Bioethics in the Care of Adolescents with Caudal Regression Syndrome - Case Report
* Correia IC;
Batista KT;
Garrafa V;
-
* Correia IC: Nurse in the Sarah Network of Hospitals, Bioethics Postgraduate Program of the University of Brasilia, Brasilia.
-
Batista KT: Plastic Surgeon in the Sarah Network of Hospitals, Bioethics Post-graduation Program of the University of Brasilia, Brasilia.
-
Garrafa V: Chairman of Unesco Chair, Bioethics of the University of Brasilia, Brasilia.
-
Aug 30, 2020 |
-
Volume: 1 |
-
Issue: 5 |
-
Views: 3564 |
-
Downloads: 2541 |
Abstract
Publications on Caudal Regression Syndrome (CRS) have preferentially addressed the diagnosis and treatment of such cases. There has been little discussion about related bioethical dilemmas.
Objective: To analyze ethical conflicts relating to adolescents with CRS.
Method: This was a case study on a patient with this rare disease who received a diagnosis of the neurogenic bladder during childhood but refused to undergo the invasive procedures proposed by the rehabilitation team. The discussion had as reference the principlist bioethics and the ethics of care.
Results: Upon reaching adolescence, the patient perceived the need for urinary continence and tried to face the challenge. A bioethical analysis of the dilemmas that he and the rehabilitation team faced is presented and discussed, along with the benefits of building respect for adolescent autonomy.
Final remarks: It was observed that the adolescent’s participation in the decision-making process made it possible to respect his autonomy without damaging the care provided.
Introduction
Caudal Regression Syndrome (CRS) is a rare malformation condition first described by Bernard Duhamel in 1960 as a spectrum of congenital malformations of the cardiovascular, urogenital, and sacral lumbosacral and lower extremity systems [1]. The higher the degree of agenesis is, the greater the neurological impairment will be. The structural defects seen within CRS include incomplete development of the sacrum and lumbar vertebrae; absence of the sacral body causing flattening of the buttocks; shortening of the intergluteal cleft and buttock depression; rupture of the distal spinal cord with neurological involvement ranging from urinary or fecal incontinence to complete neurological injury; and marked decrease in growth of the caudal region resulting from decreased leg movements secondary to neurological involvement.
Occasional abnormalities include renal agenesis, imperforate anus, microcephaly, other spinal malformations, spina bifida, and meningocele. The prognosis depends on the severity of the defect; severe cases are usually associated with heart, kidney and respiratory problems responsible for neonatal death. The treatment consists of observing and controlling possible cardiac, renal, and orthopedic problems and rehabilitation [1–6]. Urinary bladder training forms part of the rehabilitation program. It consists of developing the ability to maintain urinary bladder capacity, emptying the bladder through intermittent catheterization of the organ, and acquiring sufficient control to avoid urinary incontinence. The earlier that this training is started, the more satisfactory the results will be [7].
CRS has an incidence of one to five cases per 5000 births, and 16% of the cases occur within diabetes mellitus or gestational diabetes. However, only 1% of women have diabetes. CRS is a consequence of an embryological defect in the mid-posterior axial mesoderm of obscure etiology, which results in the induction of the syndrome before the fourth gestational week [1–3]. It has been discussed that the possible causes are maternal diabetes, teratogenic genetic predisposition, the interaction between environmental and genetic factors, and low vascular perfusion. Notably, CRS occurs most frequently in infants from diabetic mothers: the risk in such cases reaches around one in 350, i.e., a 300-fold higher incidence than in the general population [1–3].
Bioethics emerged in the early 1970s, both as a response seeking ethical control over the accelerated techno-scientific advances that were witnessed within the field of biomedicine at that time (transplantations, new reproductive technologies, etc.) and as a means of facing up to the abuses that were being committed at that time within the field of clinical trials involving humans, especially in the United States [8]. Although in its early days, bioethics had broad epistemological connotations that ranged from daily moral conflicts to planetary ethical issues, its foundations became redirected after a few years, almost exclusively towards studying the relationships between healthcare professionals and their patients and between researchers and pharmaceutical companies and their clinical research subjects [8].
In this context, the book The Principles of Biomedical Ethics was written by Tom Beauchamp and James Childress. This book still forms a reference point for this field today and is now in its seventh edition [9]. Over the years, these authors' proposals have garnered many followers and some criticisms. Nonetheless, their book is internationally recognized as defining "Principlism", based on four principles that are presumed to be universal: respect for autonomy, beneficence, non-maleficence, and justice.
The popularity of principlism has become so high among bioethics scholars that many followers of the discipline confuse it with bioethics itself. However, while on the one hand, researchers who are critical of the subject have praised the practical applicability of using these four principles for resolving ethical conflicts within biomedicine. These researchers have, on the other, and with greater emphasis, come to criticize the limitations of principlism, in the light of ethical macro-problems and the need to resolve specific moral issues that involve social matters within the daily routine of clinics, wards, and hospitals [8]. Therefore, at the same time that the so-called "four principles theory" can assist in resolving most of the issues arising from conflicts that healthcare professionals and researchers/sponsors have concerning patients, it proves to be insufficient to face individual, specific situations, such as the case in the study presented here.
Thus, it becomes opportune to consider the importance of so-called "ethics of care", which is a concept widely used in the field of nursing that encompasses preservation, maintenance, support for, and taking care of the "other" person, i.e., the patient. Among the various meanings of care, it implies helping others, promoting their wellbeing and preventing them from suffering any harm [10].
In healthcare, and more specifically in the field relating to patient care, there is now growing awareness among professionals, mainly within nursing, of the need to gain improved technical and scientific knowledge, thereby increasing their level of responsibility and the quality of the assistance provided. These care practices and the "act of caring" itself, are closely influenced by the current biomedical hegemonic model, which still disregards inter-professional relationships in many professional training institutions.
In nursing practice, care-giving means assisting humans with their healthcare needs. When the practice of caring goes beyond a patient's decisions, and healthcare professionals assume what is best for this patient from their understanding, they are paternalistic [7], i.e., they are not considering that the limit of "doing good" (or providing beneficence) for the other person is his autonomy. One of the obstacles to autonomy, i.e., the ability to decide and choose what is best for oneself, is precisely paternalism. When professionals are motivated by the desire to protect the patient and provide the treatment they deem most convenient from their point of view; they end up considering themselves to be the most suitable people to make these decisions. In such cases, even if the motivation is for the patient's benefit, the limit of the patient's free will cannot be exceeded. Therefore, the principle of beneficence that generally rules medical practice often collides with the limit required to respect the patient's autonomy.
Hence, the present article aimed to present a case report to discuss the conflicts present in healthcare for adolescents with Caudal Regression Syndrome (CRS), a rare disease. This discussion is presented in the light of principlist clinical bioethics and nursing at its interface with care ethics, especially regarding non-adult patient's right to have their autonomy respected.
Case report
The case in question was of a 14-year-old male with caudal regression syndrome, paraparesis, foot cavity, neurogenic intestine and bladder, and a preserved upper urinary tract. The patient was thus at risk. This case was associated with Situs inversus totalis, a rare genetic inheritance that causes its carriers to present complete inversion of all thoracic and abdominal organs. The patient was born in the Federal District, Brazil, and was admitted to a two years rehabilitation program. He was escorted by his mother, a young woman who had had six children, among whom the first four died during the first year of life due to congenital malformations, the fifth was one healthy daughter, and the sixth was the patient whose study is presented here.
At two years of age, LS (fictitious initials for identifying the patient) was indicated to begin bladder re-education, with Clean Intermittent Catheterization (CIC) to empty the bladder at regular periods. However, at no time did he allow or collaborate with the procedure, or with hygiene measures for the genitalia, or even less, with the urethral probe's introduction. The interdisciplinary team (nursing, psychology, and pediatrics) made several attempts without success. LS said that it hurt when the probe was introduced and displayed panic, cried, and did not touch. During this time, he continued to present urinary incontinence, with urine loss into diapers. The team maintained longitudinal monitoring and performed tests to control renal function, to remain aware of any possible aggravation.
At the age of 14, the patient brought to the team a complaint relating to bladder continence. He expressed his desire to "be free from diapers", given that now, as a teenager, he was feeling socially uncomfortable with the situation. Therefore, LS was admitted to the orthopedics and rehabilitation unit in a specialized hospital to assess and train self-catheterization. During this hospitalization, it was observed that the adolescent presented calm and collaborative behavior. However, significant slowness in the maneuvers execution was observed, and constant mediation was required in order to finish them within the scheduled time. He underwent an intellectual evaluation using the Wechsler Intelligence Scale for Children [11], from which he presented a result classified as "lower average", with even lower performance on the processing speed scale (IVP = 74).
In the ward, LS agreed to start self-catheterization training and was excited, demonstrating knowledge about the technique and catheterization indication. When the training itself was started, he showed no difficulties organizing the material and performing intimate hygiene measures. However, he could not introduce the probe in the urethral meatus: he complained of extreme pain and presented tremors throughout his body, with tachycardia, intense sweating, muscle rigidity, tension, and panic. Nevertheless, even with all these symptoms, he was collaborative and wanted to continue the training; however, he could not insert the probe. Intervention by the psychiatry team was considered necessary. This began with the use of propranolol (a beta-blocker used as an adjuvant for treating anxiety) and clonazepam (a benzodiazepine that is used for controlling anxiety), and the symptoms consequently improved.
LS ended up learning the procedure, but with considerable slowness, taking from two to three hours in the bathroom to achieve the introduction of the bladder probe. This meant that the act had to be done in the patient's own time. Thus, the training was gradual, respecting the patient's progress. A referral nurse was made responsible for facilitating a bond with the patient and ensuring adherence, and a psychologist also had effective participation during the catheterizations. Several methods were used to help the patient relax and be comfortable, such as music, private bathroom and devices for positioning, and follow-up from nurses and psychologists for all the necessary time. Daily goals were set for each procedure, with the decreased time taken and increased numbers of Clean Intermittent Catheterization (CIC) procedures. The goal of four catheterizations per day was achieved, with a maximum time of 15 minutes each. After 15 days of training, the patient was discharged from the hospital with outpatient monitoring.
Caudal Regression Syndrome (CRS) in nursing practice: Urological treatment is necessary for most CRS patients since they have a neurogenic bladder. This means that the bladder presents abnormal functioning, which leads to urinary incontinence, sphincter failure, and renal impairment. Over recent decades, there has been significant progress in diagnosing and treating this condition, with more explicit concerns about the prognosis, patient's quality of life, and treatment. CIC was described in the 1970s and is still the treatment of choice in the situations studied here, and is used in association with anti-cholinergic medications for the neurogenic bladder. This procedure is indicated early in childhood and is maintained for life. For children, guidance is directed towards caregivers, especially to family members, to learn how to perform the procedure. Adolescents with a neurogenic bladder can be trained to perform bladder self-catheterization, which is fundamental for independence in activities of daily living [11–14].
Clean Intermittent Catheterization can be performed by the patient himself (self-catheterization), with assistance from the team or the caregiver. It is an effective and safe technique, in which sterile catheters are used, introduced into the urethral meatus for bladder emptying. This technique is used for the treatment and prevention of gall bladder-urinary complications resulting from the neurogenic bladder. Bladder retraining for children and adolescents is part of an individualized program, and the physical and emotional traits of the child and adolescent need to be considered [11–14].
Although bladder catheterization is considered a simple and easy-to-perform procedure, it is an invasive procedure that is directly linked to privacy and physical intimacy and taboos relating to the individual's sexuality. These issues should also be considered in the general context of the procedure since they represent important bioethical dilemmas in caring for adolescents' health [15].
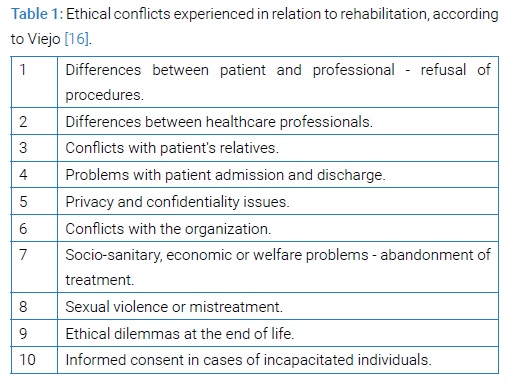
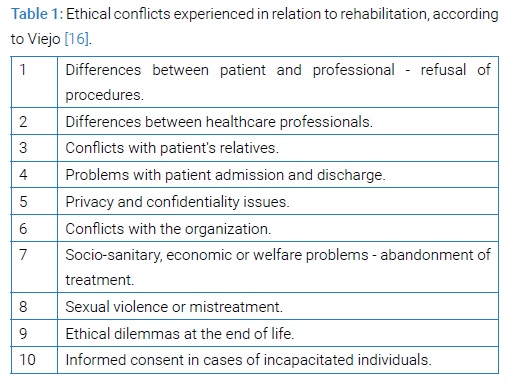
Other ethical conflicts [15] experienced in rehabilitation, which Viejo reported [16], are described in (Table 1).
Principlist bioethics: In the book Principles of Biomedical Ethics, the use of four principles that can be applied to analysis and management of bioethical dilemmas is accurately described [9]. These principles are the following: respect for autonomy, which represents the individual's freedom to decide; beneficence, which recommends that action should be taken to do good; non-maleficence, which advocates avoiding any type of intervention that harms other individuals; and justice, which generally requires development of fair and non-discriminatory practices [9].
Principlism was and still is widely used internationally. In Brazil, it is also present in several regulations, such as Resolution 466/2012 of the National Health Council, which regulates ethical control of health research. This hegemonic model of analyzing bioethical dilemmas has been widely used around the world since the 1980s and 1990s and has already been applied to different biomedical situations and conflicts in studies conducted in Brazil, which is why it was chosen as the reference point for this study [7,17,18].
As already mentioned, principlism has been criticized since its creation, mainly in relation to difficulty in using it to analyze moral macroproblems that are present in daily life, such as its vagueness or omission regarding the right of access to healthcare, among other situations. According to Paranhos [6], intervention bioethics (an epistemological current within bioethics, of Latin American origin) criticizes, for example, the feasibility of talking about relative and absolute principles, as proposed through the principlism of Beauchamp and Childress, along with the aim of basing principles on a presumed principle of common morality. In this article, in using principlism as a reference point for debate, we ask which principle should be favored for guiding professional conduct: beneficence or respect for autonomy? And why?
Currently, there is a predominant tendency in the international biomedical context to privilege the autonomy of the individual. To do so, it is necessary to understand its real meaning. Autonomy means self-government, self-determination and freedom to make decisions relating to one's life, health, physical-psychological integrity and social relations. It assumes the existence of options, freedom of choice and individuals capable of acting according to their own deliberations. Respect for autonomy is based on the principle of respect for human dignity and universal human rights, starting from the categorical historical imperative proposed by de Kant as early as the 18th century, which holds that the human being is an end in itself. Certain variables contribute to an individual becoming autonomous, such as biological, psychological and social conditions. However, there are certain transitory or permanent situations in which a person’s autonomy may become diminished, and it is then up to others who have a legal responsibility to make decisions. This is seen in relation to childhood and to some chronic and rare diseases in which the patient is in a transitory or permanent situation of vulnerability.
In the study by Albuquerque and Garrafa [18] on autonomy and underage individuals, specifically regarding consent within pediatrics, two terms stood out: capacity and competence to make decisions. In this regard, these authors drew attention to the need to distinguish "capacity", which is the psychological term that describes everyday mental abilities, from "competence", which refers to the legally established capacity to create a legal norm through and according to statements in this regard. It is worth highlighting that in the case reported here, the adolescent had a mild cognitive deficit and a very vulnerable social condition, a situation that required greater care both in conducting and in managing the explanations and teaching the maneuvers to be performed.
It should also be noted that there are still gaps in the legal arrangements that legitimize decisions made by children and adolescents about clinical procedures that are to be performed. These gaps open the way for paternalistic action by professionals and legal guardians, who often act based on their own perspective.
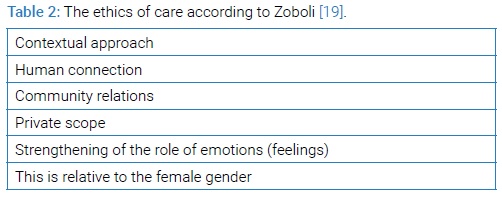
The ethics of care: The history of nursing in Brazil began in the 16th century and is still strongly influenced by Anna Nery who, like Florence Nightingale, applied the principles of "abc", i.e., knowledge of the meaning of sick human beings, understanding their behavior and awareness that care should be provided to people. This principle remains in practice within nursing. Selli [10], Zoboli [19,20], Gilligan [21] and other researchers have discussed and pondered the meaning of the expression "care" in nursing practice, summarized in (Table 2).
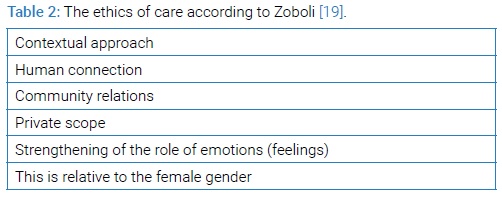
Care has several definitions and, in the current context, it relates to the notion of attention, consideration and respect for other people, which are important aspects of the bioethical analysis of dilemmas, especially within Latin American realities. According to Weil, as quoted by Zoboli [19] "(...) attention is an effort that consists of suspending one's own thought, leaving it neutral, empty and ready to receive the other person’s thoughts, as they are, in all their truth"(p. 24).
Nurses' training intrinsically includes the role of an educator and the coordination and implementation of the systematization of nursing care. Since the beginning of modern nursing, their educational role has been considered, such that curative purposes are broadened to include the roles of prevention and rehabilitation within nursing practice. The principles relating to rehabilitation are basic in the context of the care-giving interface. In this regard, efforts need to begin in direct contact with patients, and the essentially preventive-educational model through which the patient/care binomial is approached needs to be considered.
The interpersonal relationships based on attention and help, which caregivers are called upon to intervene in, are at the center of care. The relationship of respect and reliability built through the interpersonal relationship between the nurse and the patient to produce the proposed therapeutic result is considered an important point of debate. Nowadays, although "care" itself is not a direct part of the four principles proposed by Beauchamp and Childress in their principlist proposal for bioethics, the "care principle" is incorporated in the theory and practice of clinical bioethics.
Discussion
From principlism to care ethics: Ethical conflicts within rehabilitation assistance may occur between professionals and patients and their relatives, between patients and their relatives and/or caregivers, or between healthcare professionals in the same or different teams. This study describes dilemmas relating to differences registered between a patient, initially as a child and later as a teenager, and the healthcare professionals who assisted him. His initial refusal to cooperate with self-care treatment brings reflections on conflicts caused by difficulty, since childhood, in acceptance of elective treatment proposed for rehabilitation.
In this case report, there are three strands for reflection and bioethical analysis: autonomy in childhood, dilemmas specifically relating to rare diseases, and bioethical care. The first strand, concerning autonomy, i.e., .individuals' right and capacity to make their own decisions, was shown by the child's refusal to perform the procedure that had been proposed. This occurred in early childhood, which is an important stage for the construction of an individual's personality.
According to Weaver [22], refusal is still considered a complex and multidimensional construction, without any consensus among specialists. The International Society of Pediatric Oncology defines "refusal" as "a decision to avoid the recommended elective treatment", which differentiates it from "abandonment", based on the argument of "lack of mutual understanding" between families and medical professionals [22]. Abandonment of treatment is a more complex phenomenon and is related to psychosocial factors, with direct impacts on patients and family members and institutional and social repercussions.
The second strand related to the proposed procedure of intermittent bladder catheterization (IVC) for treating this rare pathological condition of caudal regression syndrome, and its impact on both the child and his caregiver. IVC plays an important role in neurogenic bladder care: it promotes improved quality of life and leads to lower mortality due to renal complications in spinal cord injury patients. However, it demands regularity, availability, discipline, and compliance, without which the patient may present adverse reactions in up to 56% of the cases. As also described by Lopes [12], we observed in our case that the patient refused to perform the procedure. Our patient's case was submitted to a team discussion in which the principle of respect for the patient's autonomy at its interface with the bioethics of care was considered. In this case, the difficulty in applying the principlism proposed by Beauchamp and Childress [8] was highlighted, because of doubts regarding which principle should be used: the principle of beneficence, which would naturally be the one that was most clinically appropriate; or the principle of respect for the patient's autonomy in his own decision not to accept the procedure? To what extent does autonomy prevail, especially concerning children and adolescents, over the beneficence recommended by the healthcare team? Thus, the classic dilemma was seen in this case: professional paternalism versus the patient's will.
It became clear that there was a bioethical dilemma around the use of the principle of beneficence. The rehabilitation team was concerned with the health and prevention of complications arising from the rare disease and the patient's wellbeing, knowing that the most effective treatment of choice would be gall bladder catheterization, which is already recommended worldwide. On the other hand, the context also demanded that the principle of non-maleficence should be considered as a historical principle within medical ethics: the Hippocratic principle of "primum non nocere", i.e., first, not harm. In this case, the patient's pain, fear, and trauma generated by the catheterization were preponderant, since these were the mandatory principles for the patient at that moment, such that he refused the proposed treatment.
How long does non-maleficence take precedence over beneficence? These dilemmas can be discussed with the patient's care in mind, according to the bioethics of care, to ensure the patient's wellbeing. Whenever clinical cases within the daily practice are analyzed, the application of clinical bioethics (i.e., dealing with identification, analysis, and resolution of problems or moral dilemmas that arise within patient's individual care) is an indispensable tool. Like in the present case, Gracia [23] made some observations regarding the evaluation of dilemmas within clinical ethics and stated that medical ethics should not begin with the establishment of major principles, but rather with studies on practical cases. Therefore, the starting point for every decision needs to be the clinical history, and, in this regard, clinical ethics cannot be understood as a mere application of general principles established through fundamental bioethics. Thus, this author pondered that bioethics had become a medical discipline, from analysis of clinical judgment's moral dimensions. For this reason, Gracia [23] took the view that analysis procedures should always start from a thorough study of clinical facts. This author elaborated on another proposal based on four premises: ontological, deontological, teleological, and moral justification, from which decision-making would be based on contrasting the conflicts of values that were clarified in each of the propositions.
Schramm [17] dealt with what this author called "difficult autonomy" or "fragile autonomy" and provided a general description of the private and collective application of autonomy. According to this author, autonomy is one of the basic principles of bioethics, which has historically been used with different technical meanings within the various currents of modern and contemporary ethics. However, and despite these differences, this author considered that it was legitimate to affirm that there would be a common denominator among such currents, consisting of, in some way, setting the principle of autonomy against the heteronomous and often paternalistic principle of beneficence. Thus beneficence can be seen as the way of solving problems of authority, power, obedience, and freedom through traditional means based on the patriarchal family structure, in which the father decides and makes all the choices, through applying the model of his relationship with his children, supposedly for the greater wellbeing of his protege.
The third strand specifically concerns care for patients with neurogenic bladder, as presented in this case report and, therefore, for patients with urinary incontinence, in which the situation is considered to be one of risk, since other complications may arise, such as vesicoureteral reflux, damage to the upper urinary system, infections, and renal failure. Faced with this complex situation, the indication for regular emptying of the bladder, with bladder catheterization or Clean Intermittent Catheterization, is considered the first choice for treating neurogenic bladder, since it is easy to perform, low cost and has good resolution. However, in the case of the present study, the patient initially refused any kind of manipulation and insertion of the probe because of complaints of pain and sensitivity, which made the introduction of the probe difficult. Several attempts were made by the rehabilitation team, using several strategies and teamwork, without success. In this regard, then, methodological use of bioethics of care became necessary. This had the aim of protecting the patient and promoting interpersonal relationships to maintaining confidence, with the particularities of the ethics of care described earlier.
Although the patient was a child, the rehabilitation team did not force him to undergo this procedure to avoid further trauma and thus further harm his physical and mental health conditions, while respecting his autonomy. The team chose to maintain follow-up until an appropriate time, in order to reach conclusions regarding what would be the best time to perform the proposed treatment. Only when the patient reached adolescence did he understand and participate effectively in the most appropriate clinical recommendation to improve his health.
References
- regressione caudale con assenza completa del rachide lombo-sacrale in figlio di donna diabetica presentazione di un caso. Min Ped. 1988;40:367–371.
- Stroustrup SA, Grable I, Levine D. Case 66: caudal regression syndrome in the fetus of a diabetic mother. Radiology. 2004;230(1):229–233.
- Schwartz Y, Williams TS, Roberts SD, Hellmann J, Shaul RZ. Adolescent decision-making in Canadian medical contexts: Integrating neuroscience and consent frameworks. Paediatr Child Health. 2018;23(6):374–376.
- Negrete LM, Chung M, Carr SR, Tung GA. In utero diagnosis of caudal regression syndrome. Radiol Case Rep. 2015;10(1):1049.
- Temizkan O, Abike F, Ayvacı H, Yilmaz A, Demirag E, Sanverdi I. Prenatal diagnosed caudal regression syndrome. Open J Obstet Gynecol. 2013;03(02):227–231.
- Paranhos FRL. Crítica à teoria da moralidade comum como fundamentação do principialismo [thesis] [Internet]. Brasilia: UNB;2015.
- Baptista MKS, Santos RM, Costa LMC, Macedo AC, Costa RLM. O poder na relação enfermeiro-paciente: revisão integrativa. Revista Bioética (Impr.). 2018;26(4):556–566.
- Garrafa V. Da bioética de princípios a uma bioética interventiva. Revista Bioética. 2005;13(1):125–134.
- Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th edition. New York: Oxford University Press (2013).
- Selli L. O cuidado no cotidiano da enfermagem: enfrentamentos e conquistas em relação a bioética e ética. Cadernos Centro Universitário São Camilo. 2000;6(2):75–81.
- Wechsler, D. Escala Wechsler de inteligência para crianças: WISC-IV. Manual Técnico. Tradução do manual original Maria de Lourdes Duprat. 4th edition. São Paulo: Casa do Psicólogo, 2013.
- Lopes MAL, Lima EDRP. Continuidade do Cateterismo Vesical Intermitente: pode o suporte social contribuir? Rev. Latino-Am. Enfermagem maio-jun. 2014;22(3):461–466.
- Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010;184(1):213–217.
- Gormley EA. Urologic complications of the neurogenic bladder. Urol Clin North Am. 2010;37(4):601–607.
- Almeida RA, Lins L, Rocha ML. Dilemas éticos y bioéticos en la atención de la salud del adolescente. Rev Bioet (Impr). 2015;23(2):325–336.
- Viejo MAG, Garrido AG, Soriano RF, Díaz AH, Magraner LM, Eizmendi AR. Mapa de conflictos éticos intrahospitalarios en rehabilitación. Rehabilitación. 2010;44(1):16–24.
- Schramm RF. Autonomia difícil. Bioética. 1998;6(1):27–37.
- Albuquerque R, Garrafa V. Autonomia e indivíduos sem a capacidade para consentir: o caso dos menores de idade. Rev. bioét. (Impr.). 2016;24(3):452–458.
- Zoboli ELCP. A redescoberta da ética do cuidado: o foco e a ênfase nas relações. Rev Esc Enferm USP. 2004;38(1):21–27.
- Zoboli ELCP, Sartorio NA. Bioetica e enfermagem: uma interface no cuidado. O Mundo da Saúde. 2006;30(3):382–397.
- Gilligan C. In a different voice: Psychological theory and women’s development. Cambridge, MA, US: Harvard University Press; 1982.
- Weaver MS, Howard SC, Lam CG. Defining and distinguishing treatment abandonment in patients with cancer. J Pediatr Hematol Oncol. 2015;37(4):252–256.
- Gracia D. Procedimientos de decisión en ética clínica. Madrid: Eudema, 1991.
Keywords
Caudal regression syndrome; Bioethics; Autonomy; Beneficence; Care
Cite this article
Correia IC, Batista KT, Garrafa V. Bioethics in the care of adolescents with caudal regression syndrome - Case Report. Clin Case Rep J. 2020;1(5):1–7.
Copyright
© 2020 Correia IC. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).