Abstract
Aggressive and avoidant behavior are risk factors for disruption of necessary medical therapy and challenge for medical staff. This case report offers a classification of stress reactions in very young children during oncological medical treatment. Moreover, it illustrates a best-practice case of interdisciplinary treatment to explain medical procedures and improve the compliance of young children with chronic illnesses and language barriers.
Introduction
A major psychology challenge in pediatric oncology is the age-adequate psychoeducation of children under the age of five. This age is characterized by magical thinking, associative logic, and concrete thought processes. Hence, verbalizing and discussing concepts of medical procedures and fears and anxieties is limited and can impact emotional wellbeing or, instead, increase problematic behavior [1].
Consequently, age-appropriate methods to express and regulate emotions are required [2]. The use of various teaching tools to explain medical procedures and improve compliance is part of the standard psychosocial care. Teaching dolls, preparation books, and interactive methods of medical play are used as an important approach to address these issues [3]. Role-play in particular influences the development of a child in a positive manner [4] and is used in medical settings as a preventive factor in coping with stressful and painful medical treatments and procedures, but also in adapting to chronic illness and preparing for hospitalization [3,5]. Although role-play is established in psychosocial interventions in the healthcare system, few studies have varied results [1].
This case of a 3.5-year-old boy from Romania treated in Austria captures the challenges in treating very young children with chronic illnesses and language barriers. Furthermore, it shows the importance of considering psychosocial factors and stress reactions to initiate targeted psychological interventions to improve compliance and support medical treatment success.
Case Presentation
At the age of 2.5 years, the boy was diagnosed with an embryonal tumor in the posterior fossa. After resection, the boy was treated with conventional chemotherapy in Romania. Ten months after the initial diagnosis, a recurrence was detected on an MRI of the brain. The boy and his mother moved to Austria for treatment of the recurrence. The father and the older brother remained in Romania.
MRI brain upon arrival confirmed massive tumor progression within only four weeks leading to obstructive hydrocephalus.
Antiangiogenic treatment: According to the MEMMAT approach [5] consisting of a five-drug oral regimen augmented with intravenous bevacizumab and additional intraventricular chemotherapy via an Ommaya reservoir was initiated. In addition, craniospinal radiotherapy for six weeks was administered in sedation concomitant to antiangiogenic treatment.
Interdisciplinary treatment: In the Paediatric Neuro-Oncology Unit is organized as an integrated care system [6]. Besides medical treatment, the psychosocial team supported the boy and his mother from the start of the boy’s tumor treatment in Vienna. Communication was possible in English with the mother. The boy only spoke Romanian and could not talk with medical and psychosocial staff.
During the first weeks, the psychological condition of the boy deteriorated and resulted in increasingly aggressive behavior against his mother (biting, beating, throwing objects). Moreover, as a typical age-appropriate response, the boy showed outright denial against the medical treatments, which resulted in the refusal of drug intake. Furthermore, it became evident that he was neither informed about treatment procedures nor the reason for its necessity. The mother had never explained or given any reasons for the hospital stays (telling the boy he was there “to feel even better”) and avoided talking about medical procedures. The boy experienced medical procedures (e.g., blood sampling, drug intake) as frightening and traumatic. Because of the language barrier, supportive medical advice (usually conducted before, during, and after medical treatment) could not be provided. The regular psychosocial assessment of stressors and resources followed the psychosocial standards in pediatric oncology [7]. Additional to medical and psychosocial staff reports, the regular psychosocial assessment [8] included a systematic anamnesis, standardized observation (behavior and the mother-child interaction), and a parental questionnaire [9]. As expected, both mother and child seemed to be socially isolated. Age-appropriate activities were considered below average. Concerning the boy’s aggressive behavior and inconsistent parenting style were observed.
Psychological intervention: We considered an inherent part of regulating behavior, improving compliance, and enabling indispensable medical treatment. All interventions were carried out by a clinical psychologist specializing in pediatric psycho-oncology.
The initial phase of the psychological treatment consisted of establishing a trusting relationship with the boy and his mother. Due to the high distress level, the mother agreed on the treatments in spite of her initial doubts on psychoeducation.
The treatment sessions included supportive therapy (strengthening parents’ confidence), promoting compliance during medical procedures (role-play, stress-relieving techniques, positive distraction), as well as medical play by offering playful and age-appropriate materials [2,3,10]. To demonstrate medical treatment, examination methods and various materials were used (anatomical teddy with doctor’s case, toy hospital, and hand puppet). The representation of medical procedures in a nonverbal way illustrates a standard in psychoeducation in young children, especially when considering the language barrier.
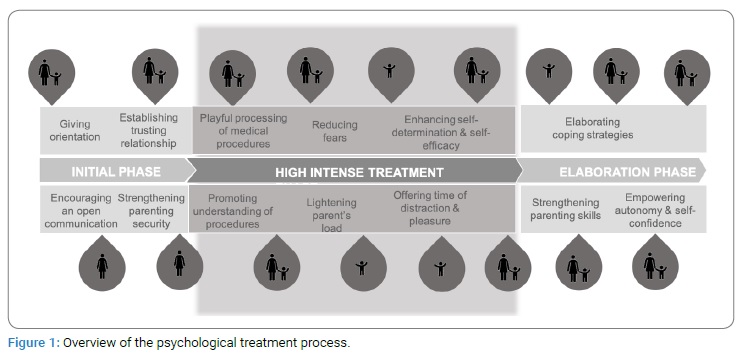
Additional nonverbal communication methods (eye contact, facial expressions, and gestures) elucidated the given information. The following sessions (about 2–3 times a week, 30 minutes–70 minutes) were clearly structured, starting the session with the boy choosing an object from a selection of different play tools on his own. This allowed him to experience a sense of control and self-efficacy. (Figure 1) gives an overview of the psychological treatment process.
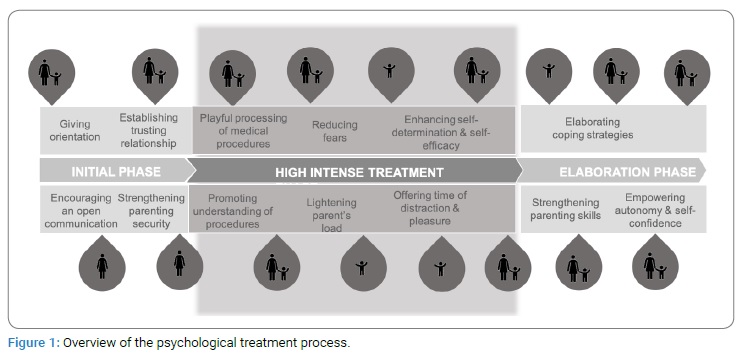
On the patient’s side, the medical play was used to age-adequately process and reenact stressful or threatening treatment situations to increase the boy’s self-determination. Swapping into the role of a doctor allowed the boy to process medical supplies and experience himself as an autonomous person. As shown in (Figure 1), the boy dealt with various topics, gradually showed increased confidence, and was more accessible to medical treatments.
As a result, he could draw parallels between the play setting and his treatment (e.g., a peripheral venous catheter). Compared to his previously observed playing behavior, an increased drive was observed. A common final ritual rounded out the treatment process.
On the parent’s side, the mother was encouraged to use open and age-adequately communication with her child and was counseled in supporting her son in frightening and painful medical procedures. Her ability to convey medical information to her child increased over time. She was counseled in the necessity of parent’s regeneration and was more comfortable using spare time for herself.
A decrease in his aggressive behavior was observed after a few sessions. Especially during the medical procedures, a lower fear and aggressive level were observed, resulting in higher compliance.
When the boy was discharged into day-clinic, psychological treatment sessions were continued to elaborate the practiced coping strategies and increased the adherence. In addition, counseling of the mother was continued, strengthening confidence in her parenting skills and transferring the acquired strategies into the daily routine. After 17 sessions, the psychological condition and compliance to medical treatment were recognized as stable.
Six months after the start of antiangiogenic treatment, the patient was in complete remission. Altogether, the treatment was administered for one year and was well tolerated. The family returned to their home country. Frequently repeated MRIs still show complete remission.
Discussion
The complicated situation of being in a foreign country with a different language and an uncertain future was a challenge for the family. Taking an overall view of the severity of the disease, the presented symptoms of behavioral functioning, the situation was recognized as persistent and escalating distress accompanied by high-risk factors [9]. Assessment of psychosocial needs is standard to determine subsequent steps and resulted in a diagnose of a persistent stress reaction [8,10]. Hence, the boy’s aggressive behavior was regarded as concomitant, comorbid, and consequence of the disease and considered as the natural impact of his experience of helplessness and lack of autonomy due to the intensive oncological treatment. Therefore, it was important for the patient to develop insight and age-adequately understanding of the medical treatments and express associated feelings and actively participate.
Playing is an important aspect of a child’s life. Therefore, it was obvious that the boy appreciated the playful character of treatment. Moreover, it enabled him to experience control of actions, self-efficacy, and expressing emotions. Moreover, the medical play led to decreased aggressive behavior and relief.
Hence, psychopharmacological treatment to regulate behavior was only considered as a second-line treatment option. Moreover, the case report illustrates intensive psychological intervention (psychoeducation) by specialists (considering local specific professional titles such as a clinical psychologist or child life specialists trained in developmental psychology and pediatric psycho-oncology) as a first-line choice to minimize the emotional consequences of the chronic disease and to support the cooperation with the medical treatment.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Medical therapy; Pediatric oncology; Age-adequate psychoeducation; Interdisciplinary treatment; Integrated care system; Persistent stress reaction - excluding medical therapy
Cite this article
Weiler-Wichtl LJ, Kollmann AS, Schwarzinger A, Fohn-Erhold V, Peyrl A, Slavc I, et al. Incompliant and aggressive behavior in a 2-year-old with language barrier during oncological treatment: how can we proceed with necessary therapy? Clin Case Rep J. 2021;2(4):1–4.
Copyright
© 2021 Liesa J. Weiler-Wichtl. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).