Abstract
A 65-year-old man with a VVI pacemaker and persistent Ventricular Tachycardia (VT) was referred to catheter ablation. The successful ablation site was 5 mm under the left pulmonary cuspid valve and 2 mm from the Right Ventricular (RV) electrode. No significant change on pacing thresholds, perception thresholds, and pacing impedance of pacemaker electrode before and after VT ablation.
Introduction
Dual-chamber or dual-ventricular implantable electronic devices are usually set to atrial tracking mode (typically DDD or DDD-R). In this mode, ventricular synchronization and pacemaker-mediated tachycardia are common, and the tachycardia is generated solely by inappropriate rapid pacing frequencies driven by continuous ventricular retrograde conduction [1]. Besides, acute myocardial damage, and electrical irritation shortly after pacemaker implantation may also induce VT [2]. Here; we report a patient with pacemaker electrode position-related Ventricular Tachycardia (VT) other than pacemaker-mediated tachycardia.
Case Presentation
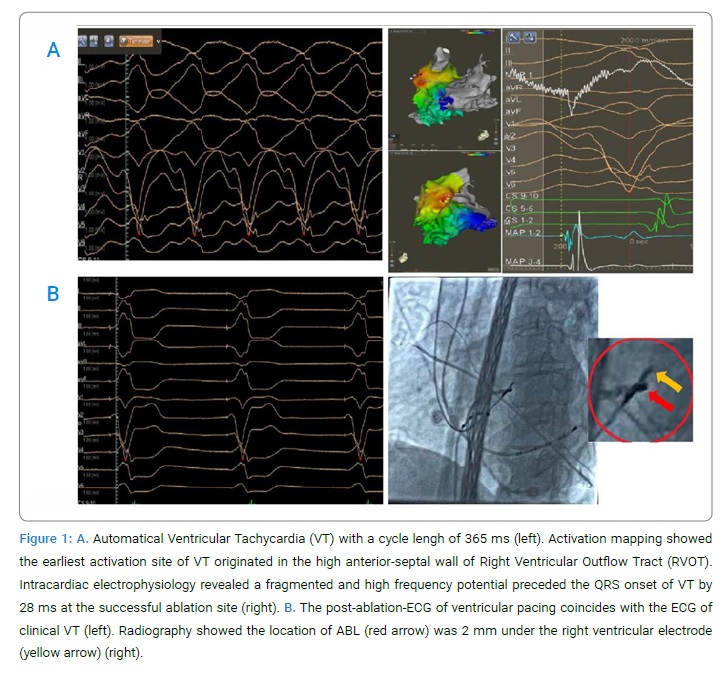
A 65-year-old man with persistent Ventricular Tachycardia (VT) was referred to catheter ablation. He was diagnosed with paroxysmal atrial fibrillation and third-degree atrial-ventricular conduction block without any heart disease and then was planted a VVI pacemaker (St. Jude Medical, 5056) three years ago. There used to be frequent short episodes of VT after pacemaker implantation. The morphology of clinical VT (Figure 1A) was the same as pacing ECG (Figure 1B).
The pacemaker was turned off right after cardioversion, but VT automatically emerges again. Many drugs, including amiodarone and lidocaine, did not slow the rate of VT except esmolol. VT could only be temporally terminated by cardioversion. The ablation procedure was performed under the guidance of the CARTO® 3 mapping system. Persistent VT was identified and mapped throughout the procedure using activation mapping and voltage mapping by PENTARAY® catheter and THERMOCOOL® SMARTTOUCH® (ST) catheter. Activation mapping by PENTARAY® catheter showed the earliest activation site of VT originated in the high anterior-septal wall of the Right Ventricular Outflow Tract (RVOT). Voltage mapping revealed no low-voltage regions in that site (Figure 1A). When we manipulated the ST catheter to the earliest activation site, a ventricular potential earlier than the onset of QRS by 28 ms could be recorded.
Ablation (30 W, 45 s) eliminated the VT successfully. No ventricular arrhythmia can be induced by isoproterenol infusion (10 ug/min). Measurements from CARTO® and radiography showed the successful ablation site was 5 mm under the left pulmonary cuspid valve and 2 mm from the Right Ventricular (RV) electrode (Figure 1B). There were no intra- or post-procedural complications. Aspirin was used for one month. This patient has been followed up for three months without recurrence of VT. There was no significant change in pacing thresholds, perception thresholds, and pacing impedance of pacemaker electrodes before and after VT ablation (1.0 v vs. 1.0 v, 7.5 mV vs. 7.2 mV, and 392 Ω vs. 370 Ω respectively).
Discussion
To our knowledge, this is the first report of VT related to the implantation position of an electrode of a VVI pacemaker. Dual-chamber or dual-ventricular implantable electronic devices are usually set to atrial tracking mode (typically DDD or DDD-R) to keep the Atrioventricular (AV) synchronized. In this mode, ventricular synchronization and pacemaker-mediated tachycardia are common, and the tachycardia is generated solely by inappropriate rapid pacing frequencies driven by continuous ventricular retrograde conduction [1]. Besides, acute myocardial damage, and electrical irritation shortly after pacemaker implantation may also induce VT [2].
In our patient, the pacemaker was a single-chamber device with VVI mode, and the AV node of the patient has no antegrade and retrograde conduction. The electrodeposition was located at the very high anterior-septal wall of RVOT under the pulmonary valve. Myocardial sleeves extended into the pulmonary artery in 74% of patients, and there was a higher prevalence of intercuspal extensions than the aortic valve [3]. These anatomical features are the basis for VT most commonly occurring in the RVOT right under the pulmonary valve. For the following reasons: there used to be frequent short episodes of VT after pacemaker implantation; the post-ablation-ECG of ventricular pacing coincides with the clinical VT; the electrodeposition was located at the very high anterior-septal wall of RVOT; VT can be sustained although the pacemaker was turned off, we suspect that this VT may be related to long-term electrical stimulation after electrode implantation which could induce the accelerated automaticity of the local myocardium.
Declarations
Patient consent: The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient provided her consent for the images and other clinical information to be reported in the journal. The patient understands that her names and initials will not be published and efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
The authors claim no conflicts of interest.
Keywords
Ventricular tachycardia; Pacemaker electrode position; Ablation
Cite this article
Li JY, Yang YY, Lv C, Jiang JB. Ablation a rare ventricular tachycardia related to pacemaker electrode position. Clin Case Rep J. 2021;2(2):1–3.
Copyright
© 2021 Jing-bo Jiang. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).