Abstract
A 28-year-old woman underwent fertility-sparing surgery with a right salpingo-oophorectomy for a Stage IA well-differentiated mucinous cystadenocarcinoma. She remains disease-free at twenty months of follow-up. A literature review suggests that among young women with early-stage epithelial ovarian cancer, conservative, fertility-preserving surgery is safe. In a well-staged patient, neither ovarian preservation nor uterine conservation had an adverse impact on survival. Advanced stage, grade, and clear cell histology were the main prognostic factors for recurrence.
Introduction
Epithelial ovarian cancer (EOC) is the second most common gynecologic malignancy but is the most lethal [1]. Serous epithelial ovarian cancer is the most common histological type. Mucinous ovarian carcinoma (MOC) is separate from all other EOCs and accounts for only 3% of these malignancies [2]. It has a distinct natural history, molecular profile, chemosensitivity, and prognosis compared to other epithelial ovarian cancer histologic subtypes.
The well-known risk factors for EOCs, such as nulliparity, early menarche, late menopause, lack of breastfeeding, homologous recombination deficiency gene mutations such as the BRCA 1 and 2 gene mutations of the hereditary breast and ovarian cancer syndrome, are not associated with MOC [3]. In contrast, in malignant mucinous tumors, KRAS, HER2 amplification, and TP53 mutations. MOC is the most frequent histological subtype in women under the age of 40 [4]. The only clinical risk factor for MOC is tobacco abuse. Early-stage MOC has an excellent 5-year survival rate of greater than 90%, while advanced MOC is almost uniformly fatal with minimal chemotherapy sensitivity and 5-year survival rates around 12% [2,5].
We present a case of MOC treated at Maulana Azad Medical College in New Delhi and review the literature on fertility-sparing surgical interventions and outcomes for early-stage MOCs.
Case Presentation
A 28-year female, gravida 2, para 2, living children 2, presented with pain in the lower abdomen and a three-month history of a progressively increasing mass in February 2020. There were no associated menstrual, bladder, or bowel complaints. A cystic mass measuring 15.0 cm by 20.0 cm size was palpated on abdominal examination, which corresponded to a 30-week size uterus. The mass was mobile and non-tender. On vaginal examination, the same mass could be felt in the anterior fornix, mobile in all directions, non-tender, cystic to a firm consistency. The uterus was anteverted and normal size, and the bilateral vaginal fornices were free.
Ultrasound showed an anechoic cyst in the right adnexa of size 10.2 cm by 10.0 cm by 10.7 cm with internal echoes and septations. The left ovary, adnexa, and uterus were normal. The findings were corroborated with a CT scan showing a well-defined unilocular cystic lesion 9.7 cm by 13.5 cm by 15.2 cm. The lesion has arisen from the right adnexa with thick internal septations, and an eccentric solid enhancing nodule maintained fat planes with adjacent bowel loops and no locoregional lymphadenopathy. The right ovary was not visualized separately. The scan was suggestive of mucinous cystadenoma/cystadenocarcinoma. Tumor markers were done for the patient, and CA 125 was slightly raised (70.5 IU/ml), CEA was 2.4 ng/ml, CA 19–9 was 2.0 U/ml, LDH was 687.4 U/L, beta hCG 0.18 mIU/ml, and AFP: 2.04 ng/ml were normal.
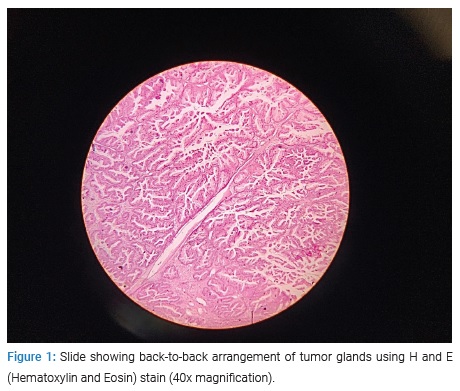
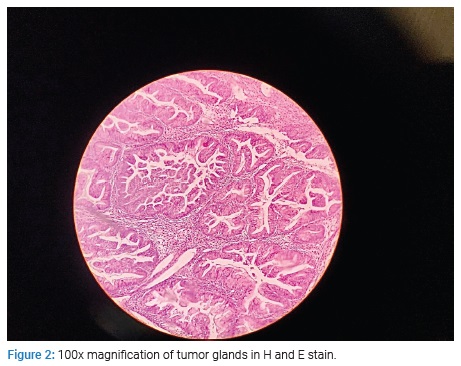
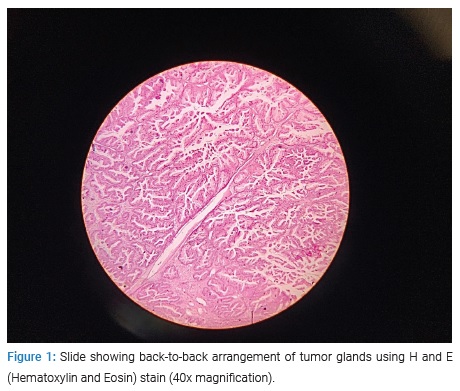
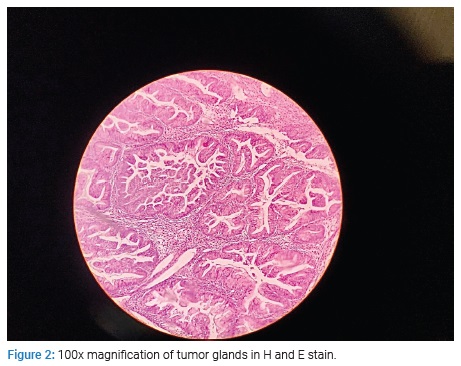
The patient opted for fertility-sparing surgery although she did not desire future childbearing. She underwent an exploratory laparotomy, surgical staging with lymph node sampling, and omentectomy with right-sided salpingo-oophorectomy. Intraoperatively a 15 cm by 20 cm size cystic mass was found with 90cc of gelatinous fluid, thick septate, and a solid area in the cyst wall measuring 4 cm by 5 cm. A frozen section reported a borderline mucinous cystadenoma. The appendix was found to be normal. Peritoneal washings showed no malignant cells, and lymph nodes showed reactive changes. The omental biopsy was unremarkable. The final histopathology from the tumor revealed well-differentiated papillary mucinous cystadenocarcinoma, stage IA positive for immunohistochemical marker CK7. Representative tumor sections are shown in (Figure 1) and (Figure 2).
She was followed closely without chemotherapy and was planned for complete surgical staging. We chose to observe the patient without any chemotherapy since she had a stage IA mucinous cancer. The patient was followed at three-monthly intervals. She is disease-free with normal tumor markers at 20 months of follow-up.
Discussion
Mucinous ovarian carcinoma (MOC) is usually a heterogeneous tumor. A single neoplasm can contain benign, borderline, and carcinoma components, which indicate a stepwise progression to carcinoma [2]. Mucinous cystadenomas account for 20% of benign ovarian neoplasms. Grossly, 95% of the tumors are unilateral, greyish-white, large, often multilocular upon sectioning. Malignant transformation occurs in 5%–10% of tumors.
Certain histological features are suggestive of metastatic mucinous carcinoma. For example, ovarian and pancreatic cystic mucinous carcinomas contain a large amount of intracellular mucin (> 50%) in at least 90% of tumor cells. On the other hand, colloid mucinous carcinomas arising from the gastrointestinal tract, lung, breast, and skin are associated with abundant extracellular mucin accounting for 50% or more tumor volume. In addition to the microscopic features, IHC staining plays an essential role in distinguishing MOC from other possible diagnoses. MOC typically shares positive IHC patterns for CK20, CEA, Ca19–9, and CDX2 with metastatic Colorectal cancer (CRC). Nevertheless, CK7 is mostly positive in MOC and negative in CRC.
Most patients with epithelial ovarian cancer will undergo the surgical standard of care of a radical surgery defined as a full hysterectomy, bilateral salpingo-oophorectomy, and surgical staging and complete cytoreduction [6]. Patients with early-stage disease EOC, borderline ovarian neoplasms, or non-epithelial histologies such as germ cell and sex cord-stromal tumors could be offered Fertility Sparing Surgery (FSS) depending on prognostic factors [7,8]. FSS in patients with ovarian carcinoma preserves the uterus and at least part of one ovary. Complete surgical extirpation in young patients leads to loss of reproductive potential and subjects them to the long-term consequences of estrogen deprivation, resulting in decreased quality of life, grief, distress, and sexual dysfunction. Loss of reproductive capability and surgical menopause can negatively impact survivorship and quality of life (QoL) among young women with ovarian cancer [9].
According to National Comprehensive Cancer Network (NCCN) guidelines, among women with select unilateral stage I tumors (stage 1A and 1C, but not stage 1B) and/or low-risk ovarian tumors (i.e., early-stage, grade 1 neoplasms; borderline histologies). FSS can be considered if fertility preservation is desired and if conservation is technically feasible from a surgical perspective, as our patient did [6].
Pre-operative workup and imaging can help decide whether to offer fertility-sparing surgery to a patient or not. The USG appearance of a mucinous ovarian neoplasm is a cystic mass of varying complexity. Mucinous ovarian neoplasms are often large and may require transabdominal imaging to view the full extent of the mass. They tend to be multilocular, containing small cystic components or honeycomb-like loculi. The cysts tend to have smooth walls. The echogenicity of the intralocular fluid varies based on the mucinous elements of the cyst contents. Cysts filled with thick proteinaceous mucin often demonstrate low-level echoes. MRI may be useful in determining the site of origin (i.e., ovarian vs. uterine vs. metastasis) and for further characterization of masses with indeterminate features at USG. In the setting of an indeterminate complex cystic mass, CT may be useful in confirming the diagnosis. When a mucinous cystic neoplasm is imaged using CT, the imaging findings again include a large, unilateral, complex cystic mass. The attenuation of the fluid within the cyst loculi is variable. It also aids in evaluating the extent of the disease [10].
In a 2009 study, the effect of radical surgery versus fertility-sparing surgery was compared to evaluate survival and long-term outcome on young women greater than or equal to 50 years with stage 1A or 1C epithelial ovarian cancer [11].
In total, 1186 women were identified for the analysis of ovarian preservation. The cohort included 754 women (64%) who underwent bilateral oophorectomy and 432 women (36%) who had preservation of at least a portion of one ovary. The 5-year survival rate among women who underwent oophorectomy was 91% (95% CI, 88%–93%) versus 94% (95% CI, 91%–96%) among women who underwent ovarian conservation. Another cohort of 2911 women analyzed the impact of uterine conservation on survival. The group included 2242 women (77%) who underwent hysterectomy and 679 women (23%) who had uterine preservation. The 5-year survival rate was 91% (95% CI, 90%–93%) among women who underwent hysterectomy compared with 92% (95% CI, 89%–94%) among women who retained their uterus. The findings suggest that, among young women with epithelial ovarian cancer (IA and IC), conservative, fertility-preserving surgery is safe and neither ovarian preservation nor uterine conservation had an adverse impact on survival [11].
Similarly, another series of 52 patients with stage IA and IC disease reported an estimated 5-year survival rate of 98% and concluded that ovarian conservation was safe and was associated with an excellent outcome [12].
Another study reported on 108 patients of reproductive age (≤ 40 years) diagnosed with stage I EOC and treated at Peking Union Medical College Hospital between 1999 and 2013 [13]. The type of surgery included fertility-sparing surgery (FSS) (48.1%) and radical surgery (RS) (51.9%). After a median follow-up of 83 months, it was observed that grade 3 or clear-cell carcinoma were the only independent risk factors for disease-free survival and tumor-specific survival in the multivariate analysis. Fertility-sparing surgery did not affect disease-free survival or tumor-specific survival among patients of reproductive age with stage I EOC and among high-risk patients with stage IC2–3, grade 3, or clear-cell carcinoma.
Clinical outcomes of patients with stage I epithelial ovarian cancer (EOC) who received fertility-sparing surgery (FSS) with those who underwent radical surgery (RS) was compared [14]. A total of 572 patients were retrospectively evaluated. Patients were divided into three groups: group A {FSS (n-74); age, <= 40}; groups B and C [RS; age, <= 40{(B), n-52}; > 40{(C), n-446}]. Five-year overall survival (OS) and disease-free survival (DFS) rates of patients in the groups were as follows: group A, 90.8% (OS)/87.9% (DFS); group B, 88.3% (OS)/84.4% (DFS); group C, 90.6% (OS)/85.3% (DFS), respectively. Additionally, there was no significant difference in OS and DFS among the three groups stratified to stage IA or IC. Furthermore, patients with a grade 1–2 or 3 tumors in the FSS group did not have a poorer prognosis than those in the RS group.
The role of FSS in low and high-risk early EOC patients undergoing comprehensive surgical staging was investigated in another retrospective study [15]. Overall, 307 patients had surgery for early-stage EOC between 1975 to 2011. Seventy (22.8%) and 237 (77.2%) women had FSS and complete radical surgery (RCS), respectively. At univariate analysis, FSS did not influence DFS (p = 0.84) and OS (p = 0.16). Stage of disease was the only factor correlating with DFS (p < 0.001). Independently, increased age (p < 0.001) and high-risk disease (p = 0.01) remained associated with a worse overall survival. Focusing on the high-risk group (stage IAG3 or more), the type of surgery (FSS vs. RCS) did not influence DFS (p = 0.77).
Some reports focused on one subset of ovarian epithelial carcinomas, such as clear cell, endometrioid, or mucinous histologies. One retrospective study conducted between 1991 and 2010 evaluated the safety of fertility-sparing surgery as a treatment option for mucinous ovarian carcinoma [16]. A total of 110 patients underwent primary surgery. At the time of surgery, tumors appeared to be grossly confined to the ovaries in 90 patients, and evidence of metastasis was definite in 20 patients. Of the 90 patients with tumors that appeared to be grossly confined to the ovaries at surgical exploration, 35 (38.9%) underwent fertility-sparing surgery, and the rest underwent radical surgery. There was no difference between recurrence-free survival (p = 0.792) or disease-specific survival (p = 0.706) between the two groups.
Another retrospective analysis identified patients treated for early-stage EOC and compared the clinical outcomes of patients treated with FSS and radical surgery (RS) [17]. A total of 1031 patients were treated at two Institutions, 242 with FSS (group A) and 789 with RS (group B). The median duration of follow-up was 11.9 years. At univariate analyses, FSS was associated with decreased risk of relapse (P < 0.002) and tumor-related death (P < 0.001). However, the type of treatment did not influence cancer-specific survival or relapse-free interval in any grade group.
The lack of randomized clinical trials has led to the heterogeneity of recommendations about selecting FSS eligibility. An examination of predictors of fertility-sparing surgery (FSS) among reproductive-aged women diagnosed with epithelial ovarian cancer (EOC) looked at data from two cancer registries [18]. The Surveillance, Epidemiology, and End Results (SEER) Program and the National Cancer Database (NCDB) were analyzed for women ≤ 44 years old with a diagnosis of primary EOC. Data included 9,017 women (SEER, N = 3,932; NCDB, N = 5,085) with EOC diagnosed between the ages of 15 years and 44 years. In both cohorts, significant determinants of higher FSS receipt included younger age, more recent diagnosis, and diagnosis with mucinous histology, suggesting that FSS could be an option for patients fulfilling these criteria.
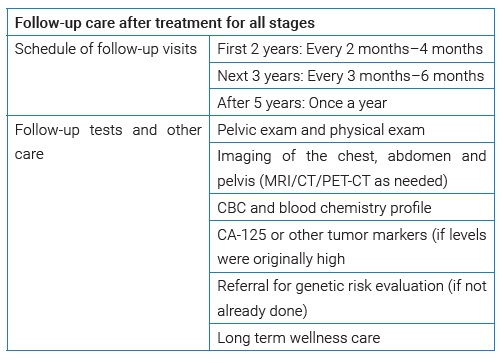
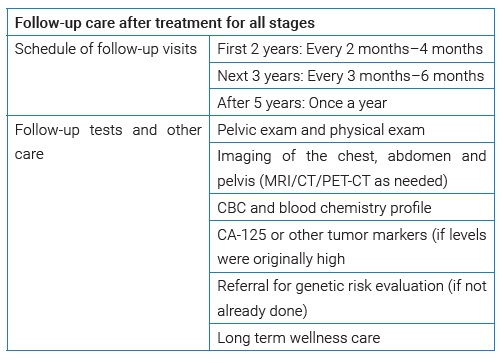
Patients need to be followed up after fertility sparing surgery. The follow-up protocol is as stated by the NCCN for all stages.
Aside from reproductive concerns, surgical menopause in young women results in several long-term sequelae that can be avoided with ovarian preservation, like the risk of coronary disease, osteoporosis and hip fracture, and cognitive dysfunction. A meta-analysis demonstrated that both early menopause and oophorectomy are associated with a significantly increased risk of cardiovascular disease [19]. Another study demonstrated that hysterectomy with bilateral oophorectomy in women < 50 years increases the risk for cardiovascular diseases by 40% [20]. The Religious Orders Study and Memory and Aging Project (SUA) followed 1884 women from two separate cohorts for 18 years. They reported that younger age at the time of salpingo-oophorectomy was associated with a rapid decline in global cognitive function and a high risk of Alzheimer’s disease. These associations were not observed in women with natural menopause [21]. Ovarian conservation was associated with lower death rates regardless of the cause [22].
The decision to perform a limited surgical staging in our patient was justified based on her young age and early stage of disease. However, the question remains on balancing the risk of recurrence and survival associated with conservative surgery with the long-term sequelae of premature menopause and its associated morbidity for women undergoing radical surgery. In addition, the non-reproductive benefits of ovarian conservation should also be considered in young women with early-stage ovarian cancer, as in our patient who underwent conservative surgery despite having her family complete to prevent premature surgical menopause.
Conclusion
Some aspects of the surgical management of MOC are still uncertain. FSS is an option in young, selected patients after proper counseling. In advanced disease, cytoreductive surgery and the amount of residual disease at the end of the surgery are the most critical factors in prognosis.
Choosing the best treatment for younger patients should include careful counseling and shared decision-making. It appears safe for women who have not completed childbearing to carry out conservative surgery. However, close monitoring is important to ensure early diagnosis and treatment for future recurrences. It is imperative to balance each patient’s pros and cons and decide the optimal surgery for the best outcome for the patient in terms of quality of life and disease-free survival.
Cite this article
Agarwal N, Garg R, Gandhi G, Goodman A. Mucinous ovarian malignancy in a young woman: a case report. Clin Case Rep J. 2021;2(5):1–5.