Abstract
Adnexal torsion sometimes causes diagnostic challenges, mainly in a pediatric patient and when it lacks an ovarian tumor. For four days, a 9-year-old girl presented to the medical service complaining of right lower abdominal pain. Laboratory data showed mild leukocytosis and an elevated C-reactive protein. Abdominal ultrasound showed an enlarged right ovary measuring 57 mm x 38 mm. A pelvic computed tomography showed a small amount of free fluid in the peritoneal cavity. These data suggested an adnexal torsion, and therefore laparotomy was performed. Right adnexal torsion was confirmed with almost necrotic ovary and fallopian tube, resulting in right adnexectomy. There was no underlying ovarian tumor, and thus normal-ovary-torsion was confirmed. Adnexal torsion in childhood is an uncommon finding. This should be listed as a differential diagnosis of non-specific acute abdominal pain. Early diagnosis before ovarian necrosis is completed might preserve the ovary. Physicians should be aware of this condition.
Introduction
Adnexal torsion is characterized by the complete or partial rotation of the ovary and its adnexa, such as uterine suspensory ligaments [1]. This is often associated with an ovarian tumor or cyst, but it may occur in normal ovaries, especially in children. Torsion of adnexal structures may involve the ovary or the tube, but it usually affects both. In most cases, it is unilateral with a slight predilection for the right side and is commonly confused with acute appendicitis [2].
Abdominal pain is the most common ovarian masses symptoms. When intense acute pain presents, it may indicate adnexal torsion or rupture with hemorrhage [3]. Nevertheless, abdominal pain has a high prevalence in gastrointestinal disorders, making diagnosis difficult when it is caused by adnexal torsion, especially in very young children who cannot accurately describe their symptoms or locate their discomfort [4].
Imaging exams may show increased ovarian volume with decreased or absent vascularity. Late diagnosis or treatment may lead to hemorrhagic necrosis and other complications such as peritonitis [2]. Infertility is a rare condition, but it cannot be excluded. Early diagnosis would enable a conservative treatment consisting of ovarian untwisting and fixing [5].
Case Presentation
For four days, a 9-year-old healthy female presented with abdominal pain in the right iliac fossa region. Laboratory tests showed mild leukocytosis and an increased relative protein C. On abdominal examination, Blumberg’s sign was present, which is suggestive of peritoneal irritation.
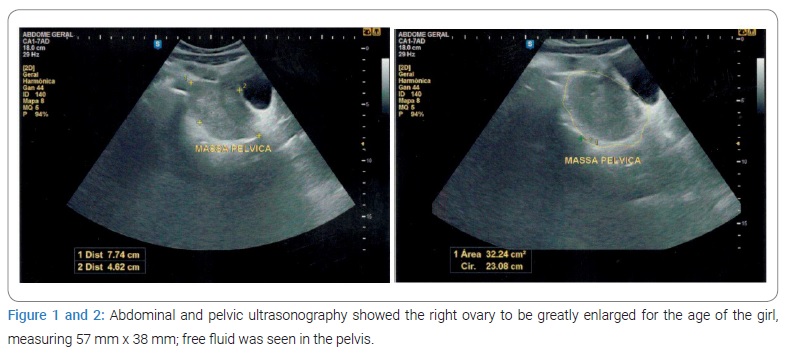
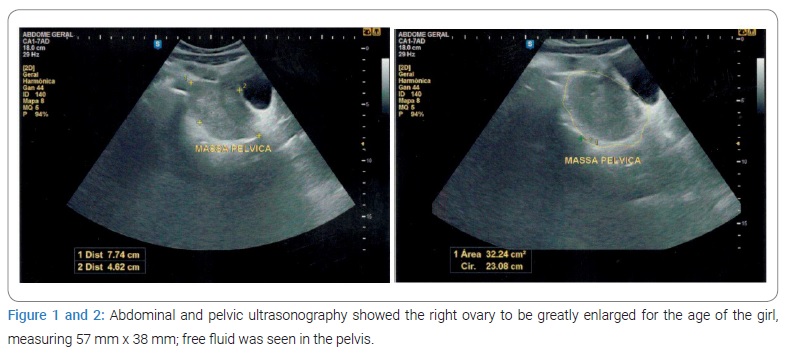
The first abdominal ultrasound describes a hypoechoic right ovary with regular limits and increased volume (5.7 cm/3.85 cm) without visualizing normal parenchyma. There was also a small amount of free fluid in the pelvis. After 48 hours, with increasing intensity of abdominal pain, a new ultrasound examination was performed. An increase in the right ovary volume (7.6 cm/4.6 cm) was identified concerning the previous exam and the absence of vascularization on color Doppler. As in the first ultrasound, the right ovary was hypoechoic, with regular limits and without visualization of normal ovarian parenchyma (Figure 1, Figure 2). The propaedeutics were complemented by computed tomography, which revealed the presence of an adnexal mass (round formation) separated from the uterus, with no signs of hemorrhagic infarction and no limited vascularization.
The findings were corroborated with a pelvic computed tomography scan showing an adnexal mass with intermediate density in the pelvis, in a right paramedian situation, and with regular contours. The contrast medium showed a slight enhancement, associated with tiny peripheral hypodense formations, measuring about 4.6 cm x 4.2 cm x 5.9 cm and an estimated volume of 59.27 cm3. A small amount of free fluid in the peritoneal cavity was also observed, especially in the right iliac fossa, the cecal appendix of normal caliber, and rounded formation in the pelvis.
The scan was suggestive of enlarged ovaries secondary to partial torsion. With the etiology to be clarified, the ovaries were with increased dimensions. No tumor was seen.
The hypothesis of partial adnexal torsion was then considered, and a decision was made for surgical treatment. The child was referred for a laparotomy procedure as the only way available in the hospital. A small amount of blood was found in the abdominal cavity, and identification of a right adnexa with an enlarged and completely ischemic ovary. Thus, right adnexal torsion was detected, resulting in a right adnexectomy. No changes were seen in the left adnexa, and a review of hemostasis and closure by planes was then performed. The surgical procedure was uneventful.
After surgery, the patient was in good general condition and already walking. She reported diuresis and evacuation. On physical examination, the abdomen was free, and the surgical wound had a good appearance. Thus, she was discharged from the hospital.
The anatomopathological examination report showed, at macroscopy, a right ovary with an increased volume and an external surface that was blackish in color, and a hemorrhage, measuring 7.0 cm x 4.2 cm x 3.5 cm and weighing 80.0 g. A cyst with yellowish edges and a brownish-black content was seen in the area where the incisions had been made. This coexisted with several smaller cysts with thin edges, gelatinous contents, and smooth and shiny internal surfaces. On the other hand, the corresponding fallopian tube measured 4.0 cm in length by 0.8 cm in external diameter and presented a light brown and shiny serous. Four-slide microscopy showed an ovary with coagulation necrosis and diffuse blood congestion, with tiny cystic structures lined with flattened epithelium and Albicans bodies. No elements suggestive of neoplasia or malignancy were observed. A slide with material from the corresponding fallopian tube shows sections with hemorrhage and diffuse coagulation necrosis. The ovary was seen with changes compatible with ischemic etiology (adnexal torsion), with no suggestive elements of neoplasia or malignancy—fallopian tube with changes compatible with ischemic etiology.
A month later, the child was in good general condition. Her appetite was preserved, and she tolerated her diet. She remained afebrile, flushed, hydrated, and free abdomen; her surgical wound had a good appearance.
Discussion
Adnexal torsion is an uncommon gynecological emergency that refers to the complete or partial rotation of the ovaries bending the axis of the ovarian ligaments [6]. Thus, the blood supply of these organs is impaired and may result in tissue necrosis, thromboembolism, sepsis, and the loss of ovarian function. The first case of normal adnexal torsion and its resulting infarction was described in 1898 by Hartman [7].
Adnexal torsion is the fifth most common gynecological emergency in surgery, representing 2.7% of surgical emergencies [8]. The torsion of the ovarian pedicle produces vascular stasis, initially of venous origin, which evolves with an arterial component as the edema resulting from the first progresses [2].
Symptoms are vague, mainly moderate to severe, with diffuse or localized pelvic pain, often associated with nausea and vomiting [6]. Diagnosis is usually delayed by non-specific symptoms included in the differential diagnosis of acute abdomen in children and adults [5].
A retrospective study analyzed 21 patients under the age of 18 who were admitted to Changhua Christian Hospital in Taiwan with adnexal torsion between June 2003 and June 2010. All patients had abdominal pain, followed by vomiting and nausea (33.3%). The average period between the onset of symptoms and diagnosis was 3.29 days. Torsion of the right adnexa occurred in fourteen patients and the left adnexa in seven patients. One case was treated conservatively. The other cases showed in the anatomopathological examination were as follows: eight dermoid cysts, two cystadenomas, one follicular cyst, eight simple cysts, and one malignant tumor [4].
Another study analyzed cases of fallopian tube torsion over fifteen years and concluded that abdominal pain presented itself as a symptom in all cases; other symptoms such as nausea and vomiting are variable. Also, there were no specific symptoms, clinical, imaging, or laboratory findings that might be considered conclusive in diagnosing this condition. The authors also claimed that its diagnosis is rarely made before surgery [9].
Infertility due to adnexal torsion is rare, but it cannot be excluded. Early diagnosis would enable conservative treatment consisting of ovarian untwisting and fixing. However, due to diagnostic difficulties, as seen in the literature, the treatment of choice for adnexal torsion is usually surgical resection, which allows its diagnosis and treatment [5].
In children, torsion of a normal ovary occurs due to the presence of a disproportionate length of the utero-ovarian ligament that causes excessive ovarian movement. The higher prevalence of torsion in the right ovary compared to the left at a ratio of 3:2 is due to the greater mobility of the cecum and distal ileum on the right side and the greater space occupied by the sigmoid colon on the left side [8]. Differential diagnoses occur mainly with acute appendicitis on the right side, and it warns of the difficult diagnosis when on the left side [7].
Known risk factors for adnexal torsion are previous ovarian cysts, tubal connection, ovarian hyperstimulation syndrome; polycystic ovary syndrome; gestation; a history of endometriosis, and pelvic infection or hydrosalpinx [10].
Imaging diagnostics may be inconclusive. Nuclear Magnetic Resonance and Computed Tomography may detect ovarian masses, edema, and hemorrhagic infarcts, and these findings are highly suggestive of adnexal torsion. Ultrasonography, and more precisely, Doppler ultrasonography, represents the safest assessment method, with the reduction and absence of venous and arterial flow being the most consistent findings [8]. In the case presented here, the “ovarian crescent sign” (OCS) was not observed, defined as a hypoechoic normal ovarian tissue, with or without follicles, adjacent to a pathological ovarian mass, which would help the differential diagnosis between malignant and benign lesions. As the lesion was greatly enlarged, normal ovarian tissue appears to have been stretched around the lesion, which may have made it difficult to detect the ovarian follicles, as described by Stankovic et al., who found the absence of the OCS in 85% of the torsion adnexal masses [11].
Patients with an adnexal torsion may present intermittent episodes of pain on the affected side, days or even weeks before presentation. It is estimated that this may occur in 10% of patients [8]. There is a distinction between twists that occur suddenly and those that occur chronically, lasting longer [7].
Treatment of adnexal torsion is primarily surgical. If feasible, the ovary will usually stabilize with sutures, and any ovarian mass suspected to have caused the torsion will be removed [8]. When an adnexal torsion is diagnosed or highly suspected, it is implied that an early ovarian untwisting enables ovarian rescue. Early laparoscopic untwisting has become the preferred method of ovarian preservation in women who wish to preserve future fertility [10]. One study suggests that Doppler ultrasound findings may distinguish ovaries that require excision from those that may be preserved by laparoscopic untwisting. In cases of adnexal torsion associated with a malignant tumor, oophorectomy is considered the most appropriate treatment due to the risk of thromboembolism.
Conclusion
Adnexal torsion in childhood is an uncommon finding, but it should be considered in the differential diagnosis of non-specific acute abdominal pain. There are no imaging findings or laboratory changes that lead to an accurate diagnosis of adnexal torsion, which makes this diagnosis more challenging and, therefore, reaffirms the importance of the case presented. Early diagnosis is essential as the risk of necrosis of the ovaries and tube increases with time since the onset of abdominal pain.
It is the pediatrician’s responsibility to be aware of and to consider this disease despite the inaccuracy of children in reporting its symptoms to make an early diagnosis with less possibility of ovarian resection.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article Informed consent was obtained for this publication.
Keywords
Adnexal torsion; Acute abdomen; Oophorectomy; Laparotomy; Pediatric; Abdominal pain; Pelvic ultrasonography
Cite this article
De Faria IM, Guimarães MR, De Faria MLC, Silveira RPR, Chaves RG. Adnexal torsion during childhood: a case report. Clin Case Rep J. 2022;3(1):1–4.
Copyright
© 2022 Roberto Gomes Chaves. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).