Radiology, Bolton NHS Foundation Trust, BL4 0JR, United Kingdom.
-
Feb 14, 2022 |
-
Volume: 3 |
-
Issue: 2 |
-
Views: 2304 |
-
Downloads: 787
-
Download PDF
Abstract
Spontaneous occurrence of pelvic floor hematoma is not common, and there is no specific figure in literature for its incidence. Most cases of pelvic hematomas arise from bleeding lacerations following operative deliveries or episiotomies; therefore, a high index of suspicion is needed when a patient presents with excessive perineal and back pain following a normal vaginal delivery as early detection of puerperal hematomas prevents morbidity and mortality. Most cases of large vaginal hematomas are managed with surgical or radiological intervention. There are, however, a few documented cases of conservative management for large hematomas.
We present 2 cases; the first one was the case of a 31-year-old multiparous lady who complained of severe perineal discomfort three hours following vaginal delivery. A fullness was felt in the left fornix on examination. A bedside ultrasound scan was in keeping with an organized hematoma at the lower end of the cervix level. This was confirmed on computerized tomography (CT scan). She remained hemodynamically stable and was managed with analgesia, intravenous fluids, antibiotics, tranexamic acid, and serial blood checks. She was discharged home 13 days post-partum.
The second case was a 33-year-old para one who also developed vaginal hematoma 3 hours following a planned home birth. A 5 cm bulge was noted in the right lower third of the vagina. The CT scan revealed a 10 cm x 5 cm hematoma to the right of the vagina extending from the pelvis to the perineum. Her hemoglobin level dropped from 100 grams/liters to 84 grams/liters and remained stable afterward. She was managed with vaginal packing, analgesia, antibiotics, serial blood checks and was discharged on the third-day post-delivery.
Introduction
Spontaneous occurrence of pelvic floor hematoma is uncommon. Most cases of pelvic hematomas arise from bleeding lacerations following operative delivery or episiotomy. The quoted incidence for vaginal hematoma is 0.8/1000 deliveries [1] (ranges from 1:300 to 1:1500) [2]. However, there is no specific figure in the literature for hematomas that occurred spontaneously in the absence of any bleeding lacerations. A high index of suspicion is needed when a patient presents with excessive perineal and back pain following a normal vaginal delivery, as early detection of puerperal hematoma prevents morbidity and mortality.
Most cases of large vaginal hematomas are managed with surgical or radiological intervention. There are, however, a few documented cases of conservative management for large hematomas. Three cases have been reported in the literature [3]; two cases were delayed presentation of vaginal hematoma on day three postpartum, while the third was diagnosed 3 hours after delivery. The clinical course and management of these cases were like the cases presented in this article. It should be noted that the management of genital tract hematomas is based on practice patterns established over the years rather than clinical trials with clearly defined outcomes. Conservative management can be considered in hemodynamically stable patients with no evidence of ongoing bleed irrespective of the size of the hematoma, as exemplified by the successful management of the two cases of large vaginal hematoma examined in this article.
Case Presentation
We present two cases of paravaginal hematomas where conservative management was employed successfully.
The first is a case of a 31-year-old P3 who presented in spontaneous labor at 40 weeks and three days.
She had a previous cesarean delivery in 2017 for pathological cardiotocograph (CTG) followed by a vaginal birth after cesarean section in 2019. She sustained a third-degree tear in 2019, which healed satisfactorily. She was happy to have a vaginal delivery following discussion at the antenatal clinic. She had no known medical condition, and the antenatal period was uneventful.
Her membranes ruptured spontaneously 3 hours after the initial assessment, revealing a clear liquor. She had opioids analgesia and epidural for pain relief. Contractions were augmented with low dose oxytocin 4 mls/hr (of 30 IU oxytocin in 500 mls normal saline) following an assessment of slow progress secondary to inadequate contractions. She subsequently progressed to full cervical dilatation and had a spontaneous vaginal delivery of a live female baby weighing 3470 grams. The total duration of the first stage of labor was 11 hours, while the second stage lasted only 30 minutes. She sustained a second-degree perineal tear on the right vulva, which was repaired in the room. The estimated blood loss was 450 mls.
Three hours post-delivery, she complained of perineal pain. Paracetamol and morphine were given orally; however, she continued to report pain and was advised that her stitches were causing pain. This prompted a review by a senior member of the team. The examination revealed a well-contracted uterus displaced to the right. Upon an inspection of the vulva, the stitches of the second-degree tear repair were found intact. However, a fullness was felt in the left fornix/adnexa, which measured approximately 6 cm. A bedside ultrasound scan was also in keeping with an organized hematoma at the lower end of the cervix. A tentative diagnosis of lateral vaginal wall hematoma was made following the examination.
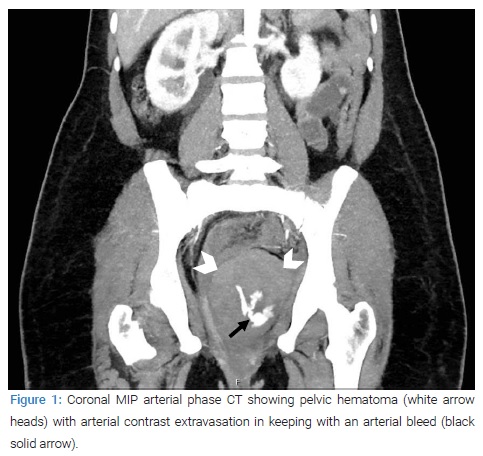
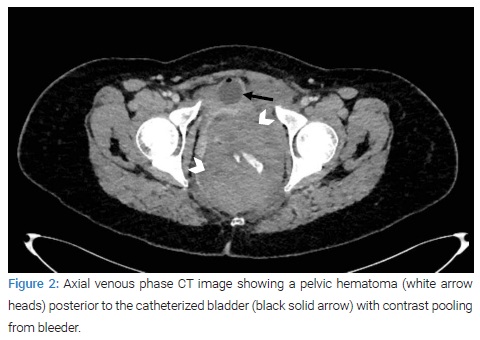
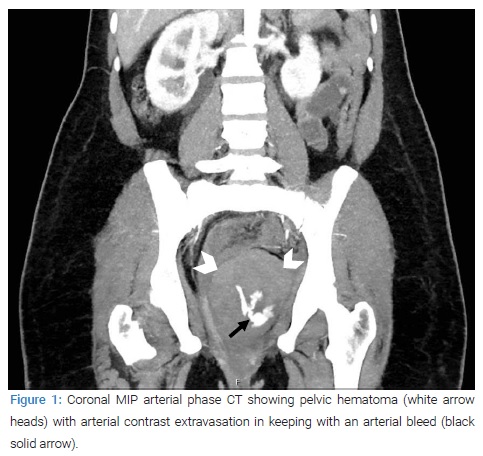
She subsequently had an urgent computerized tomography (CT) scan of the abdomen and pelvis (with contrast) and was transferred to a high dependency unit (HDU) for further care. The CT scan revealed a 10 cm x 8 cm pelvic hematoma, and an internal active bleeder was identified (Figure 1,Figure 2). The hematoma appeared to originate from the left ischiorectal fossa and extended into the peritoneum in the left pouch of Douglas. The local interventional radiologist suggested further discussion regarding the amenability for a vascular interventional radiology procedure and recommended referral to an outside facility for this procedure.
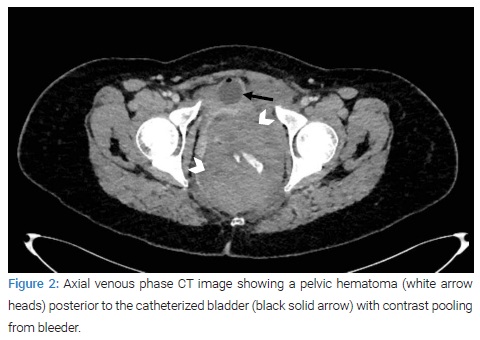
Blood was essentially normal. Two full blood counts six hours apart revealed hemoglobin levels of 117 grams/liters and 114 grams/liters, respectively. After that, a referral was made to a tertiary center as vascular surgery cover was not available locally. She remained hemodynamically stable.
In the tertiary unit, she had a further pelvic CT scan consistent with an organized hematoma as no extravasation of contrast was seen, and the hematoma wall was well-defined. There was also no significant interval change in the hematoma size, which still measured 10 cm x 6.5 cm x 8 cm. A slight increase in the intraperitoneal fluid was noted, particularly in the left paracolic gutter. However, there was no active intraperitoneal hemorrhage. The cause of intraperitoneal hemorrhage could not be confirmed on the CT scan, but the following possibilities were entertained; a tear from the previous lower segment cesarean section site or a proximal extension of the pelvic hematoma, possibly through a tear in the vaginal fornices. Serial hemoglobin (HB) monitoring and repeat CT examination if the further progressive drop in HB were recommended.
She was managed in the high dependency unit (HDU), where she had serial blood checks, hourly urine output monitoring, and pain relief medications. She also received oral tranexamic acid, antibiotics, and laxatives. In addition, two units of blood were grouped and cross-matched for her.
Repeat full blood count showed hemoglobin of 104 grams/liters, which later stabilized at 92 grams/liters on the fifth day of admission. On the seventh day of admission, she became tachycardic with evidence of raised C-reactive protein (CRP). Therefore, the antibiotics were switched to an intravenous route and carried on for seven days. Infection markers improved, so did her clinical parameters. On the 13th day of admission, she was discharged on oral antibiotics and laxatives. She had a follow-up CT scan six weeks later. This revealed a significant reduction in the size of the left posterior extraperitoneal pelvic sidewall hematoma, now measured 2.8 cm x 1.4 cm as opposed to the initial size of 10 cm x 8 cm.
The second case is a 33-year-old para one who presented 3 hours after a planned home birth with back and right hip pain. She went into spontaneous labor at 40 weeks plus four days. Labor was uneventful, and the active phase lasted about 6 hours, while the second stage of labor was about 30 minutes long. She delivered a female neonate with a birth weight of 3250 grams. Estimated blood loss at delivery was 300 mls. Her observations at admission were essentially normal. The uterus was well contracted; however, an asymmetry of the introital area with a 5 cm bulge was noted in the right lower third of the vagina. The medial aspect of the right labium appeared bruised, and no perineal tears were seen. She was also examined rectally, which confirmed that the hematoma had not extended to the ischiorectal fossa.
She was a low-risk primigravida at booking and had midwife-led care. At 39 weeks, she presented at the antenatal day unit with her first episode of reduced fetal movement. The CTG for assessment of fetal well-being was normal. She, however, declined an induction of labor which was offered according to the local protocol for ladies presenting with reduced fetal movement after 39 weeks. She was keen to have a home birth and was aware of the possible risks and complications.
Conservative management was offered because of her hemodynamic status. A vaginal pack was inserted to provide tamponade, and intravenous antibiotics (clindamycin and gentamicin) were commenced. An indwelling catheter was also inserted. In addition, pain relief in the form of opioid analgesia was provided. Initial blood tests revealed a hemoglobin level of 123 grams/liters, a white cell count of 19.4/microlitre, and 138 x109/liters platelets. The clotting profile was normal. The C-reactive protein remained stable at 40. Electrolytes, urea, and creatinine were within the normal range.
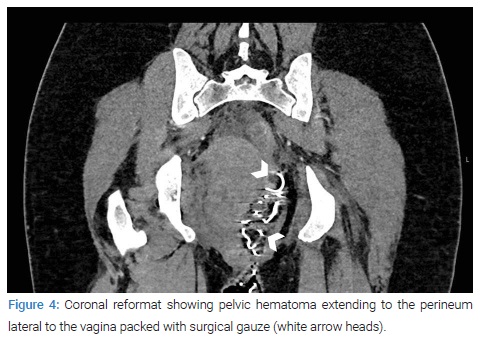
A CT scan of the pelvis done the next day (Figure 3,Figure 4) revealed a 9.2 cm by 7 cm hematoma within the vagina cavity with no obvious active contrast extravasation. A separate hematoma measuring 10.2 cm by 5.1 cm was seen to the right of the vagina extending from the pelvis to the perineum. An extension to the right ischiorectal fossa with fat stranding was also seen. The hematoma was reported as appearing complex with an extension (5 cm) to the right peri-vesicular space. Edema of the rectal wall with fat stranding in the mesorectum and mild free fluid in the right iliac fossa was also noted.

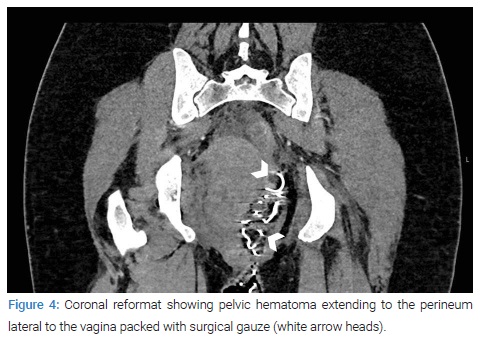
The hematoma seen within the vaginal cavity was thought to be a big clot trapped behind the vaginal pack. There was no evidence of ongoing bleeding in the imaging; therefore, conservative management continued. She remained hemodynamically stable, and intravenous antibiotics were continued for 48 hours while the vaginal pack was removed after 24 hours.
Serial blood checks (every 6 hours) revealed a further drop in her hemoglobin to 100 grams/liters, and thereafter 84 grams/liters. However, it remained stable at 84 grams/liters subsequently.
On the third day of admission, she was discharged with oral antibiotics (to be continued for five days), analgesics, and hematinics. Unfortunately, she had no follow-up scans.
Both patients reported no concerns during routine post-natal checks and were very happy with the outcomes.
Discussion
Puerperal hematomas can be classified into supralevator and infralevator types. Paravaginal and supravaginal/subperitoneal hematomas are referred to as the supralevator type and are caused by injury to the descending branch of the uterine artery and branches of the uterine artery in the broad ligament, respectively [4]. The infralevator types are the vulva and vulvovaginal hematomas caused by injury to the pudendal vessels.
Paravaginal hematomas, as stated earlier, arise from injury to the descending branch of the uterine artery. The hematoma is confined to the paravaginal tissues in the space bounded inferiorly by the pelvic diaphragm and superiorly by the cardinal ligament. Hence, a paravaginal hematoma will not be obvious externally but can be diagnosed by vaginal examination. The mass often occludes the vaginal canal and extends into the ischiorectal fossa, as detailed in the CT scan findings.
Injury can be direct (for example, from a pudendal needle or episiotomy) or indirect (for example, from radial stretching of the birth canal as the fetus passes through). Case series have reported that up to 87% of hematomas are associated with sutured perineal tears or episiotomies, but superficial tissues are not always lacerated. Good surgical technique, with attention to hemostasis in the repair of lacerations and episiotomy, should limit the occurrence of this complication. The hematoma in the first case occurred remotely from the perineal tear and repair. We, therefore, think a cervical trauma or injury to branches of the uterine artery during the birthing process may be responsible. The second case had intact perineum; therefore, the hematoma could have occurred following an injury to the uterine artery branches during delivery. This is an uncommon cause, and given the fact that the baby was of average size and labor was not prolonged, a high index of suspicion was paramount.
Primiparity has been identified as a strong risk factor for a vaginal hematoma in some studies, so are age (> 29 years), birth weight (> 4000 grams), preeclampsia, the prolonged second stage of labor, operative vaginal delivery, multifetal pregnancy, vulvar varicosities, and clotting disorders [1]. However, apart from age and primiparity in one of the patients, the cases presented did not have most of the recognized risk factors.
Symptoms usually develop within a few hours of delivery. The significance they give and the speed of diagnosis will depend on the extent of the bleeding, its effect on the cardiovascular status of the woman, and the level of awareness of midwifery and medical staff. Thus, a woman with a large hematoma may present with collapse within a few hours of delivery, whereas a woman with a small hematoma in an episiotomy may present with persisting pain over a few days. Continued vaginal bleeding is also commonly seen. There was no revealed bleeding in the index cases, and the hallmark symptom was excessive perineal or back pain which prompted pelvic examination.
If a hematoma ruptures into the vagina, the cause must be differentiated from other causes of postpartum hemorrhages, such as the atonic uterus. Hematomas can also present with urinary retention or, rarely, unexplained pyrexia.
Ultrasound (USS), computed tomography (CT), and magnetic resonance imaging (MRI) scans will be mainly helpful for diagnosing hematomas above the pelvic diaphragm and for assessing any extension into the pelvis, particularly as bimanual examinations may not aid in their discovery until they are quite large. MRI can also be beneficial in providing information on the location, size, and extent of a hematoma and monitoring progress or resolution. MRI can help to differentiate between other causes of a pelvic mass, such as an abscess or endometrioma. They are beneficial for evaluating patients at risk of postpartum hemorrhage following difficult vaginal delivery [5].
These cases were managed after normal working hours. A CT scan was readily accessible and therefore was the imaging of choice. The use of intravenous contrast at the time of CT scan can aid diagnosis in cases of arterio-venous (A-V) malformations and retroperitoneal hematoma (these are rare causes of spontaneous puerperal hematomas) [6]. MRI scans are more time-consuming, expensive, and less readily available than ultrasound scans or CT scans but not necessarily more helpful in this setting [6].
Transabdominal (performed with a full bladder) or transperineal sonography can visualize paravaginal hematomas effectively after vaginal delivery. We suggest that ultrasound can be considered the first-line imaging tool in cases of otherwise unexplained postpartum pelvic and perianal pain, swelling of the vulva, and/or urinary retention.
The role of USS cannot be underestimated, especially in low-resource settings where CT or MRI are not readily available. A retrospective study by Bellussi and co suggested that a transabdominal or transperineal sonography can visualize paravaginal hematomas effectively after vaginal delivery and went ahead to recommend it as the first-line imaging tool [7] if the skill is available, the USS may be performed by the patient’s bedside to provide first-hand information on diagnosis and management. It has the additional benefit of better tolerability by patients.
Small, static hematomas (< 5 cm in diameter) can be managed conservatively, whereas the literature is inconclusive regarding the benefits of conservative treatment versus surgical intervention for larger hematomas. Conservative management of larger hematomas has been associated with longer stays in the hospital, an increased need for antibiotics and blood transfusion, and greater subsequent operative intervention [7]. A hematoma that expands acutely is unlikely to settle with conservative measures.
While there may be pressure to intervene in cases where the paravaginal hematoma is huge and causes significant pain or severe postpartum hemorrhage, intervention may present its challenges and risks. Interventional radiology techniques are not widely available and only useful in cases where bleeding is persistent and difficult access anticipated as in cases of retroperitoneal hematoma. Where interventional radiology technique is considered, the patient must be hemodynamically stable. Surgery carries the risk of infection, risk of general or spinal anesthetic, and further hemorrhage, particularly if the hematoma has a tamponade effect on itself (decompression may perpetuate the hemorrhage). Surgery may also present technical challenges in accessing and closing the remaining potential space [8].
The successful conservative management of the cases presented in this report suggests that factors other than the absolute size of hematoma can be considered when recommending a management option.
The components of conservative management will include adequate monitoring, pain control, infection prevention, and blood transfusion if necessary. Strategies such as vaginal packing, application of ice packs if there is an extension to the vulva, use of tranexamic acid (an antifibrinolytic agent), etc., can also be used. An initial admission for close monitoring, e.g., in HDU, is essential as continuous monitoring of observations will help detect deteriorating patients who will benefit from other forms of active management. The cardiovascular changes that occur after delivery may mask significant blood loss, and the earliest signs of deterioration may be signs of decreased end-organ perfusion such as lethargy and decreased urinary output. Blood should be grouped and crossmatched, while serial monitoring of blood count and clotting profile should be instituted. Blood collection is a veritable tool for infection, and as such, antibiotics should be commenced to prevent an abscess from forming. The presence of infection will also add to the morbidity in these patients and must therefore be prevented at all costs.
The use of serial imaging may also be considered, particularly the use of bedside USS if the skill is available. In addition, a CT scan or MRI scan may be arranged later to check the resolution of hematoma. This can be scheduled to coincide with the post-natal visit, where an experienced obstetrician can discuss further debriefing, assessment of wellbeing, and plans for future pregnancy.
Conclusion
Genital tract hematomas are uncommon, and diagnosis delays can cause increased morbidity. However, the conservative approach can be used to manage large vaginal hematomas in carefully selected patients.
Key Messages
- Spontaneous vaginal hematoma can occur after vaginal delivery in the absence of episiotomy or any bleeding lacerations.
- Perineal pain out of proportion to obvious trauma should prompt a review for possible vaginal hematoma.
- Bedside USS may have a role in the initial diagnosis and management of large vaginal hematomas; ultimately, the gold standard for diagnosis is a CT scan with contrast or MRI scan.
- The size of the hematoma should not be the sole criteria in determining the management option.
- The patient’s cardiovascular status and absence of active bleeding on imaging are favorable factors for successful conservative management of large puerperal hematomas.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Saleem Z, Rydhstrom H. Vaginal hematomas during parturition: a population-based study. Acta Obstet Gynecol Scand. 2004;83(6):560–562.
- Villella J, Garry D, Levine G, Glanz S, Figueroa R, Maulik D. Postpartum angiographic embolization for vulvovaginal hematoma. A report of two cases. J Reprod Med. 2001;46(1):65–67.
- William S, Danendran K. Large concealed paravaginal haematoma: A case report of an occult postpartum haemorrhage. Case Reports in Women’s Health. 2021;30:e00311.
- Roman AS. Management of hematomas incurred as a result of obstetrics delivery [Internet]. Waltham, MA: Up To Date, Inc; 2021.
- Jain KA, Olcott EW. Magnetic Resonance imaging of postpartum pelvic hematomas: early experience in diagnosis and treatment planning. Magn Reson Imaging. 1999;17(7):973–977.
- Po LK, Simons ME, Levinsky ES. Concealed postpartum hemorrhage treated with transcatheter arterial embolization. Obstet Gynecol. 2012;120(2 Pt 2):461–464.
- Bellussi F, Cataneo I, Dodaro MG, Youssef A, Salsi G, Pilu G. The use of ultrasound in the evaluation of postpartum paravaginal hematomas. Am J Obstet Gynecol MFM. 2019;1(1):82–88.
- Mawhinney S, Holman R. Puerperal genital haematoma: a commonly missed diagnosis. Obstet Gynaecol. 2007;9(3):195–200.
Keywords
Hematoma; Ultrasound scan; Bleeding lacerations
Cite this article
Sanusi HA, Das S, Khan K. Conservative management of large spontaneous vaginal hematoma in the puerperium. Clin Case Rep J. 2022;3(2):1–5.
Copyright
© 2022 Sanusi HA. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).