A Case of Protracted Resuscitation and Fibrinolysis During Cardiac Arrest in Emergency Room Due to St-Elevation Myocardial Infarction
Capolino A;
Cesaro C;
De Marco F;
* Gabriele Valli;
Verrelli C;
Dionisi S;
Ruggieri MP;
-
Capolino A: Sapienza, University of Rome, Rome, Italy.
-
Cesaro C: Sapienza, University of Rome, Rome, Italy.
-
De Marco F: Department of Emergency, San Giovanni Addolorata Hospital, Rome, Italy.
-
* Gabriele Valli: Department of Emergency, San Giovanni Addolorata Hospital, Rome, Italy.
-
Verrelli C: Department of Emergency, San Giovanni Addolorata Hospital, Rome, Italy.
-
Dionisi S: Department of Emergency, San Giovanni Addolorata Hospital, Rome, Italy.
-
Ruggieri MP: Department of Emergency, San Giovanni Addolorata Hospital, Rome, Italy.
-
Feb 09, 2021 |
-
Volume: 2 |
-
Issue: 1 |
-
Views: 4691 |
-
Downloads: 2564 |
Abstract
Background: Different therapies have been studied in patients with cardiac arrest due to ST-Elevation Myocardial Infarction (STEMI). However, none of the anti-arrhythmic or vasopressor medications have consistently been shown to improve these patients’ survival or neurological outcomes. Recent studies show that administration of fibrinolytic drugs during cardiac arrest may improve survival outcomes and neurological status.
Case presentation: We report the case of a 53-year-old woman who presented with an acute inferior STEMI, which occurred a few hours after chest pain onset. Soon after Emergency Department admission, she went into cardiac arrest. She was successfully treated with Advanced Cardiopulmonary Resuscitation (ACLS) according to American Heart Association’s guidelines for advanced cardiovascular life support for 65 minutes. Fibrinolysis was performed 10 minutes after cardiac arrest onset, and the patient underwent Percutaneous Coronary Intervention (PCI) three hours after Return of Spontaneous Circulation (ROSC). Neurological outcome post-cardiac arrest, assessed by Glasgow Outcome Scale (GOS), was favorable (GOS 15).
Conclusion: Our case report shows that in cardiac arrest due to STEMI, the immediate performance of the ACLS algorithm and fibrinolysis could substantially influence survival and neurological outcome, even if guidelines do not yet recommend this practice.
Introduction
Cardiac arrest represents the most severe adverse event that may occur during hospitalization. Survival rates after adult In-Hospital Cardiac Arrest (IHCA) does not exceed 20% in most studies [1]. No anti-arrhythmic or vasopressor medications have consistently been shown to improve survival or neurological outcomes.
Older studies showed that administration of fibrinolytic drugs during an out-of-hospital cardiac arrest could improve survival outcomes and neurological status in patients with a high probability of myocardial infarction [2,3], whereas fibrinolysis in IHCA is generally not considered preferring direct access to cath-lab [4].
In the TROICA study [5], fibrinolysis with tenecteplase during ACLS in Out-of-Hospital Cardiac Arrest (OHCA), due to Pulmonary Embolism (PE) or Acute Coronary Syndrome (ACS), did not improve patients outcomes comparing with placebo. Nevertheless, more recent studies have shown a significantly higher 30-day survival in patients admitted to hospital after an OHCA due to PE and who underwent thrombolysis during Cardiopulmonary Resuscitation (CPR) compared with patients who did not [6,7].
We present a case of a woman suffering from refractory IHCA in an emergency-care setting who underwent approximately 65 minutes of CPR and treated with fibrinolytic, achieving a Return of Spontaneous Circulation (ROSC) and an excellent neurological outcome.
Case Presentation
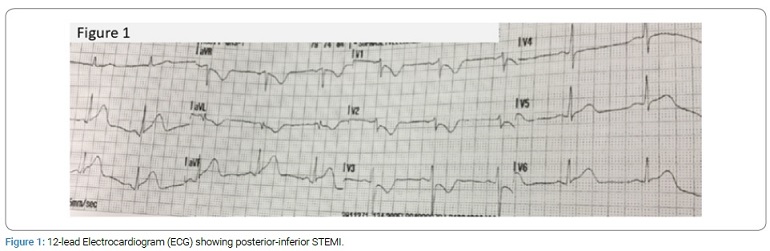
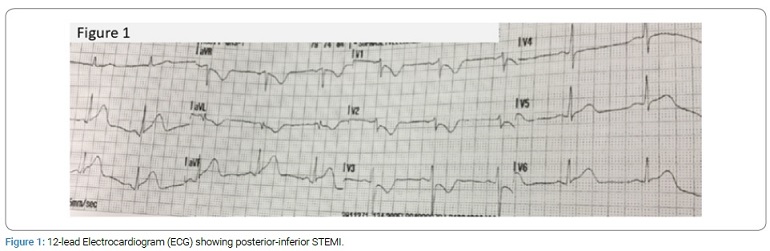
A 53-year-old woman with a story of smoking, hypertension, elevated Body Mass Index (BMI), and a family history notable for ischemic heart disease developed persistent severe chest pain at rest. She was brought by ambulance directly to the emergency room. A 12-lead Electrocardiogram (ECG) was performed during transport, showing posterior-inferior STEMI (Figure 1). A few minutes after arrival at the emergency department, the patient experienced ventricular tachycardia and cardiac arrest.
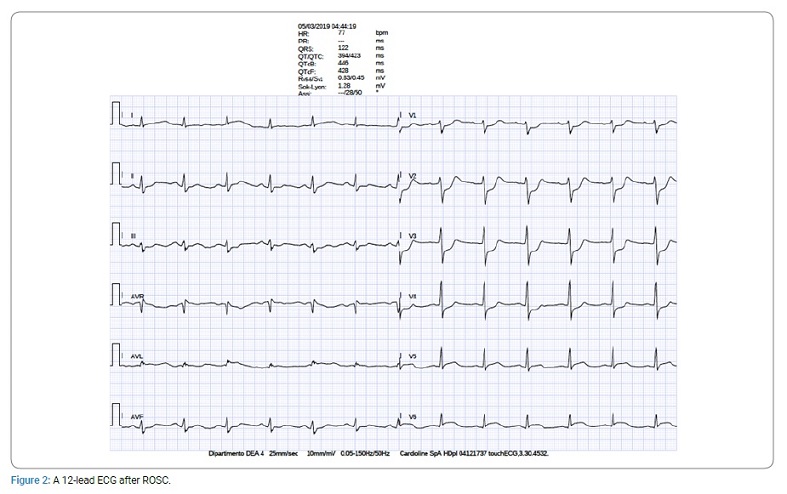
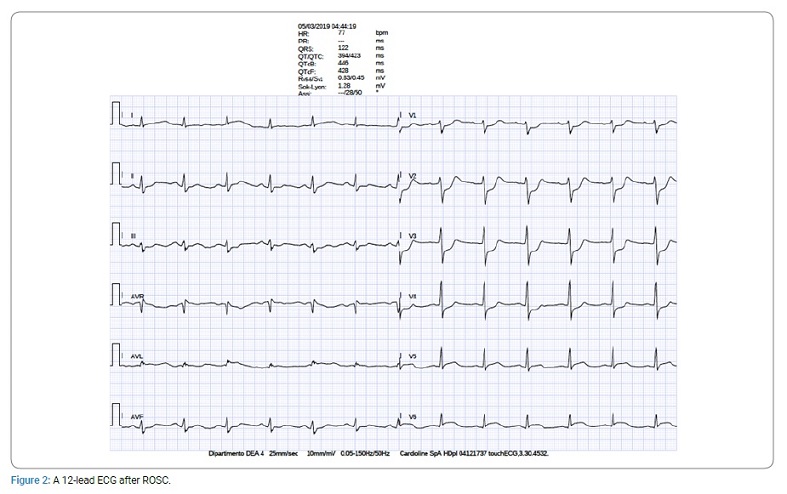
Subsequently, resuscitation was performed according to the American Heart Association/American College of Cardiology advanced cardiac life support guidelines for shockable rhythm until the return of ROSC [8], which happened 65 minutes later. After 10 minutes of resuscitation attempts, endotracheal intubation and fibrinolysis with Alteplase were performed (bolus of 15 mg followed by infusion of 0.75 mg/kg over 30 minutes). Soon after ROSC, intravenous acetylsalicylic acid (300 mg) and subcutaneous heparin (4000 UI) were administered. Sixty minutes after ROSC, the patient showed worsening of her hemodynamic status (Systolic Blood Pressure (SBP) 70 mmHg, Diastolic Blood Pressure (DBP) 40 mmHg, Heart Rate (HR) 110 bpm) and ECG changes (Figure 2).
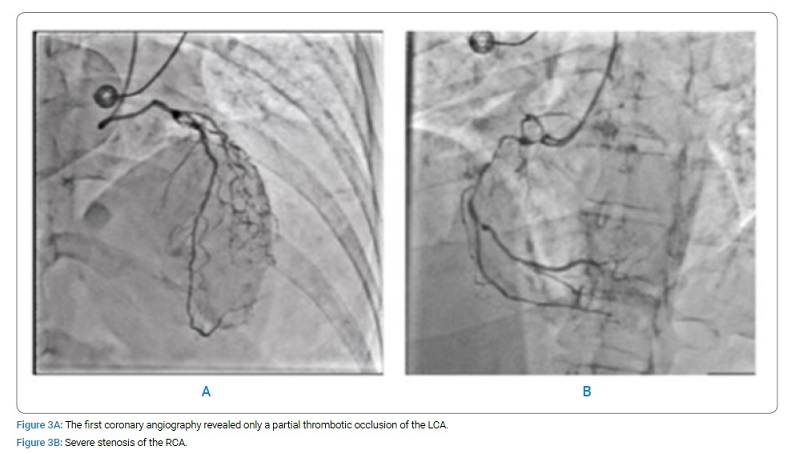
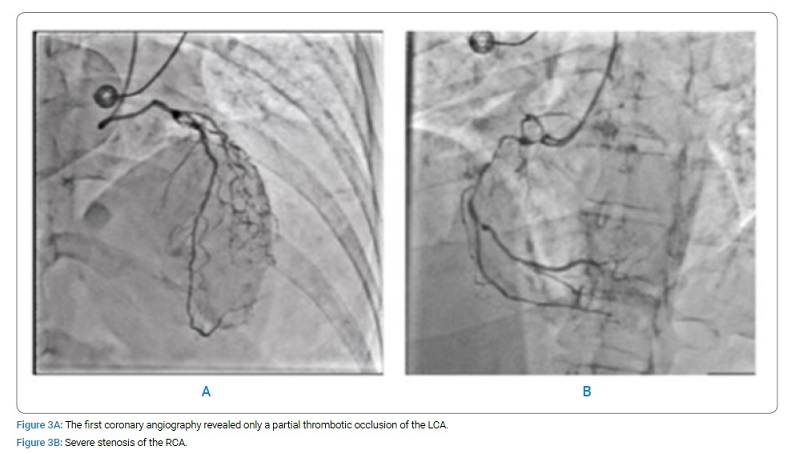
Therefore she was transferred to the catheterization laboratory for coronary angiography performed approximately after 3 hours for hemodynamic instability and severe risk of bleeding after administration of a fibrinolytic drug, although Alteplase has a short half-life (Figure 3A). The first coronary angiography revealed only a partial thrombotic occlusion of the left Coronary Artery LCA (A), while the Right Coronary Artery (RCA) showed severe stenosis (Figure 3B). The not complete occlusion of LCA was probably the effect of Alteplase.
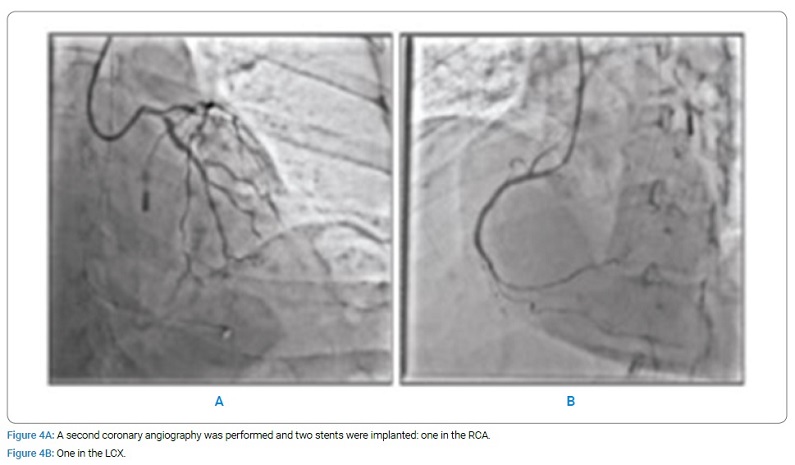
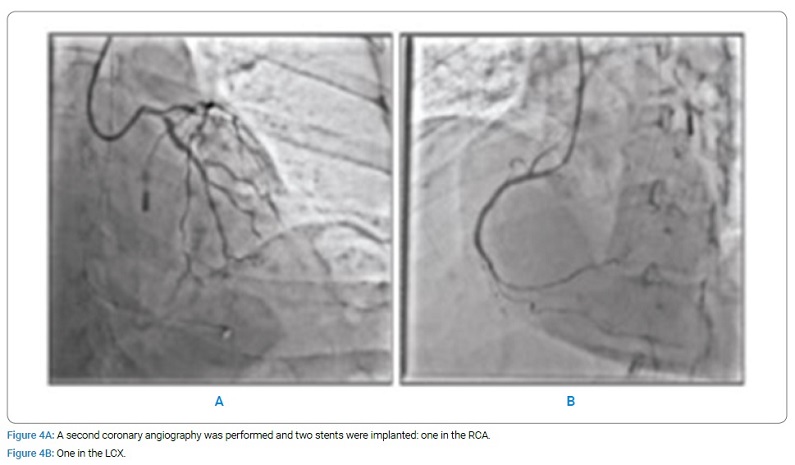
After 24 hours, a second coronary angiography was performed, and two stents were implanted: one in the RCA (Figure 4A) and one in the left circumflex artery (Figure 4B). After the procedure, the patient was transferred to the cardiological intensive care unit in stable clinical conditions where she underwent therapeutic hypothermia, with a good neurological outcome (GCS 15).
Discussion
Mortality rates in patients suffering from cardiac arrest due to STEMI are high, and the chance of survival without neurological sequelae decreases dramatically with every passing minute [2,9].
Our case report demonstrates that even after a cardiac arrest with prolonged time until ROSC, more than 1 hour in this specific case, survival with a favorable neurological outcome is possible. European Society of Cardiology guidelines for the management of acute myocardial infarction 4, do not recommend fibrinolysis during ACLS to treat cardiac arrest due to myocardial infarction [8].
In our case, the quality of CPR and the use of fibrinolysis, even if not recommended by current guidelines, substantially made a difference for the neurological outcome.
Despite prolong ACLS and a delay of 65 min till ROSC, our patient showed a remarkably favorable neurological outcome during the clinical course.
During cardiac arrest, an etiologic diagnosis is crucial to choose the best therapeutic strategy. In our case, clinical symptoms and electrocardiographic signs of cardiac ischemia during the pre-arrest phase influenced the in-arrest decision-making process. While the rhythm was still interpreted as shockable and RCP/Drug therapy was delivered, fibrinolysis treatment was also considered and therefore applied. It is plausible to assess that the outcome of the patient was influenced by therapy.
Why should a physician be aware of this?
The use of fibrinolysis during cardiac arrest due to myocardial infarction is a controversial issue: current guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation do not recommend fibrinolytic therapy during refractory cardiac arrest due to the bleeding risk and its low level of effectiveness. On the other hand, these guidelines are based on out of hospital studies, and most of them concern shockable rhythms [4]. Two retrospective studies [2,3] analyzing survival ratio and neurological outcome of patients who had undergone thrombolysis during CPR, have been shown encouraging results. These contradictory results may be due to selection bias: in the out-of-hospital studies, there were a high proportion of both relatively young patients and witnessed cardiac arrests; while, a high proportion of patients with VF doubtlessly contributed to the result of a favorable outcome in the retrospective studies.
In conclusion, even if it is necessary to deepen our knowledge of this issue, recent studies are reviewing the role of fibrinolysis in cardiac arrest, but further investigations are needed.
Availability of Data and Materials
The patient data and figures of this manuscript is available from the authors on request.
Ethics Approval and Consent to Participate
The patient’s written informed consent was obtained for the publication of the case report concerning herself.
Consent for Publication
The patient gave consent to her data being published in the Journal.
Competing Interests
The authors declare that they have no competing interests.
References
- Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE. One-year survival after in-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2018;132:90–100.
- Arntz HR, Wenzel V, Dissmann R, Marschalk A, Breckwoldt J, Müller D. Out-of-hospital thrombolysis during cardiopulmonary resuscitation in patients with high likelihood of ST-elevation myocardial infarction. Resuscitation. 2008;76(2):180–184.
- Renard A, Verret C, Jost D, Meynard JB, Tricehreau J, Hersan O, et al. Impact of fibrinolysis on immediate prognosis of patients with out-of-hospital cardiac arrest. J Thromb Thrombolysis. 2011;32(4):405–409.
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177.
- Böttiger BW, Arntz HR, Chamberlain DA, Bluhmki E, Belmans A, Danays T, et al. TROICA Trial Investigators, European Resuscitation Council Study Group. Thrombolysis during resuscitation for out of-hospital cardiac arrest. N Engl J Med. 2008;359(25):2651–2662.
- Javaudin F, Lascarrou JB, Le Bastard Q, Bourry Q, Latour C, De Carvalho H, et al. Thrombolysis during resuscitation for out-of-hospital cardiac arrest caused by pulmonary embolism increases 30-day survival: findings from the french national cardiac arrest registry. Chest. 2019;156(6):1167–1175.
- Böttiger BW, Wetsch WA. Pulmonary embolism cardiac arrest: thrombolysis during cardiopulmonary resuscitation and improved survival. Chest. 2019;156(6):1035–1036.
- Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Adult advanced cardiovascular life support: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S444–S464.
- Karam N, Bataille S, Marijon E, Tafflet M, Benamer H, Caussin C, et al. Incidence, mortality, and outcome-predictors of sudden cardiac arrest complicating myocardial infarction prior to hospital admission. Circ Cardiovasc Interv. 2019;12(1):e007081.
Keywords
Fibrinolysis; Stemi; Prolonged resuscitation; Cardiac arrest; Percutaneous coronary intervention
Cite this article
Capolino A, Cesaro C, De Marco F, Valli G, Verrelli C, Dionisi S, et al. A case of protracted resuscitation and fibrinolysis during cardiac arrest in emergency room due to st-elevation myocardial infarction. Clin Case Rep J. 2021;2(1):1–5.
Copyright
© 2021 Gabriele Valli. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).