False Positive Uptake of I-131 in a Case of Hemangioma Mimicking as Bone Metastasis
Singh V;
* Jain B;
Ora M ;
Kumar PK;
-
Singh V: Department of Nuclear Medicine, SGPGIMS, Lucknow, India.
-
* Jain B: Department of Nuclear Medicine, SGPGIMS, Lucknow, India.
-
Ora M : Department of Nuclear Medicine, SGPGIMS, Lucknow, India.
-
Kumar PK: Department of Nuclear Medicine, SGPGIMS, Lucknow, India.
-
Jan 21, 2022 |
-
Volume: 3 |
-
Issue: 1 |
-
Views: 2582 |
-
Downloads: 2416 |
Abstract
Thyroid carcinoma is treated by near-total or total thyroidectomy, followed by 131Iodine (131I) ablation of any remnant thyroid tissue. 131Iodine whole-body scan (WBS) has been used for the follow-up of differentiated thyroid carcinoma for several decades. The specificity of the 131I whole-body scan for detecting residual, metastatic, and recurrent differentiated thyroid carcinoma is reported to be higher than 90%. However, radioiodine uptake is not specific to thyroid tissue. It could also be observed in various physiological and pathological conditions that could be mistaken for metastasis. Therefore, a thorough understanding of radioiodine physiology and biodistribution is critical when interpreting radioiodine scintigraphic studies to avoid misinterpretation of the various variants as thyroid cancer metastases. Here we present a papillary carcinoma case treated with 131I following total thyroidectomy and showing uptake of 131I in vertebrae on follow-up whole-body radioiodine scintigraphy mimicking as bone Metastasis, which was later found to be a hemangioma.
Abbreviations
I-131: Iodine 131; WBS: Whole Body Scan; SPECT: Single-Photon Emission Computed Tomography; CT: Computed Tomography; TFT: Thyroid Function Tests; USG: Ultrasonography; FNAC: Fine Needle Aspiration Cytology; PCT: Papillary Carcinoma of Thyroid; Tg: Thyroglobulin; Atg: Antithyroglobulin; Bq: Bequerel; mCi: mili Curie.
Introduction
Iodine-131 (I-131) whole-body scan (WBS) plays an essential role in the management of patients with differentiated thyroid carcinoma (DTC) to detect normal thyroid remnant and recurrent or metastatic disease [1]. A focus of 131I accumulation outside the thyroid bed and physiological uptake areas is strongly suggestive of distant functioning metastasis [2]. However, many false-positive 131I WBS findings have been reported in the literature. Although being a sensitive marker for the detection of thyroid cancer, Radioiodine is not specific for thyroid tissue [3]. Apart from thyroid, uptake can also be seen in including thymus [4], liver, gastrointestinal tract, nasal activity, lactating breasts, Zenker’s diverticulum, and Meckel’s diverticulum or benign diseases, such as hiatal hernia [5], inflammatory lung disease, sialadenitis, cysts, and inflammation or in a variety of benign and malignant non-thyroidal tumors, which could be mistaken for thyroid carcinoma [2,6,7].
Therefore, a thorough understanding of radioiodine physiology and biodistribution is critical when interpreting Radioiodine scintigraphic studies to avoid misinterpretation of physiologic and pathologic variants as thyroid cancer metastases. The interpretation of Radioiodine scintigraphic studies should be performed in conjunction with a comprehensive history, histopathologic correlation, pertinent blood parameter values, and correlation with available anatomic images and the physical examination findings.
Differentiating a false-positive finding from a metastasis on pretherapy radioiodine scintigrams is essential to determine the appropriate radioiodine treatment dose. The correct interpretation of post-therapy Radioiodine scintigraphic studies is also essential to determine if repeated radioiodine doses are required and for the patient’s future clinical and imaging follow-up [8].
Quite a few false-positive findings have been reported in the literature. They are further demonstrated with SPECT/CT hybrid imaging (single-photon emission computed tomography SPECT integrated with computed tomography).SPECT/CT has improved the prognostic value of planar radionuclide techniques as it evaluates morphological and functional information together. The use of SPECT/CT significantly increases the diagnostic accuracy of planar scintigraphy. SPECT/CT has been documented to be of supplementary value in the accurate anatomic localization and characterization of radioiodine uptake as false-positive findings, particularly in cases with incongruous findings of a low serum thyroglobulin level but positive findings on Radioiodine whole-body planar scintigram [8].
Case Presentation
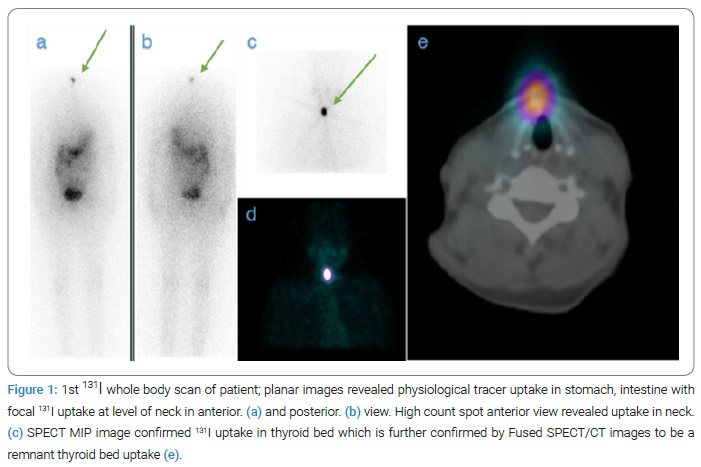
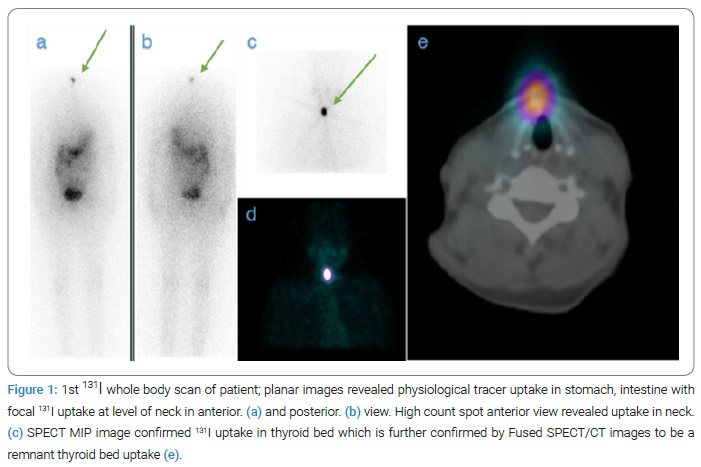
A 40-year-old female patient presented with a complaint of anterior neck swelling for three years. After further routine investigations (TFT, USG, FNAC), a diagnosis of papillary carcinoma of the thyroid (PCT) was made, for which the patient underwent total thyroidectomy. The final histopathology report confirmed it to be a case of PCT. The patient was referred to our department for a radioactive iodine scan and further treatment. After two months, the patient was scheduled for follow-up in our department with the advice to stop thyroxine one month before the visit. On the follow-up day, blood parameters included TSH- > 150 micro IU/ml, Serum thyroglobulin (S.Tg) – 0.3, Anti Thyroglobulin (Atg)- 109.4 IU/ml. A whole-body radioiodine scan was done, planar images showed uptake in the thyroid bed only. SPECT/CT of neck and thorax confirmed it to be thyroid bed uptake (Figure 1). There is no other uptake anywhere else in the body.
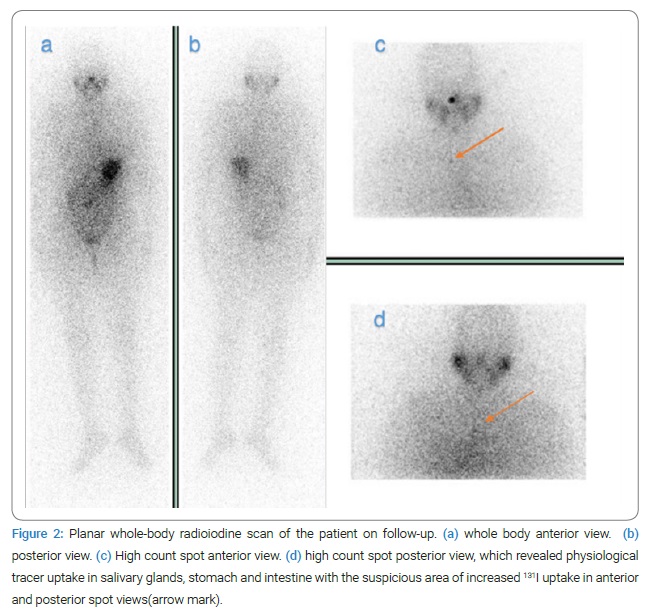
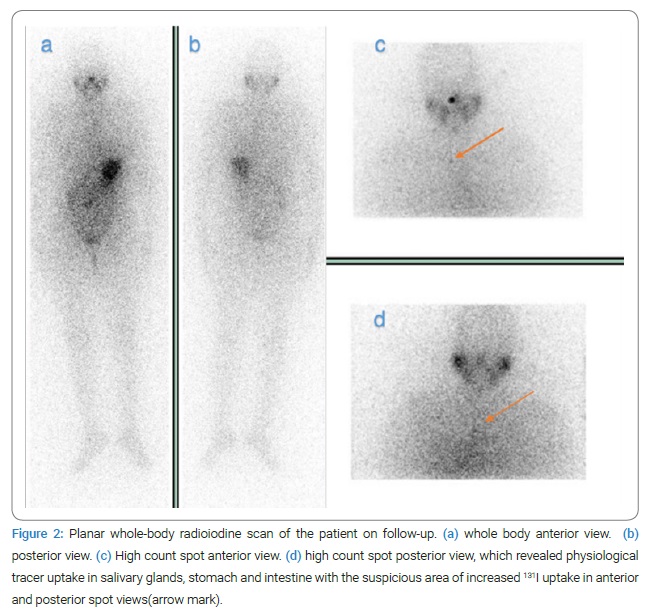
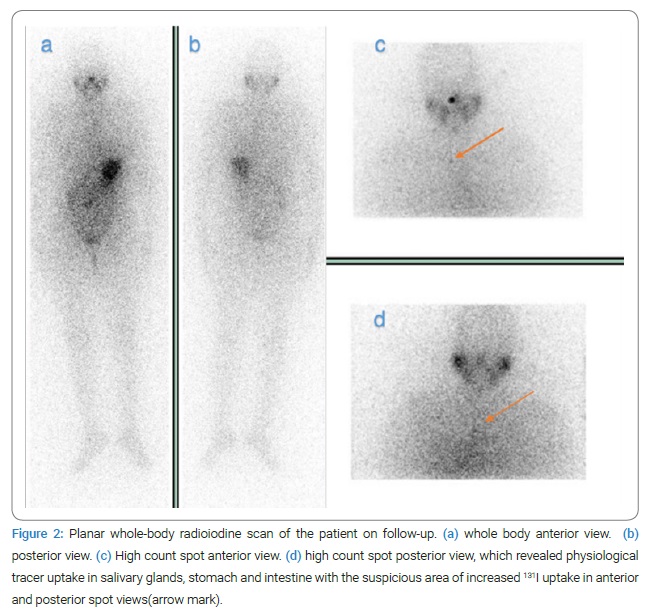
The patient was treated for remnant with 1850 Bq (50 mCi) of 131I orally under medical supervision. The post-therapy scan showed similar uptake as the pre-therapy scan. After 131I therapy patient started on thyroxine and was further scheduled for follow-up after six months with advice to stop Thyroxine a month before. Follow-up whole-body radioiodine scan after six months revealed a suspicious focus of mildly increased uptake in the upper thorax; however, values of serum Tg and ATg showed a decreasing trend (S.Tg < 0.2, ATg-16.4). SPECT/CT of the suspected region was done, which revealed mild uptake in the first thoracic vertebra. CT scan of the neck and upper thorax was consistent with hemangioma in the body of the first thoracic (D1) vertebra (Figure 2 and 3). On looking at the whole scenario, the uptake on the 131I scan was considered false-positive uptake in haemangioma. The patient is on regular follow-up in our department and is presently asymptomatic & disease-free.
Discussion
Thyroid carcinoma requires a multidisciplinary approach for its management. Nuclear medicine and radioactive iodine, in particular, have been deterministic in the diagnosis and treatment of differentiated thyroid carcinoma. Papillary carcinoma, the most common among all thyroid cancers, is increasing in incidence around the world [9]. Differentiated Thyroid Cancer (DTC) is a malignant tumor, with a favorable prognosis and low mortality, compared with most other malignancies [10].
Several false-positive findings have already been reported; Benign hemangiomas are one of them. Vertebral hemangiomas are common benign vascular tumors of the spine, with an incidence of 10%–12%, more common in the thoracic spine. They are usually asymptomatic and are diagnosed incidentally. Occasionally, symptoms are manifested due to pressure effects on the surrounding structures or the vertebral body’s destruction [11]. The characteristic histopathological pattern is thin-walled, blood-filled vessels and sinuses lined by endothelium and interspersed among the bones’ longitudinally orientated trabeculae [12]. Due to this structural arrangement, vertebral hemangiomas appear ‘Corduroy’ in sagittal sections and ‘polka dot appearance’ in axial images [13]. False-positive uptake of 131I in a case of hemangioma could be due to intravascular blood pooling and transcapillary escape of iodine with interstitial retention, as suggested by previous reports [14,15]. Therefore clinical, biochemical, functional, and anatomical correlation should also be emphasized before making therapeutic decisions. The presence of metastatic bone disease can have significant consequences in the treatment, course, and prognosis of the disease; hence, a bony lesion’s detailed evaluation is essential. This case report highlights the use of nuclear medicine modalities in detecting false-positive uptake of 131I to avoid additional costly investigations and unnecessary surgery or exposure to further radiation from repeated therapeutic doses of 131Iodine.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Vini L, Harmer C. Radioiodine treatment for differentiated thyroid cancer. Clin Oncol (R Coll Radiol). 2000;12(6):365–372.
- American Thyroid Association Taskforce On Radioiodine Safety, Freitas J, McDougall IR, Dauer LT, Hurley JR, Brierley JD, et al. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I : practice recommendations of the american thyroid association. Thyroid. 2011;21(4):335–346.
- Oh JR, Ahn BC. False-positive uptake on radioiodine whole-body scintigraphy: physiologic and Pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging. 2012;2(3):362–385.
- Haghighatafshar M, Farhoudi F. Incidentally visualization of the thymus on whole-body iodine scintigraphy: report of 2 cases and review of the latest insights. Medicine (Baltimore). 2015;94(26):e1015.
- Haghighatafshar M, Khajehrahimi F. Hiatal hernia uptake of iodine-131 mimicking mediastinal metastasis of papillary thyroid carcinoma. Indian J Nucl Med. 2015;30(4):347–349.
- Shapiro B, Rufini V, Jarwan A, Geatti O, Kearfott KJ, Fig LM, et al. Artifacts, anatomical and physiological variants, and unrelated diseases that might cause false-positive whole-body 131-I scans in patients with thyroid cancer. Semin Nucl Med. 2000;30(2):115–132.
- You DL, Tzen KY, Chen JF, Kao PF, Tsai MF. False-Positive Whole-Body Iodine-131 Scan Due to Intrahepatic Duct Dilatation. J Nucl Med. 1997;38(12):1977–1979.
- Chudgar AV, Shah JC. Pictorial review of false-positive results on radioiodine scintigrams of patients with differentiated thyroid cancer. Radiographics. 2017;37(1):298–315.
- Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013;2013:965212.
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29.
- Fox MW, Onofrio BM. The natural history and management of symptomatic and asymptomatic vertebral hemangiomas. J Neurosurg. 1993;78(1):36–45.
- Wilner D. Radiology of bone tumors and allied disorders. Saunders: Philadelphia; 1982.
- Laredo JD, Reizine D, Bard M, Merland JJ. Vertebral hemangiomas: Radiologic evaluation. Radiology. 1986;161(1):183–189.
- Khan S, Dunn J, Strickland N, Al-Nahhas A. Iodine-123 uptake in vertebral haemangiomas in a patient with papillary thyroid carcinoma. Nucl Med Rev Cent East Eur. 2008;11(1):30–33.
- Laguna R, Silva F, Vazquez-Sellés J, Orduña E, Flores C. Vertebral hemangioma mimicking a metastatic bone lesion in well-differentiated thyroid carcinoma. Clin Nucl Med. 2000;25(8):611–613.
Keywords
I-131; False positive; Hemangioma, Iodine whole body scan
Cite this article
Singh V, Jain B, Ora M, Kumar PK. False positive uptake of I-131 in a case of hemangioma mimicking as bone metastasis. Clin Case Rep J. 2022;3(1):1–4.
Copyright
© 2022 Jain B. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).