Abstract
Spontaneous heterotopic pregnancy is a rare condition and can present with signs of hypovolemic shock due to rupture. A 31-year-old woman presented in the emergency department with lower abdominal pain with signs of peritoneal irritation and hypovolemic shock. She was eight weeks pregnant via spontaneously conceived intrauterine pregnancy confirmed on an ultrasound scan. Her past medical history was significant for a C-section 2 years ago. Initially managed in the resuscitation room in ED, she underwent laparoscopic washout of hemoperitoneum and right salpingectomy for ruptured and bleeding heterotopic pregnancy. Postoperatively, she remained well and was discharged home on the third postoperative day. Ultrasound scans done in the follow-up period confirmed satisfactory progression of viable intrauterine pregnancy.
Introduction
Spontaneous heterotopic pregnancy is a rare and potentially life threatening condition which can easily be missed [1]. It is a condition in which intrauterine and extrauterine pregnancies occur at the same time. Co-existence of heterotopic pregnancy should be suspected in a woman with hypovolemic shock and viable intrauterine pregnancy. We report a case of a young woman presenting with hypovolemic shock due to ruptured heterotopic pregnancy.
Case Presentation
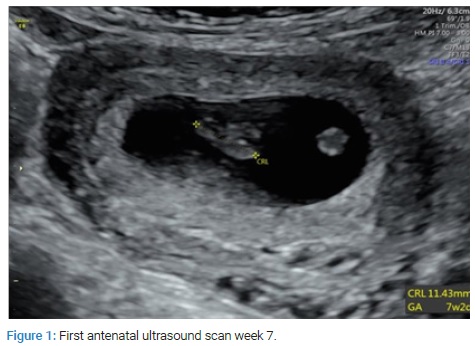
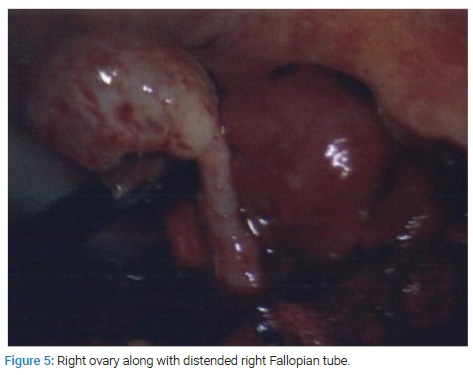
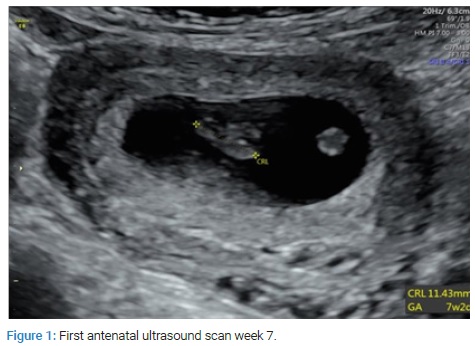
A 31-year-old Caucasian woman (gravida 2, para 1) presented to the emergency department after experiencing a few hours of severe lower abdominal pain alongside an episode of vomiting. The patient was eight weeks pregnant via spontaneous conception. She underwent a cesarean section for a spontaneously conceived full-term pregnancy two years ago. There were no associated medical problems, and she was not on any regular medications. There was no history of assisted reproductive therapy, ectopic pregnancy, miscarriage, or pelvic inflammatory disease. Her current pregnancy was confirmed 1week ago by a Transvaginal Ultrasound Scan (TVUS). The scan revealed a normal Intrauterine Pregnancy (IUP) with no free fluid or adnexal masses. The fetus had a Crown-Rump Length (CRL) of 11.43 mm, consistent with gestational age of 7 weeks and two days (Figure 1).
At ED triage, she reported ongoing lower abdominal pain and discomfort. She denied abnormal vaginal bleeding or discharge. Although she reported some nausea and an episode of vomiting while in ED, there were no urinary or lower GI symptoms. Her vital signs were stable and normal with a heart rate of 60 bpm, blood pressure 104/71, respiratory rate of 17/min, SpO2 of 99% at room air. Her blood sample was taken for a set of blood tests; an IV line was secured in the left antecubital vein.
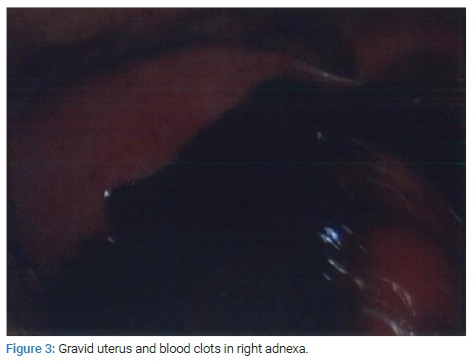
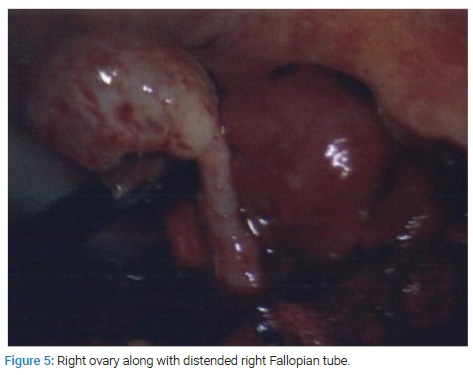
While waiting to be seen by a doctor, she felt dizzy and fainted. She was transferred immediately to the resuscitation room. She regained her consciousness spontaneously but appeared pale. Her repeat observation of vital signs showed HR of 67 bpm, BP 83/59 mm Hg, respiratory rate of 32/minute, and SpO2 99% on 2 L/min oxygen via face mask. Abdominal examination revealed signs of peritonism, including tenderness, guarding, and rebound tenderness more pronounced in the right lower quadrant. Per vaginal examination by the on-call Obstetrics & Gynaecology team revealed closed cervical os with no bleeding seen in the vaginal canal. At this point, On-call surgical team was called to A & E for further assessment and management of the patient. She continued to be resuscitated with IV fluids and analgesia. A urinary catheter was placed. VBG analysis revealed a hemoglobin level of 93 gm/liter compared to 134 gm/liter taken at the time of triage in ED. A bedside ultrasound scan revealed free fluid in the pelvis and hepato-renal pouch. It also confirmed viable intrauterine pregnancy. She was started with an O-negative blood transfusion as part of ongoing resuscitation. The surgical team decided to proceed with diagnostic laparoscopy under general anesthetics in emergency theatre to identify and potentially control the source of bleeding. Informed consent was taken, and her partner was involved in decision making as well. Laparoscopy revealed approximately 2 liters of hemoperitoneum with blood clots, distended and bleeding right Fallopian tube, and enlarged uterus (Figure 2).
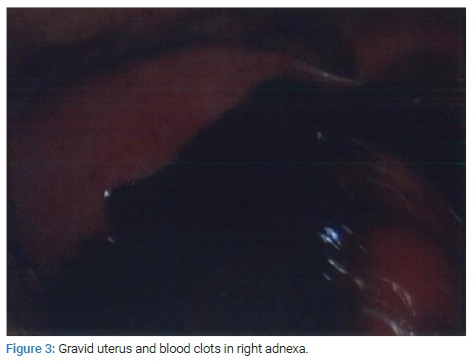
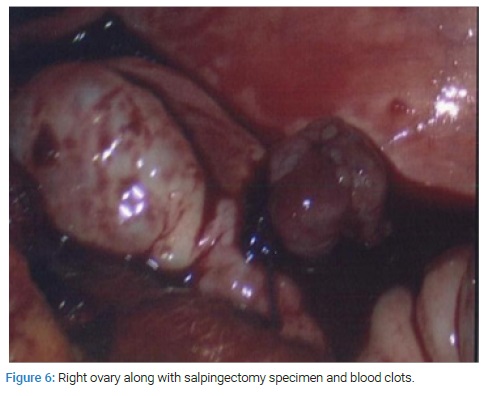
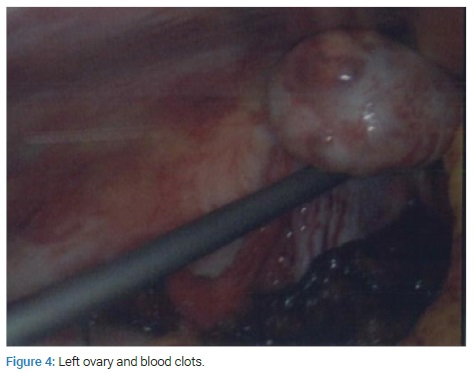
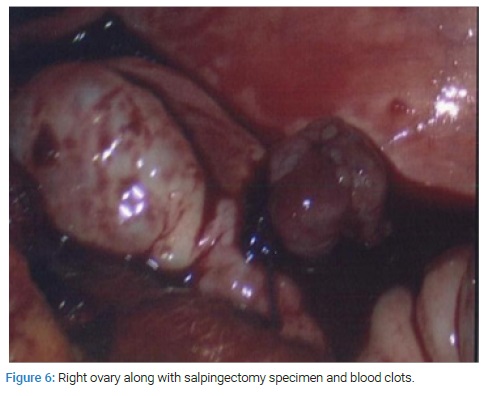
A thorough peritoneal wash-out was carried out, and right salpingectomy was done (Figure 3 and Figure 6). A size 24Fr Robinson drain was left in the pelvis. Intraoperatively, she remained hemodynamically stable and did not require any ionotropic support. Postoperatively she remained in HDU for 24 hours before being transferred to the ward for ongoing care. A repeat ultrasound scan on postoperative day 1 confirmed viable intrauterine pregnancy. The scan visualized a gestational sac and an embryo measuring CRL of 21.7 mm (22nd percentile). She was discharged home on the 3rd post-operative day without any early postoperative complications. Histology of the right Fallopian tube showed chorionic villi consistent with products of conception (Figure 5). She has been regularly followed up with ongoing antenatal care. Her latest ultrasound scan done at 12 weeks of gestational age is satisfactory (Figure 4 & Figure 7).

Discussion
Heterotopic pregnancies (heterotopic pregnancy) in natural conception are a rare and potentially life-threatening phenomenon. It is defined as the simultaneous occurrence of both an intrauterine and extrauterine pregnancy. It occurs most commonly in the fallopian tube; however, cervical, ovarian, and abdominal heterotopic pregnancies have also been found [2]. The first reported case of heterotopic pregnancy in literature dates back to the year 1708 during an autopsy procedure [1,3]. The incidence of heterotopic pregnancy in spontaneous conception is extremely rare and was previously reported at 1:30,000 [4]. The use of Assisted Reproductive Therapies (ART) increases heterotopic pregnancy risk by 30 to 60 fold [5,6]. In recent years, the incidence of heterotopic pregnancy has risen to 1:7000, reflecting the rise in the use of assisted reproductive therapy (ART) and increased prevalence of tubal disease [2].Talbot et al. note that 71% of cases are associated with at least one risk factor [7], most commonly: ART, previous ectopic or miscarriage, fallopian tube damage, or previous pelvic surgery [8]. However, in this case, no predisposing risk factors were identified, which contributed to the delay in diagnosis. Early diagnosis of heterotopic pregnancy is difficult as patients can present non-specifically, and up to 50% of patients can be asymptomatic [9]. Up to 66.7% are diagnosed after rupture of the ectopic, as was in this case [10]. When symptoms are present, Rees et al. noted acute lower abdominal pain, hypovolemic shock, uterus enlargement, and peritoneal irritation should raise clinical suspicion. Vaginal bleeding has been reported in less than 50% of patients, and if present, it may be retrograde due to intact endometrium from the intrauterine pregnancy [11,12]. The gold standard investigation to diagnose heterotopic pregnancy is Transvaginal Ultrasonography (TVUS), with sensitivity and specificity ranging from 71%–100% and 41%–99%, respectively. In their study, Yu et al. showed that 56% of patients were diagnosed by routine ultrasound examination, and in the remaining 44%, heterotopic pregnancy was not diagnosed until the second scan [13]. Another study reported that diagnosis was made by laparoscopy/laparotomy in 74% of cases [14]. In our case, the patient had a TVUS showing an intrauterine pregnancy of 6 weeks of gestational age without tubal pregnancy evidence. Our patient did undergo a bedside ultrasound scan in ED, which revealed free fluid in the abdomen, which prompted an emergency laparoscopy, and the diagnosis was made after that of a ruptured right ectopic. As has been continually echoed in the literature, one of the main pitfalls with TVUS as a gold standard is that a normal intrauterine pregnancy serves as false reassurance for the exclusion of an ectopic pregnancy result sees many cases of heterotopic pregnancy being missed. One study in 2011 showed TVUS did not pick up 33% of cases due to false reassurance by detection of an intrauterine pregnancy [15]. As such, though it is widely agreed that TVUS plays an important role in diagnosing heterotopic pregnancy; the salient learning points from this case report is that in the absence of predisposing risk factors and a TVUS reporting a normal intrauterine pregnancy, this should not be used as a means to exclude a heterotopic pregnancy definitively. Furthermore, a repeat ultrasound scan can improve diagnostic efficiency and prevent misdiagnosis. A study conducted in 2014 reported that repeat ultrasound is required to improve the overall diagnostic sensitivity of heterotopic pregnancy [13]. Free fluid in the abdomen coupled with clinical features of tubal rupture or hemodynamic instability should prompt clinicians to consider heterotopic pregnancy and thus result in diagnostic and therapeutic laparoscopy performed earlier. The management of heterotopic pregnancy depends upon various factors, including gestational age at the diagnosis and urgency of clinical situation [16]. Surgery is still the most frequently chosen method of treatment in a patient with unstable hemodynamic parameters [17]. The intervention aims to save women’s lives and preserve intrauterine pregnancy and resolve heterotopic pregnancy [16,17]. Surgical options include, but are not limited to, salpingectomy, salpingotomy, and oophrectomy which could be performed as an emergency laparotomy or laparoscopy in experienced hands [16].
This case was particularly interesting as the patient was symptomatic with an acute abdomen’s clinical features, signs of peritoneal irritation, hemodynamic instability, declining serum hemoglobin, free intraperitoneal fluid detected on ultrasound scan, and viable singleton intrauterine pregnancy. The patient was managed by a multidisciplinary team approach beginning with A & E, Obstetrics & Gynecology, and then on-call surgical team and support from a blood bank, anesthetics, and theatres and recovery teams. Also, the therapeutic procedure was successfully carried out by laparoscopic approach without any perioperative complication. It was interesting to find out that the cause of hemoperitoneum was ruptured ectopic tubal pregnancy along with spontaneously conceived viable intrauterine pregnancy in this young woman. It also reminded us that the differentials for spontaneous acute hemoperitoneum are vast and varied and can encompass rare gynecological conditions. This case presents a crucial learning point; features of tubal rupture or acute abdomen, despite confirmed intrauterine pregnancy, should continue to warrant the consideration of heterotopic pregnancy as a differential diagnosis.
Conclusion/Learning points
This case report emphasizes that the list of differential diagnoses should be kept broad and excludes heterotopic pregnancy in the first trimester in a pregnant woman presenting with abdominal pain and hemodynamic instability. A teamwork approach involving multiple specialties is often necessary for the management of patients with an uncertain diagnosis.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Heterotopic pregnancy; Acute abdomen; Hemorrhagic shock; Hemoperitoneum; Salpingectomy
Cite this article
Fahim M, James A, Gandhi H, Thumber N, Bradshaw C, Szekeres C. Ruptured Heteroptopic pregnancy: A surgical emergency with an uncommon cause. Clin Case Rep J. 2021;2(6):1–4.
Copyright
© 2021 Muhammad Fahim. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).