Treatment of Postoperative Non-Healing Wound with Fire Needle Therapy: A Case Report
Pei Yu;
Yuanbo Fu;
Bo Li;
Guilin Liu;
Tao Zhang;
Yan Anna;
* Bin Li;
-
Pei Yu: Department of Acupuncture and Moxibustion, Beijing University of Traditional Chinese Medicine, Beijing 100029, China.
-
Yuanbo Fu: Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Beijing 100010, China.
-
Bo Li: Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Beijing 100010, China.
-
Guilin Liu: Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Beijing 100010, China.
-
Tao Zhang: Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Beijing 100010, China.
-
Yan Anna: Department of Acupuncture and Moxibustion, Beijing University of Traditional Chinese Medicine, Beijing 100029, China.
-
* Bin Li: Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Beijing 100010, China.
-
Apr 19, 2022 |
-
Volume: 3 |
-
Issue: 3 |
-
Views: 5425 |
-
Downloads: 2458 |
Abstract
Case summary: A 67 elderly female patient suffered from a postoperative non-healing wound after craniocerebral trauma surgery, and effective debridements and local anti-infection therapies were tried, but the effectiveness was limited. An adapted fire needle therapy was tried. The fire needle therapy used was divided into two stages. In the 1st stage, a thick fire needle was used once a day for four days, four times total. During the 2nd stage, a thin fire needle was adopted once every other day for six days, three times in total. After receiving the fire needle treatment for two weeks, a total of 7 times, the wound healed, and the patient recovered successfully without adverse events.
Conclusion: Considering the significant efficacy of fire needles and the absence of side effects in this patient, it is believed that fire needles could be a possible treatment for patients of postoperative non-healing wounds with no healing tendency after local debridement anti-infection treatment and complimentary replacement therapy. We report this case, hoping to provide a new idea for postoperative non-healing wounds.
Core Tip
A patient suffered from a postoperative non-healing wound after craniocerebral trauma surgery, and effective debridements and local anti-infection therapies were tried, but the effectiveness was limited. Therefore, an adapted fire needle therapy was tried. After receiving fire needle treatment for two weeks, a total of 7 times, the wound healed, and the patient recovered successfully. Considering the significant efficacy of fire needles and the absence of side effects, it is believed that fire needles could be a possible treatment for patients of postoperative non-healing wounds with no healing tendency after local debridement, anti-infection treatment, and complimentary replacement therapy.
Practice Points
- The postoperative non-healing wound is a common complication after surgery which is difficult to deal with.
- Due to repeated infection and long-term healing characteristics, the effectiveness of traditional therapy is sometimes limited, and the wound needs special treatment.
Introduction
A non-healing wound is any kind of wound that cannot be repaired and achieve an anatomically and functionally complete state normally [1]. Postoperative non-healing craniocerebral trauma wound has a long treatment period, easy recurrence, and has a high disability rate, which brings mental and economic pressure to patients and their families [2]. Meanwhile, it consumes a lot of medical resources.
Currently, some therapies are used in wound healing, including ultrasound or biological debridement [3,4], anti-infective dressing [5], negative-pressure wound therapy [6], and growth factor therapy [7]. However, some therapies are more suitable for hospitalized patients but not convenient for a clinical environment, so the clinical application is limited. Moreover, the effect of these treatments is sometimes limited too.
Fire needle therapy was first described in the Yellow Emperor’s Canon of Internal Medicine (475 BC–221 BC) over 2000 years ago, which was one of the alternative therapies of traditional Chinese medicine and a branch of acupuncture. Fire needle therapy has unique advantages in promoting wound healing and is often used in China for clinical wounds management. However, it has not been widely recognized in the rest of the world.
Case Presentation
Chief complaints: A 67-year-old female patient suffered from a postoperative non-healing wound after craniocerebral trauma surgery.
History of present illness: In 2016, the patient suffered from craniocerebral trauma due to a car accident and underwent decompressive craniectomy, followed by an implanted titanium alloy bone plate to maintain skull stability. Six months ago, a repeated scalp infection appeared where the left titanium mesh was placed, and the local skin was ruptured. The patient received continuous local dressing changes and debridement, but the wound still failed to recover. On October 28, 2020, the patient underwent debridement and titanium mesh removal. After the operation, the patient’s head wound remained unhealed, and a series of surgical dressing changes, chemical local wet compress, and physical replacement therapy did not work at all.
Personal and family history: No data was available.
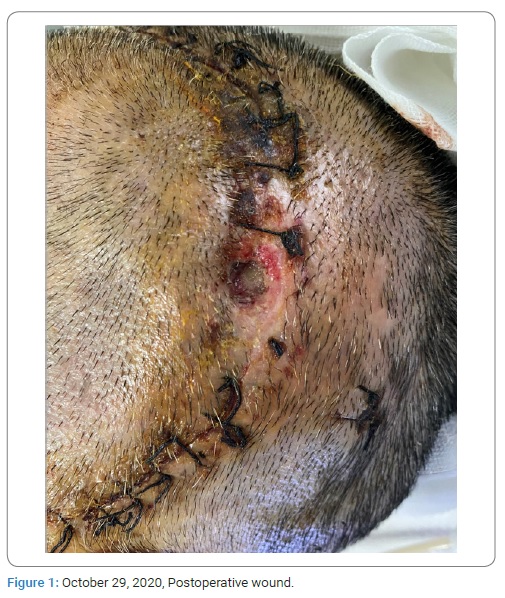
Physical examination: A 1.8 cm x 1.1 cm oval unhealed wound could be seen on the left side of the patient’s head (Figure 1). The blood supply of the skin flap around the wound was poor, the color was pale, and there was no obvious exudation. The skin temperature of the wound’s local tissue was slightly higher, and the tenderness was obvious.
Laboratory examinations: October 29, 2020, Whole blood cell analysis: leukocyte count was in the normal range (the leukocyte count is 8.74 x 10^9/L, and the normal range is 4.0–10.0 x 10^9/L), the percentage of neutrophils increased (the percentage of neutrophils is 75.5%, and the normal range is 50%–70%), and C-reactive protein increased (the C-reactive protein is 10.08 mg/L, and the normal range is 1.0–10.0 mg/L). October 29, 2020, Glycated hemoglobin is 5.9% (the normal range is 4%–6%).
Imaging examinations: Changes after skull repair.
Final diagnosis: Diagnosis: Non-healing wound, wound infection; Prognosis: Poor.
Treatment: Intervention before fire needle therapy (October 29, 2020–November 14, 2020): According to the TIME (tissue nonviable, infection/inflammation, moisture, edge) principle of clinical wound care [8], effective debridement and local anti-infection therapy had been applied:
- Debridement and surgical dressing: the local necrotic tissue was removed, and the wound was covered with 0.5% diluted iodophor. The dressing was changed every day until the wound no longer exuded and removed the necrotic tissue. After that, the dressing could be changed every 2 days–3 days.
- Anti-infection wet compress: 1% Bromogeramine was used for local disinfection, and then local wet compress with Raceanisodamine Hydrochloride injection were applied. As long as the wound continued, exudate 0.16% gentamicin was applied externally to prevent infection.
- Oxygen spray therapy and ozone disinfection water washing therapy: 75% alcohol was added into the oxygen humidification bottle, and a No. 14 catheter was used to spray oxygen on the wound. Oxygen flows 9 L/min for 15 minutes once a day. Meanwhile, an ozone disinfectant water spray tank with a concentration of more than 6 mg/L was used to rinse the wound once a day.
Laboratory examinations: November 11, 2020, Whole blood cell analysis: leukocyte count was in the normal range (the leukocyte count is 9.65 x 10^9/L), the percentage of neutrophils increased slightly (the percentage of neutrophils is 75.7%), and C-reactive protein was normal (the C-reactive protein is 7.3 mg/L).
The patient still has an obvious headache and no wound healing tendency, and the wound on the local scalp changes are not as obvious compared with the previous one. Hence, the patient began to accept fire needle therapy from November 15, 2020.
Fire needle therapeutic intervention (November 15, 2020–November 25, 2020): Based on the original local dressing change, fire needle therapy was added. The fire needle therapy was divided into two stages.
A thick fire needle was used in the 1st stage (once a day for four days, four times in total). Disinfection was performed on the edge of the wound with iodophor and deiodinated with 75% alcohol. A 1.1 mm diameter fire needle was used, and the needle tip and the lower section of the needle body were placed at the outer flame of the alcohol lamp for heating until it turned red. Then it was quickly pricked at the skin flap interspersed throughout the area 4 mm–5 mm from the wound, with a depth of about 2 mm–3 mm, and then quickly removed. The whole process of pricking and removing is about 1 second, and the time of contacting human skin is about 0.1 seconds–0.3 seconds. Prick eight needles on the skin flap 4 mm–5 mm around the wound per time. A small amount of congestion is released to eliminate the blockage and promote blood circulation. Precautions: Pay attention to avoid the wound’s inner edge injuries during fire needle therapy.
The 2nd stage (once every other day for six days, three times in total) adopted a 0.5 mm thin fire needle. Disinfection was performed, and both the needle tip and the lower section were heated to red, similarly to the method used with the thick fire-heated needle. Then the thin needle was quickly pricked to the inner skin edge of the wound, with a depth of about 1 mm–2mm, and quickly removed. The whole process of pricking and removing is about 1 second, and the time of contacting human skin is about 0.1 seconds–0.3 seconds. Prick six needles on the inner skin edge of the wound per time. The aim was to remove necrotic tissue, promote the growth of new granulation tissue and accelerate wound healing.
Ethics and Informed Consent: This case report does not involve the patient’s personal information and privacy. The patient informed and agreed to publish the case as a case report.
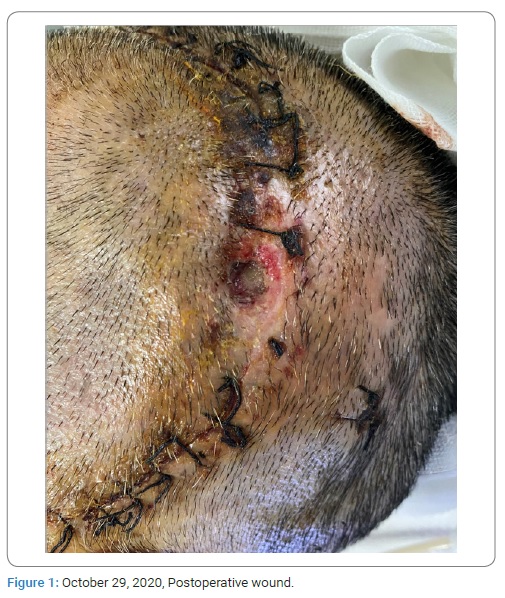
Outcome and follow-up: Two weeks later, after fire needle therapy, the patient reported that the degree of headache decreased, and the tendency of wound healing was obvious (Figure 2).

November 29, 2020, Whole blood cell analysis: leukocyte count, the percentage of neutrophils and CRP was normal (WBC 7.37 x 109/L, NEUT%, 67.3%, CRP 7.1 mg/L). After three months’ follow-up, the patient had no headache and the wound healed well.
Discussion
The postoperative non-healing wound can be divided into the patient’s own condition factors and local wound factors. The self-condition factors include body immunity, nutrition, etc. Local factors include poor blood circulation, poor drainage, and local infection. Studies have shown that biofilm infection exists in 75%–90% of chronic wounds. Therefore, chronic wound infection caused by bacterial biofilm has become the focus of wound management [9,10]. The patient in our case presented with the wound repeatedly infected and poor peripheral blood supply. The fire needle was applied to control infection by improving local blood circulation and regulating inflammation.
The fire needle is made of tungsten alloy, and burning is the key modality in this treatment. The needle must be heated until it turns red and then quickly pricked into the acupoints or parts of the human body and quickly removed. Research shows that the maximum temperature of the needle can reach 8000C after burning to red, and when pricking into the skin after 1 second, the temperature is close to 3000C [11]. The whole process of pricking and removing is about 1 second, and the time of contacting human skin is about 0.1 seconds. With strong penetration power and low resistance to the skin, a fire needle shortens the procedure’s time and reduces patients’ pain. In China, fire needle therapy is often used in clinical skin diseases, fascia and muscle diseases, orthopedic diseases [12]. Studies have also shown that fire needles can improve local blood circulation, localized inflammation and regulate immunity [13–20], which may have a benign inducing effect on promoting wound healing.
Fire needle therapy stimulates acupoints and has a moxibustion effect simultaneously, with the effect of promoting the circulation of blood. In the clinical study of knee osteoarthritis treated with fire needle therapy, it is found that fire needles can improve the hemodynamic state, hemorheology, and microcirculation around the knee [13]. Clinical studies have also shown that fire needle treatment’s high temperature destroys inflammatory lesions and accelerates wound healing and exudation, promoting blood circulation and metabolism leading to tissue regeneration [14,20].
Fire needles can localize the inflammation and accelerate the skin barrier repair. Studies have shown that fire needles can mediate and limit inflammatory response by reducing serum interleukin-1 [15]. In the clinical application of treating skin diseases, fire needles can enhance the blood supply in local skin lesions, promote leukocyte exudation, and improve its phagocytic function to help the inflammation subside and localize the inflammation [16].
Fire needle can regulate immunity and promote wound healing, and it is often used as a treatment for non-healing wounds after operation in China [18]. Animal studies show that fire needles can effectively promote the necrosis and liquefaction of wound lesions in bedsore mice, stimulate self-regulation mechanism, and release vascular endothelial growth factor (VEGF) and other growth factors to promote the growth of granulation tissue and accelerate healing [17]. In addition, a study of non-healing wounds after gynecological laparoscopic surgery treated with a fire needle showed that fire needle could trigger a local inflammatory reaction, enhance non-specific immune defense functions, improve the number and phagocytic ability of phagocytes, and further promote wound healing [18,19].
Advantages and Limitations: Currently, there are few case studies of a postoperative non-healing wound treated by fire needle therapy internationally. Fire needle is often used to promote postoperative wound healing in China, with significant efficacy. In this case, before receiving fire needle therapy, the patient adopted debridement, local dressing change, and complimentary replacement therapy, but none of these methods worked. Within two weeks after receiving fire needle therapy, the wound started improving and gradually healed. Indeed, though the wound healing tendency was obvious and no adverse events existed during fire needle therapy, we did not leave histological evidence to provide accurate histological information of wound healing.
Conclusion
This patient’s fire needle therapy led to substantial improvement of the postoperative non-healing wound. However, as a branch of acupuncture, fire needle has not been widely recognized globally. There are still few studies on fire needles in promoting wound healing. The investigators report this case in the hope of providing a new idea for the postoperative non-healing wound.
Acknowledgments
Author contributions: Pei Yu is responsible for writing the manuscript. Yuanbo Fu, Guilin Liu and Tao Zhang is responsible for collecting and providing patient information. Bo Li is responsible for providing critical comments; Yan Anna is responsible for polishing and modification of language. Bin Li is responsible for proofreading and providing critical comments on the final draft.
Funding: This work was supported by the National Key Research and Development Plan (2019YFC1709703).
Informed consent: A written informed consent was provided by the patient of the case to publish the case details and associated images.
Informed consent statement: All study participants have provided informed written consent prior to study enrollment.
CARE checklist statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Lau J, Tatsioni A, Balk E, Chew P, Kupelnick B, Wang C, et al. Usual care in the management of chronic wounds: A review of the recent literature [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). 2005.
- Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17(6):763–771.
- Magalhaes L, Martins SRP, Nogue R. The role of point-of-care ultrasound in the diagnosis and management of necrotizing soft tissue infections. Ultrasound J. 2020;12(1):3.
- Sherman RA. Maggot therapy for treating diabetic foot ulcers unresponsive to conventional therapy. Diabetes Care 2003;26(2):446–451.
- Xuan X, Zhou Y, Chen A, Zheng S, An Y, He H, et al. Silver crosslinked injectable bFGF-eluting supramolecular hydrogels speed up infected wound healing. J Mater Chem B. 2020;8:1359–1370.
- Alga A, Haweizy R, Bashaireh K, Wong S, Lundgren KC, von Schreeb J, et al. Negative pressure wound therapy versus standard treatment in patients with acute conflict-related extremity wounds: a pragmatic, multisite, randomised controlled trial. Lancet Glob Health. 2020;8(3):e423–e429.
- Zhang Y, Wang T, He J, Dong J. Growth factor therapy in patients with partial-thickness burns: a systematic review and meta-analysis. Int Wound J. 2016;13:354–366.
- Leaper DJ, Schultz G, Carville K, Fletcher J, Swanson T, Drake R. Extending the TIME concept: what have we learned in the past 10 years?(*). Int Wound J. 2012;9 Suppl 2(Suppl 2):1–19.
- Kucisec-Tepes N. [The role of antiseptics and strategy of biofilm removal in chronic wound]. Acta Med Croatica. 2016;70(1):33–42.
- Hurlow J, Blanz E, Gaddy JA. Clinical investigation of biofilm in non-healing wounds by high resolution microscopy techniques. J Wound Care. 2016;25 Suppl 9(Suppl 9):S11–S22.
- North China Electric Power University. Temperature measurement and numerical simulation of the fire needle [Internet]. Beijing: CNKI; 2013.
- Li BY, Jia CS, Wang JL, Tan ZN, Zhu XL, Shi J, et al. [Diseases treated by moxibustion and fire needling in clinical practice based on data mining: a comparison study]. Zhongguo Zhen Jiu. 2014;34(11):1093–1097.
- Bin Li, XC Xie, LP Wang. Clinical observation of fire-heated needle in the treatment of knee osteoarthritis. Journal of Traditional Chinese Medicine. 2011;30:923–924.
- SR Cai. Treatment of 32 cases of postoperative non-healing wound with fire-heated needle. Henan Traditional Chinese Medicine. 2003.
- Han RX, Yang J, Zhang TS, Zhang WD. [Effect of fire-needle intervention on serum IL-1 and TNF-alpha levels of rheumatoid arthritis rats]. Zhen Ci Yan Jiu. 2012;37(2):114–118.
- PW Wu, Shu Huang. Study on the mechanism of fire-heated needle in the treatment of acne. Chinese Journal of Ethnomedicine and Ethnopharmacy. 2010;10:13–15.
- Zhang LR, Yan CL, Wang YX, Jiang YR, Wang HH, Sun RJ. Expression and effect of vascular endothelial growth factor in the wound surface in fire-heated needle treatment of bedsore mice. Shanghai Journal of Acupuncture and Moxibustion 2012;31:606–608.
- C Yang, Y Qin, Z Zhuang, W Yi. Effects of fire-heated needle therapy on wound healing after gynecological laparoscopy. Journal of Shandong University of Traditional Chinese Medicine. 2018;42:150–152.
- HX Guo, G Liu. Analysis of the efficacy of annular drainage with electric pyropuncture needle therapy combined with blocking therapy in treatment of patients with perifolliculitis capitis abscedens et suffodiends. Tianjin Journal of Traditional Chinese Medicine. 2016;33:541–544.
- Wang H, Gu Y, Huang L, Zeng Z, Hu X, Wang X, et al. Effectiveness of fire needle combining with moist healing dressing to promote the growth of granulation tissue in chronic wounds: A case report of new study. Int J Nurs Sci. 2020;7:386–390.
Keywords
Wound healing; Postoperative wound; Fire needle; Case report; Complementary replacement therapy
Cite this article
Yu P, Fu Y, Li B, Liu G, Zhang T, Anna Y, et al. Treatment of postoperative non-healing wound with fire needle therapy: A case report. Clin Case Rep J. 2022;3(3):1–5.
Copyright
© 2022 Bin Li. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).