Smiling at Low Cost: An Alternative to Traditional Vestibuloplasty
* Amin Soolari;
-
* Amin Soolari: Department of Dentistry, Soolari Dentistry, Maryland 20854, United States.
-
Mar 31, 2022 |
-
Volume: 3 |
-
Issue: 3 |
-
Views: 3416 |
-
Downloads: 2005 |
Abstract
A 60-year-old patient presented for complete maxillary and mandibular dentures following extractions and alveolar bone remodeling. However, once the extractions and alveoloplasty were complete, the lack of depth or width of the alveolar ridge precluded the placement of a quality mandibular denture following the conventional protocol. A modified treatment technique was therefore created to enable a complete mandibular denture. A full-thick flap had been laid from mandibular premolar to premolar, the papillae were intact following extractions, and an adequate tissue length was retained. Therefore, the flap was released past the mucogingival junction, allowing for greater mobility and therefore the use of an absorbable suture to stabilize the mobile buccal periosteum by moving the suture in a lingual and inferior direction, coming out from the lip periosteum using the mentalis muscle via simple interrupted sutures. The remaining free papillae were sutured to stabilize them back into orientation and create the desired scaffold for regeneration. This retained the original vestibule depth, enabling scaffolding for new tissue. In addition, the technique preempted the need for a stent to keep the tissue in place, similar to a traditional vestibuloplasty, which enables less plaque retention and better patient comfort while reducing the resorption experienced during the healing process. Following the traditional method of extraction and alveoloplasty, in this case, would have resulted in a poor treatment outcome, owing to a lack of ridge for mandibular seating dentures. This modification improves the prognosis and enables future treatment options while minimizing the extent of anticipated surgeries.
Introduction
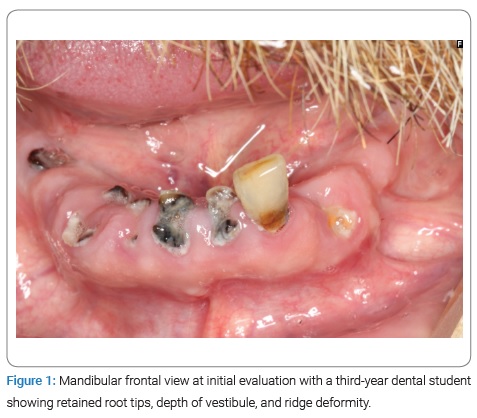
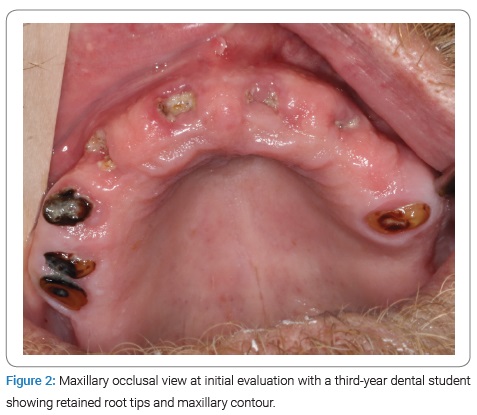
A 60-year-old male presented to the oral surgery department of the University of Maryland School for Dentistry for multiple tooth extractions and alveoloplasty in preparation for dentures. Clinical and radiographic evaluation disclosed numerous problems, including poor oral hygiene, missing teeth, ridge deformity, tooth migration, broken teeth, retained root tips, generalized severe chronic periodontal disease, teeth with endodontic involvement, severe caries, exposed dentin, loss of vertical dimension, non-restorable teeth, horizontal and vertical bone loss, poor crown-to-root ratio, and collapsed occlusion. After a general dental and prosthodontic consultation, the patient agreed to extract all existing teeth, followed by delivery of full upper and lower dentures. Medical history included a heart murmur diagnosed in 2019 and treated by reduced caffeine intake and borderline hyperlipidemia, for which the patient was put on atorvastatin for one month. In addition, the patient was taking aspirin (81 mg) for stroke prevention and had previously been treated with glecaprevir and pibrentasvir for hepatitis C from 2017 to January 2020, when the viral count became undetectable. The patient was also taking gabapentin daily for pain in his feet from an episode of frostbite sustained in 2017, had a history of alcohol abuse for 47 years (currently sober), and was a current tobacco user (one pack a day) and allergic to penicillin.
The patient stated that he brushed his teeth only three times a week because of the associated discomfort and had a family history of cardiovascular conditions, tobacco use, congenital heart defects, and liver failure. Extraoral and intraoral parameters were all within normal limits, except for a small cyst on the right side of the neck that the patient stated had been there for the past 20 years, a 7 mm × 7 mm single pink, raised, smooth but firm plaque on the mid dorsum of the tongue, and a 7 mm single inward deviation on the anterior palate of the mouth, possibly from the cleft palate or resorption.
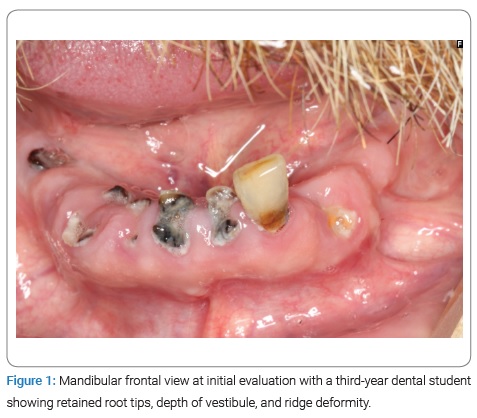
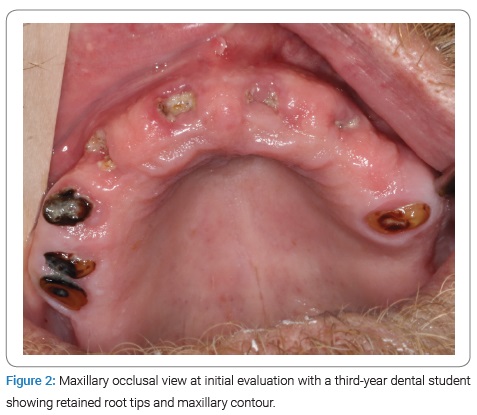
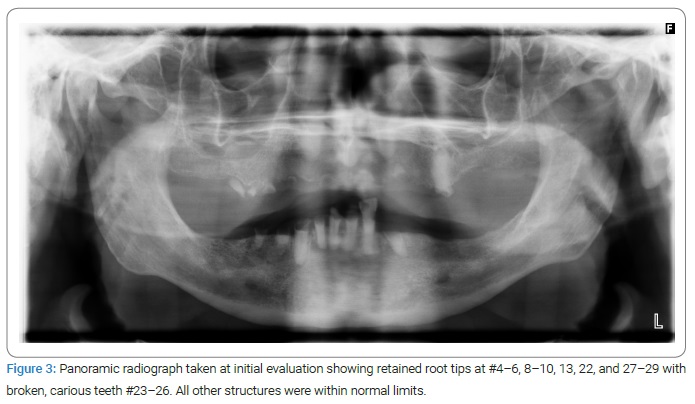
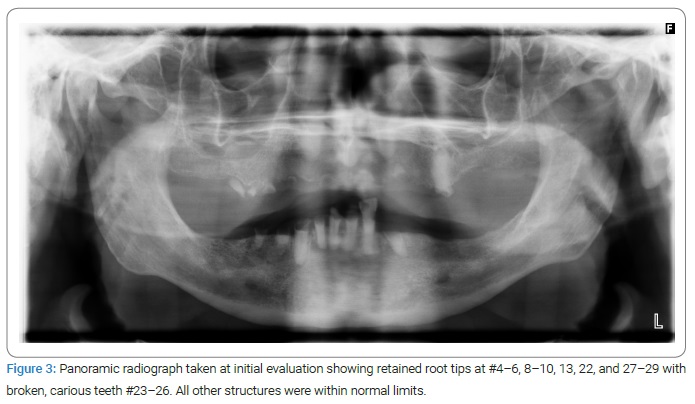
The patient had severely carious, non-restorable teeth, retained root tips, and ridge deformity (Figure 1–Figure 3). The treatment options presented to the patient were full-mouth extractions and alveoloplasty for future complete maxillary and mandibular dentures or full-mouth extraction with a variation of implant-retained overdenture or hybrid dentures. Because of financial concerns, the patient elected conventional complete dentures and consulted with his primary care physician regarding tobacco cessation, liver function, contraindications to local anesthesia with epinephrine for surgical procedures, and bloodwork to determine coagulation ability. The physician confirmed the patient’s hemodynamic stability and no contraindication for the use of epinephrine, clearing the patient for extractions and alveoloplasty. A prosthodontist then took alginate impressions of the maxilla and mandible and created surgical reduction guides after the ideal reduction of undercuts made on casts. The overall treatment plan for the patient was complete maxillary and mandibular dentures following extractions and alveolar bone remodeling. However, once the extractions and alveoloplasty were complete, the defect on the mandible left no depth or width of an alveolar ridge for a mandibular denture following the conventional protocol. A modified treatment technique was therefore created to enable a complete mandibular denture.
Case Presentation
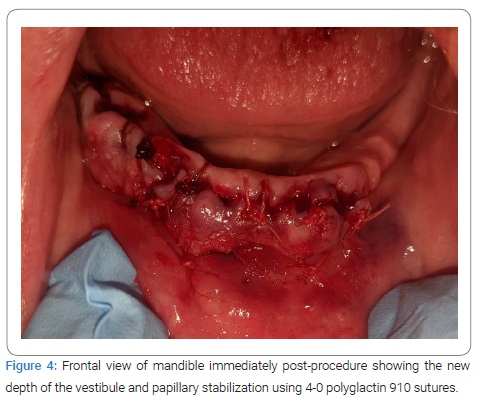
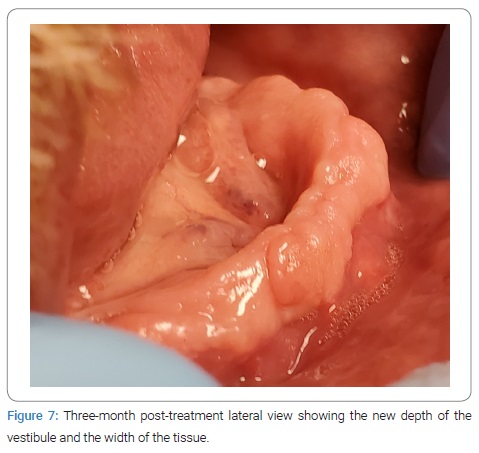
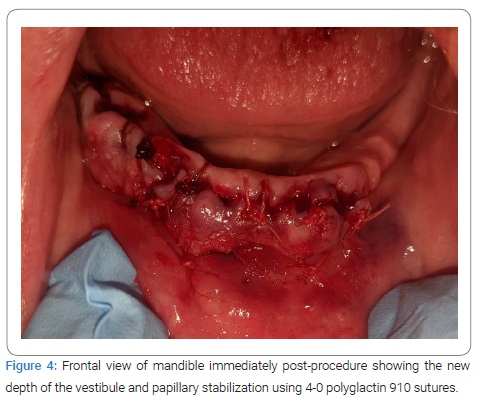
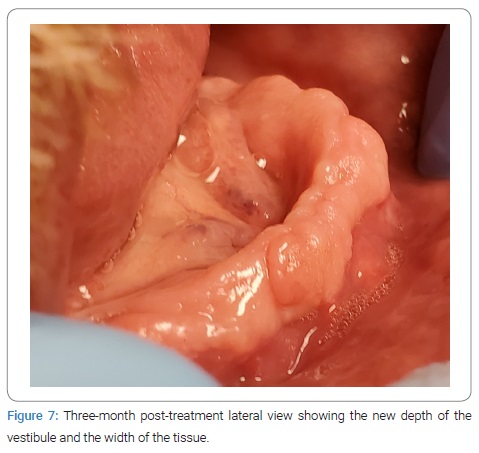
The patient presented for extraction of all remaining teeth with alveoloplasty to remove undercuts, particularly on the maxilla in the maxillary right premolar region area. A full-thickness, non-displacing, papilla-preserving flap was made using a mid-crestal incision with a 15c blade followed by simple extraction. Alveoloplasty was completed using a mucoperiosteal flap, undercuts, sharp ridges, and infected tissue was removed by a combination of rongeurs, a bone file, 84-T/XF taper, and a fine-cut titanium nitride-coated carbide bur with the handpiece. The lack of depth or width of the alveolar ridge for a mandibular denture presented a problem; however, a full-thickness flap had been laid from mandibular premolar to premolar, the papillae were intact following extractions, and an adequate length of tissue was retained, so a modified procedure was performed instead to enable the fabrication of a complete mandibular denture. The flap was released past the mucogingival junction, allowing for greater mobility and therefore the use of an absorbable 4-0 polyglactin 910 suture to stabilize the mobile buccal periosteum by moving the suture in a lingual and inferior direction, coming out from the lip periosteum using the mentalis muscle via two simple interrupted sutures in the lower canines. The simple interrupted method of remaining free papillae was sutured to stabilize them back into orientation and create the desired scaffold for regeneration. This retained the original vestibule depth, enabling scaffolding for new tissue by primary and secondary healing intentions (Figure 4, Figure 5). The patient presented for a 1-week follow-up with generalized erythema and soreness and was prescribed clindamycin (300 mg) q.i.d. for ten days. At the 1-month follow-up, no signs of inflammation were noted, and the vestibular sutures were removed. The patient then presented at three months for additional alveoloplasty, where the full extent of the treatment outcome was observed (Figure 6, Figure 7).


Discussion
Conventional treatment in the dental community is to remove teeth and allow a normal healing process when socket preservation or ridge augmentation is not done. At best, a clinician may attempt to gain primary closure of the socket by removing crestal bone and papillae or compressing buccal and lingual bone to reduce the buccal-lingual dimension of the ridge. This results in a shallow mandibular vestibule that is not conducive to the placement of a functional prosthesis. A traditional vestibuloplasty was not indicated, as the initial incision began mid-crest of the mandibular ridge with a full-thickness flap, preventing a supraperiosteal extension in the vestibule to suture the tissue to the periosteum of the mandible. In addition, a transpositional flap technique (lip switch) was not indicated because of the initial incision, as this technique is stringent on the initial semi-lunar incision to allow for the extension of the vestibule and mucosal flap to cover the exposed periosteum [1]. Extensive ridge augmentation and free autogenous gingival grafts for guided tissue regeneration are alternative treatment options but can be expensive. The case required a personalized and predictable course of treatment that yielded a denture-bearing surface for prostheses; we used a modified vestibuloplasty and coronal advancement of the entire zone of attached gingiva from the mucogingival junction. This technique deepened the vestibule and increased the zone of the attached gingiva to induce the accumulation of tough, resilient, attached, and keratinized gingiva that will resist traumatic friction between the prosthesis and alveolar ridge and increase the patient’s quality of life. The technique achieved the desired outcome for both patient and practitioner at a low cost. It preempted the need for a stent to keep the tissue in place, similar to a traditional vestibuloplasty, enabling less plaque retention and better patient comfort while reducing the resorption experienced during the healing process [2].
Chronic smoking can modulate inflammatory and cellular repair functions by decreasing blood flow and delaying healing [3]. Full-mouth tooth extractions and alveoloplasty for future complete-over-complete dentures can have unforeseeable consequences, and complex medical history can render even successful treatments unpredictable. A practitioner familiar with treatment options that prepare effectively and take the patient’s medical history and histology into account can reduce costs and improve patient satisfaction. Tissue quality, height, and width all assist in providing a functional and esthetic prosthesis with good plaque control [4]. A prospective 3-year clinical study of masticatory function in patients with conventional dentures and mandibular overdentures reported better function in participants with mandibular implant-stabilized overdentures rather than complete dentures [5]. Adequate attached gingiva in a fixed prosthesis enables an esthetic appearance, prolonged use of the prosthesis, and good oral hygiene practices. However, vestibuloplasty is required to deepen the maxillary and mandibular vestibule in preparing for a prosthesis, whether fixed or removable [6]. Histological attached gingiva have collagenous fiber bundles connected to the mucous membrane of bone, and the alveolar mucosa is smooth and loosely bound to the underlying periosteum; the mucogingival junction separates the two [7].
Tissue healing occurs in three stages: Inflammation, proliferation, and remodeling [8]. During the inflammatory stage, initial vasoconstriction, and platelet activation occur to stop bleeding. Platelet activation produces vasoactive mediators and chemotactic factors that signal inflammatory cells. Vasodilation enables neutrophil and leukocyte transmigration as a primary defense, followed by granulocyte and macrophage action to remove debris and produce collagenase and lactase for proper healing. The proliferative stage involves the formation of granulation tissue (macrophages, fibroblasts, capillary networks, fibronectin, hyaluronic acid, and endothelial cells), which causes hypoxia and initiates angiogenesis and neovascularization. The final stage of healing is the formation of collagen from fibroblasts and other progenitor cells into myofibroblasts to provide matrix constriction [9]. These factors must be considered when formulating a treatment plan that would provide long-term predictable and functional outcomes. The goal, in this case, was to focus on generating abundant soft tissue to support the prosthesis affordably despite the patient’s complex medical history.
Following the traditional method of extraction and alveoloplasty, in this case, would have resulted in a poor treatment outcome, owing to a lack of ridge for mandibular seating dentures. This modification improves the prognosis: The patient now has an abundance of attached and mucosal gingiva to allow for a functional and esthetic prosthesis and future treatment options such as implant-retained overdentures or hybrid prostheses minimizing the extent of future surgeries. Despite the additional alveoloplasty required in the mandible, the available tissue allows for more options and better outcomes.
Conclusion
The technique described in this article deepened the patient’s vestibule, created abundant soft tissue, simplified treatment, and healing, and assured that the patient would have present and future treatment options that were more affordable than conventional methods.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Wessberg GA, Hill SC, Epker BN. Transpositional flap technique for mandibular vestibuloplasty. J Am Dent Assoc. 1979;98(6):929–933.
- Ephros H, Klein R, Sallustio A. Preprosthetic Surgery. Oral Maxillofac Surg Clin North Am. 2015;27(3):459–472.
- Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069–1079.
- Mishra N, Singh BP, Rao J, Rastogi P. Improving prosthetic prognosis by connective tissue ridge augmentation of alveolar ridge. Indian J Dent Res. 2010;21(1):129–131.
- Khalid T, Yunus N, Ibrahim N, Saleh NBM, Goode D, Masood M. Assessment of masticatory function of mandibular implant-supported overdenture wearers: A 3-year prospective study. J Prosthet Dent. 2020;124(6):674–681.
- Natarajan S, Banu F, Kumar M, Lavu V. Management of shallow vestibule with reduced attached gingiva in fixed prosthetic intervention. Cureus. 2019;11(6):e4975.
- Ochsenbein C. Newer concept of mucogingival surgery. J Periodontol. 1960;31(3):175–185.
- Gonzalez AC, Costa TF, Andrade ZA, Medrado ARAP. Wound healing - A literature review. Anais brasileiros de dermatologia. 2016;91(5):614–620.
- Politis C, Schoenaers J, Jacobs R, Agbaje JO. Wound healing problems in the mouth. Front Physiol. 2016;7:507.
Keywords
Vestibuloplasty; Alveoloplasty; Mandibular denture
Cite this article
Soolari A. Smiling at low cost: an alternative to traditional vestibuloplasty. Clin Case Rep J. 2022;3(3):1–5.
Copyright
© 2022 Amin Soolari. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).