Abstract
Objectives: Present a clinical case of C1 Jugulotympanic Paraganglioma (JTPG), emphasizing treatment decision and surgery planning to improve and optimize timing and result.
Case Presentation: 52-year-old woman with left JTPG Fish´s C1 with genetic study positive for succinate dehydrogenase type B gene mutation (SDHB). Treatment of the paraganglioma with radiotherapy options or surgery was proposed. A surgical approach was decided based on age, tumor pathophysiology, and staging. Surgery planning was done in the anatomy department, and tumor exeresis was performed using type A Infra Labyrinthine (ITFA) and a cervical combined approach with facial mobilization.
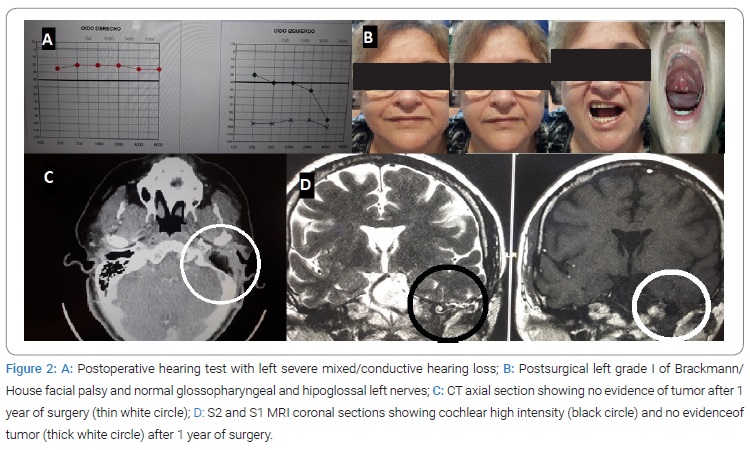
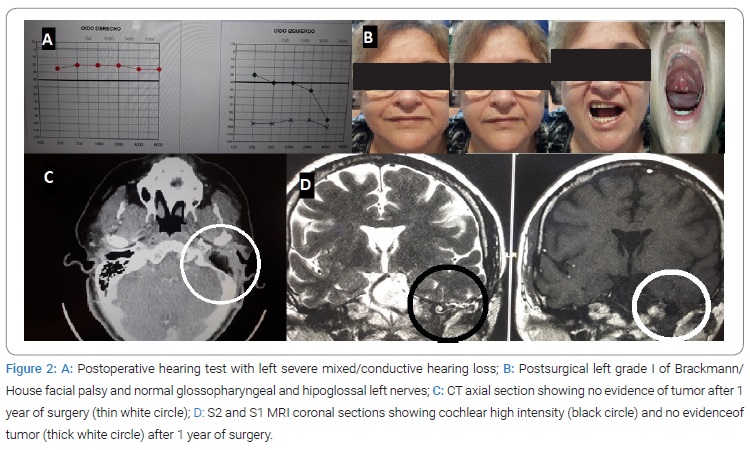
Results: The patient is disease-free at controls after 12 months with surgical sequelae of facial palsy grade II and moderate mixed hearing loss.
Discussion: JTPG treatment requires individualized indication, depending on age and risk/benefit balance. Classically surgery was the choice treatment, but there are good results in tumor control with radiotherapy modalities, but with a high percentage of regrowing after ten years; therefore, surgery indication is adequate for non-elderly patients with malignancy risk. Surgery requires planning for correct timing steps, tumor embolization, and complication control.
Conclusions: ITFA cervical combined approach with facial rerouting was a good surgery choice to treat this case of JTPG C1. This approach allowed correct tumor removal with expected sequelae, with correct planning and preparation to improve patient prognosis, quality of care, and surgical outcomes.
Abbreviation
ASA: American Society of Anesthesiologists (Physical Status Classification System); CT: Computed Tomography; ITFA: Infra-Temporal Fossa Approach; JTPG: Jugulo-Tympanic Para-Ganglioma; SDH: Succinate Dehydrogenase; MRI: Magnetic Resonance Imaging; PG: Paraganglioma; PET: Positron Emission Tomography; PTH: Parathyroid Hormone
Introduction
Paraganglioma (PG) is a tumor derived from the paraganglia of the autonomic nervous system of the adventitial layer of blood vessels. Its incidence is 1 in 30,000 to 100,000, where 60% are carotid body tumors, 40% jugulotympanic and less than 5% vagal [1–3]. They can be catecholamine-producing tumors with local aggressiveness (2% to 5% malignant); their presentation can be sporadic or familial, with multifocality of 10 to 50%–80%, respectively, in entities such as multiple endocrine neoplasias (II A–B), von-Hippel-Lindau syndrome and type 1 neurofibromatosis. The genes described in PG 1 to 5 syndromes are SDHD (11q23), SDHAF2 (11 or f79), SDHC (1q21), SDHB (1p36.1p35), and SDHA (5p15.33) respectively [1,4,5]. Its diagnosis is clinical and radiological, requiring a multidisciplinary approach due to its complexity [6–9]. The modified Fish classification allows planning of the appropriate surgical approach [1,10]. We report a case treated by our department using type A infratemporal combined with a cervical approach.
Case Presentation
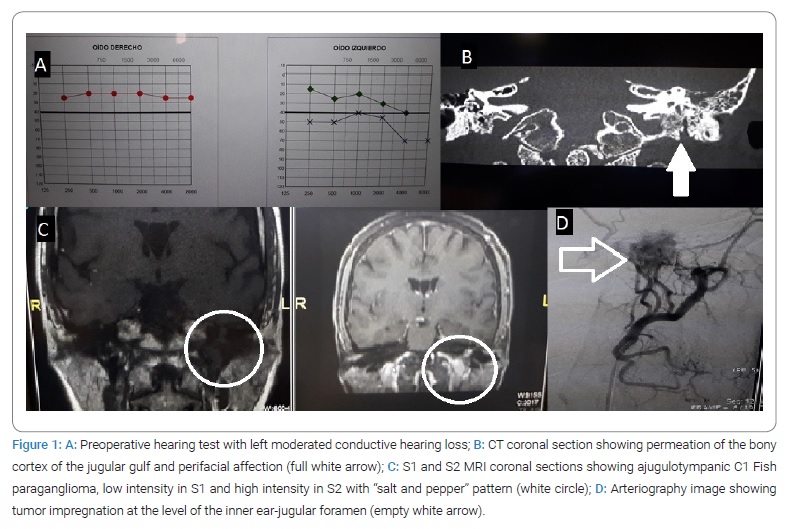
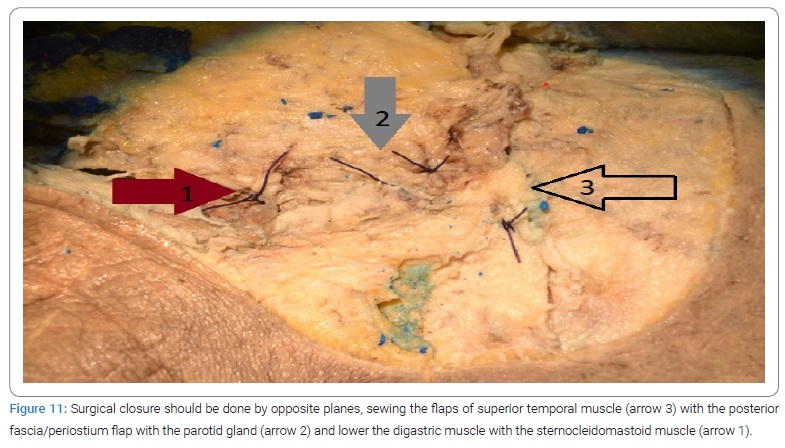
A 52-year-old woman with hearing loss, pulsatile tinnitus, autophonia of many years of evolution, paroxysmal dysphonia, and sialadenitis. Her pathological history revealed active smoking, type 2 diabetes with regular control, uterine fibroid surgery, allergy to acetylsalicylic acid, with three healthy daughters; On otoscopy examination, she presented a hyperemic middle ear mass with the intact tympanic membrane. Initial high-resolution CT scan reported: “a complete occlusion of the mastoid cells and the left middle ear, no bone erosions are identified in the medial wall, tegmen or in the wall spur, there is no permeative pattern in the jugular bulb; small microcalcifications are seen in the tissue that fills the middle ear. The radiological findings are more consistent with chronic otitis media. There is a mass in the sella turcica with erosion on the right side of the clivus, and the lesion enters the right sphenoid sinus. The findings are consistent with an invasive pituitary macroadenoma. Radiological diagnosis: Probable chronic left otitis media. Moreover, invasive pituitary macroadenoma”. A posterior exam of the ear and pituitary MRI reported that: “the tumor is located in the promontory hypo tympanum of the left ear, which is introduced at the beginning of the internal jugular vein. After reviewing the previous CT study, permeation of the bony cortex of the jugular bulb was observed, consistent with the extension of a jugulotympanic glomus. There is no growth towards the posterior fossa. Radiological diagnosis: left jugulotympanic paraganglioma Fish C1. A right pituitary macroadenoma with the invasion of the sphenoid sinus is appreciated. The lesion measures 18 mm x 17 mm and is lateralized to the right. Cranially it does not reach the optic chiasm, and laterally it exceeds the right internal carotid, Knosp III. Radiological diagnosis: pituitary macroadenoma”. Arteriography reported:” after contrast injection in the left external carotid artery, marked impregnation of tumor aspect at the level of the inner ear-jugular foramen, with a known glomus jugulotympanic tumor. Afferences from this territory from the pharyngeal and posterior auricular, venous drainage towards the internal jugular, and a little reflux to the sigmoid sinus. There are no other arterial afferences from other territories”. An analytical study was a mild elevation of noradrenaline and dopamine (< x 2), normal metanephrines, negative extension study (including PET CT), and elevation of parathyroid hormone (PTH) with associated vitamin D deficiency.
Patient’s family history: her mother died of colon cancer. Father died of liver cirrhosis; No history of a pituitary tumor or alteration of phosphocalcic metabolism of intestinal tumor. A maternal aunt had kidney cancer; Another maternal aunt had pancreatic cancer; a Maternal first cousin had a brain tumor who died; another maternal cousin had kidney cancer (who was the daughter of a maternal aunt with pancreatic cancer). The patient has 2 of 3 daughters with positive genetic study SDHB, a brother who had a brain stroke without high blood pressure, and a sister with post ablative hypothyroidism due to hyperthyroidism.
The final diagnosis was a non-producing hypophyseal macroadenoma with an invasion of the sphenoidal sinus Knosp III with a left jugulotympanic paraganglioma (JTPG) Fisch C1 (clinical stage II, T2N0M0) [11], in context to family paraganglioma with positive genetic study for SDHB c.493delp. (Glu165LysfsTer10) (pathogenic heterozygosis).
After neurosurgical evaluation without surgical criteria for pituitary surgery, treatment of the PG radiotherapy options and surgery were proposed, and a surgical approach was decided based on age criteria (middle age) and tumor pathophysiology (catecholamine producer and variant with higher malignancy risk), and staging (Fish’s C1). Surgery planning was done in the anatomy department of Facultat de Medicina of Valencia’s University to establish the surgical steps and organize the expected times in each step to optimize a predictably long surgery performed by a single surgical team; tumor exeresis was performed using a type A infralabyrinthine (ITFA) and cervical combined approach with facial mobilization.
Results
An Anatomopathologic study showed a left jugulotympanic adenopathy with a reactive pattern with no evidence of malignancy and left JTPG (CD34+, synaptophysin+, prot S100+, ki67 proliferative index < 1%). Surgical sequelae were temporary left vocal paresis for the abduction that was compensated through speech therapy, facial paresis grade II, and moderate to low spinal paresis (XI pair) for the elevation of the arm that recovered to normality. Mixed hearing loss was predominantly transmissive, and dizziness and instability that was compensated in a few weeks. The patient is disease-free in image controls after 12 months of follow-up, without changes in the pituitary adenoma.
Discussion
Diagnosis and treatment of JTPG require a multidisciplinary approach due to its complexity, probability of multifocal involvement, and neuroendocrine and familial pathology [5,6,11–13]. Radiological findings on CT scans require complementary studies with MRI or angio MRI to better define the lesion and reach an accurate diagnosis [14], and extensión study with PET CT or another scintigraphy scan if there is a suspicion of malignancy [5]. In our case, we had problems in the diagnosis by CT in the port of our radiologist (despite being specialized and experienced and with a diagnosis of suspicion), doubts that were resolved by MRI study (see CASE REPORT). The therapeutic indication has been classically surgical, and it is considered the gold standard because only complete resection can be potentially curative [5,11] and due to the possibility of malignancy and local bone complications derived from radiotherapy [15]. Radiotherapy techniques using gamma knife, external beam RT, stereotactic radiosurgery, or hypofractionated stereotactic radiotherapy offer good results with the tumor growth control of more than 90% for ten years, although it increases growth to 25% between 10 years to 15 years of follow-up [16]. A meta-analysis performed by Jansen et al. describes a good control of the tumor and a lower rate of complications using radiotherapy in C and D JTPG compared to surgery, although the level of evidence is low [17]. In the case of inoperable or metastatic disease, systemic treatment with chemotherapy, radiometabolic therapy, and local ablative therapy are described [11]. The surgical indication must be appropriate to each patient, depending on age and the risk/benefit balance, due to postoperative sequelae, compared to radiotherapy or evolutionary follow-up [5,7,11,15,18,19]. Surgery requires planning and preparation of the patient using tumor embolization and control of possible complications in cases of catecholamine-producing tumors [9,11]. The approach must allow full tumor exposure for resection depending on its evolutionary stage. The Fisch type A infratemporal access allows approaching the posterior torn hole in C1 type cases, after mobilization of the facial nerve, control of the sigmoid sinus and the jugular vein, and removal of the base of the styloid process, as key points of surgery [1,3,8,13]. The technique of respecting the Fallopian aqueduct in PG type C/D is described with less facial nerve injury but decreases the rate of total resection and increases recurrences [20]. In our experience, we have obtained satisfactory results with the expected complications [15] (Figure 1,Figure 2).
To enhance patient security, we carried out a systematization according to our experience step by step to improve and sequence the surgical time, showing the items to be achieved at each surgical moment of the ITFA approach, establishing a timing that is exposed below:
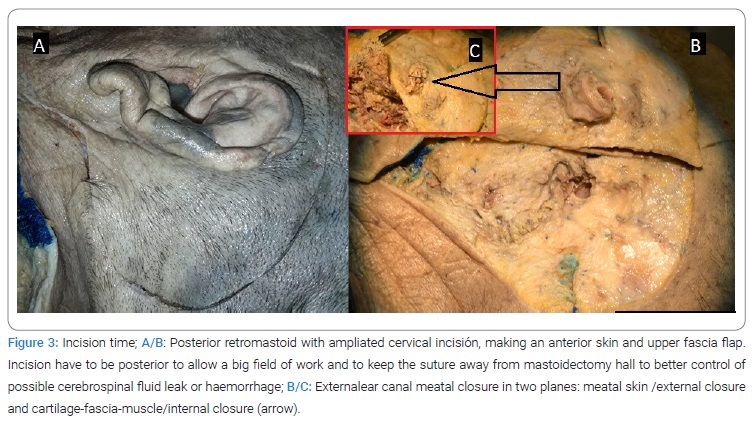
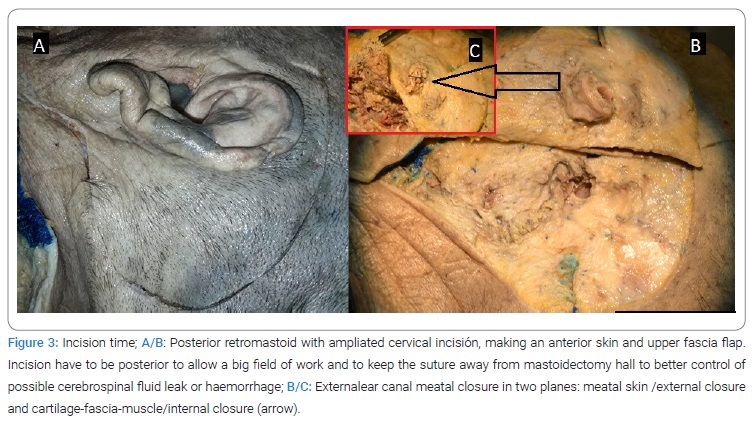
1. Incision time (Figure 3).
1a. The posterior retromastoid with ampliated cervical incisión makes an anterior skin and upper fascia flap (Figure 3A/B).
1b. External ear canal meatal closure in two planes: meatal skin /external closure and cartilage-fascia-muscle/internal closure, for middle ear occlusion (Figure 3B/C).
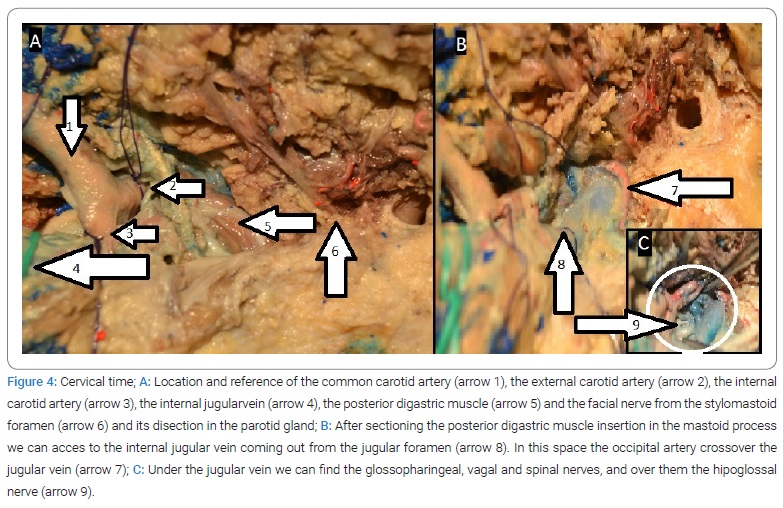
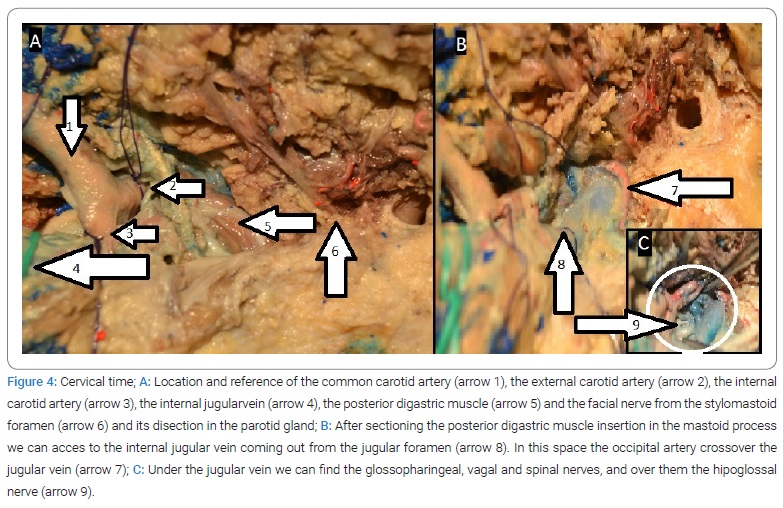
2. Cervical time (Figure 4).
2a. Location and reference of the jugular vein, common carotid artery, internal and external carotid artery, facial nerve from the stylomastoid foramen, and its dissection in the parotid gland (Figure 4A).
2b. Posterior digastric muscle section and sternocleidomastoid muscle at the mastoid insertion to access to internal jugularvein way out of the jugular foramen, occipital artery (Figure 4B), and low cranial nerves: spinal, vagal, pneumogastric and hypoglossal nerves (Figure 4C).
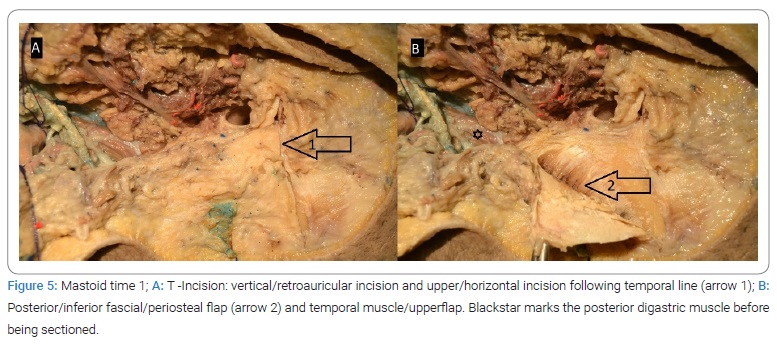
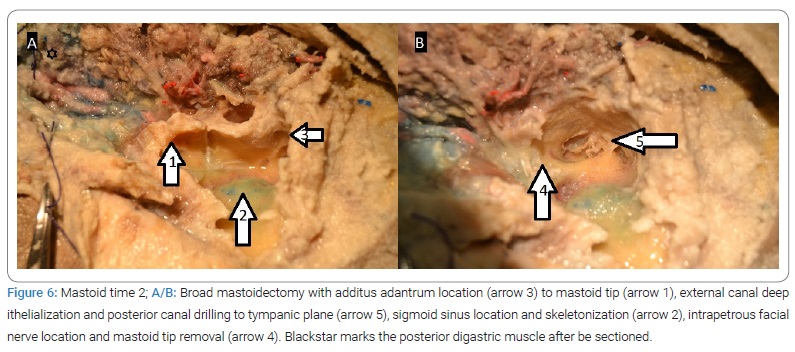
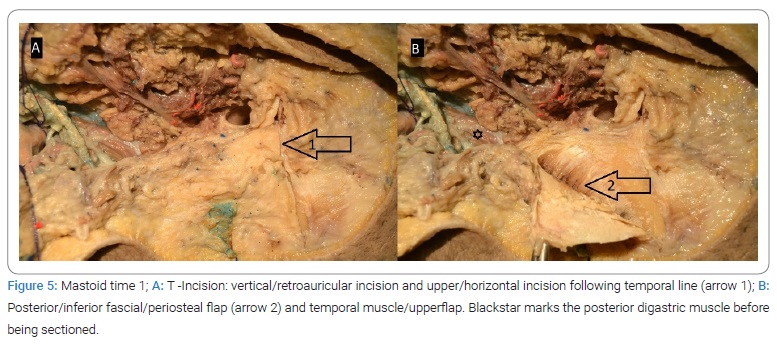
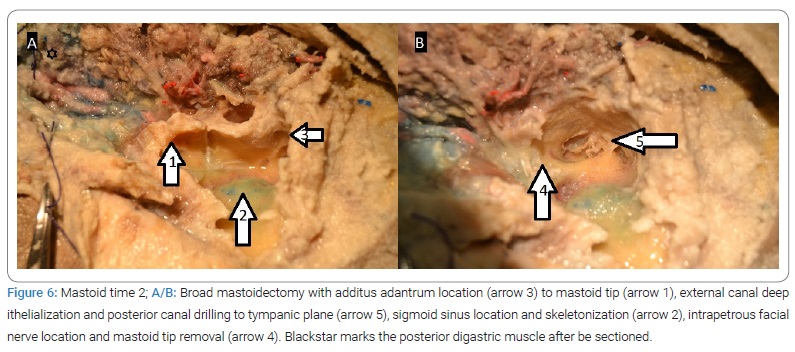
3. Mastoid time (Figure 5,Figure 6):
3a. T-incision (Figure 5): vertical/retroauricular incision to the mastoid tip and up/horizontal incision following the temporalis line (Figure 5A). We do a posterior/inferior fascial/periosteum flap (Figure 5B) and temporal muscle/upper flap to close at the end of surgery, keeping the mastoid/middle ear hole packed after filling it with abdominal fat.
3b. Broad canal down mastoidectomy (Figure 6A/B) with external canal de-epithelization, intrapetrous facial nerve location, sigmoid sinus location, and skeletonization and mastoid tip removal.
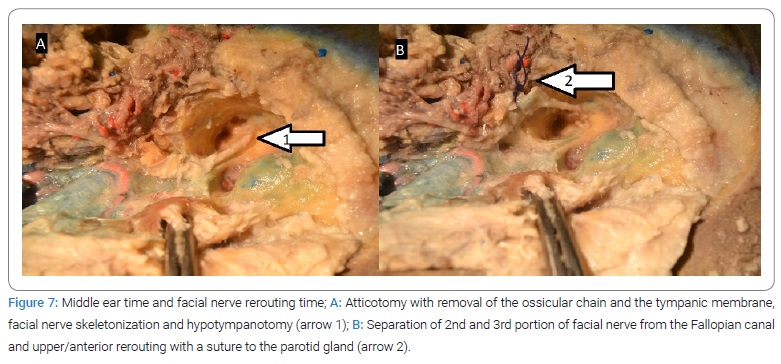
4. Middle ear time (Figure 7A):
4a. Atticotomy, ossicular chain, and tympanic membrane epithelium removal. At this time tympanic part of paraganglioma has to be removed using bipolar cauterization.
4b. Facial nerve skeletonization and hypo tympanotomy, looking for down part of the tumor.
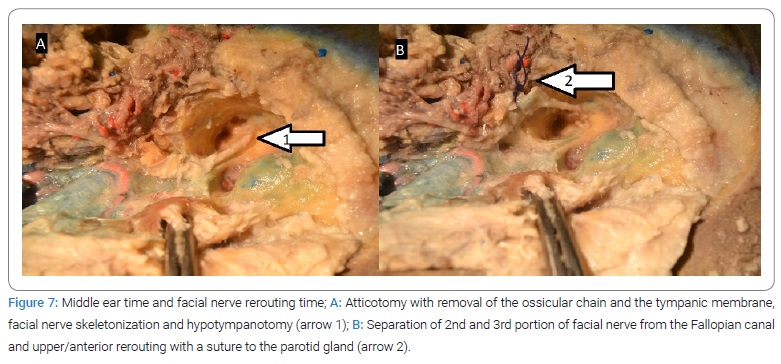
5. Facial nerve time (Figure 7B):
5a. Foramen stylomastoid cover excision with disinsertion of 2nd and 3rd portion of the facial nerve, upper/anterior re-routing, and suture to the parotid gland.
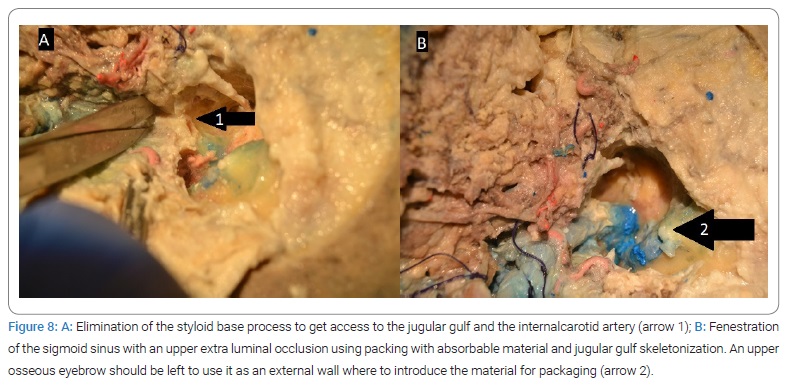
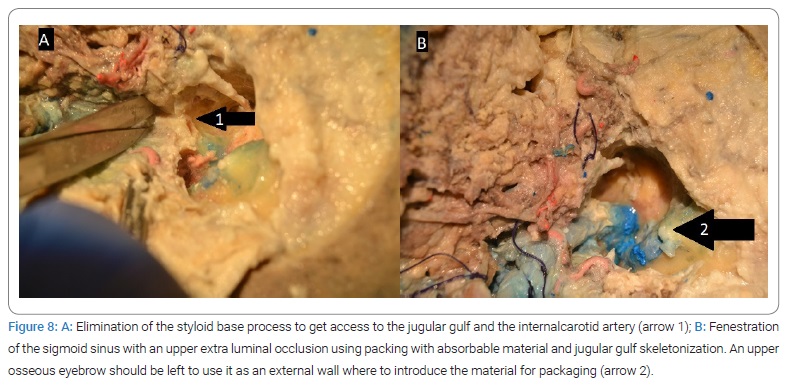
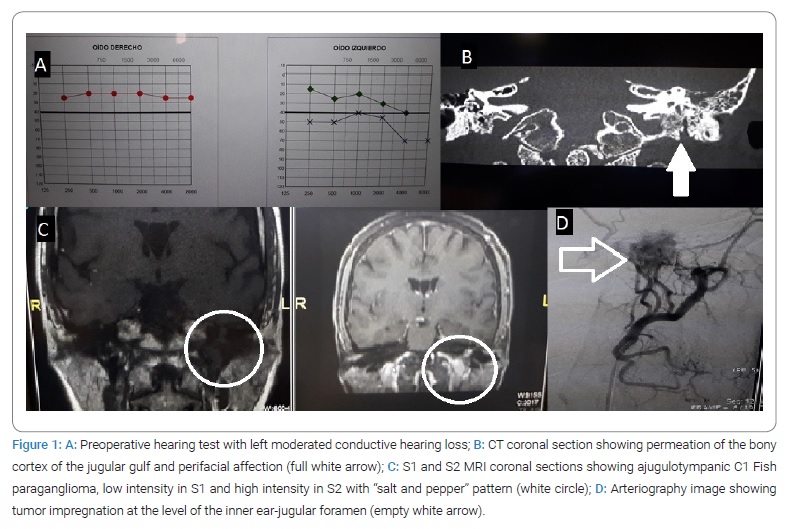
6. Sigmoid sinus time (Figure 8):
6a. Eliminating the styloid base process to access the jugular gulf and internal carotid artery (Figure 8A).
6b. Fenestration of the sigmoid sinus with extraluminal occlusion using absorbable packing material, jugular gulf skeletonization (Figure 8B).
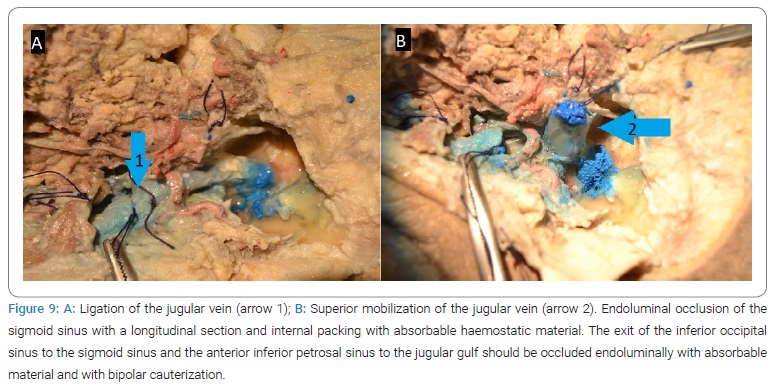
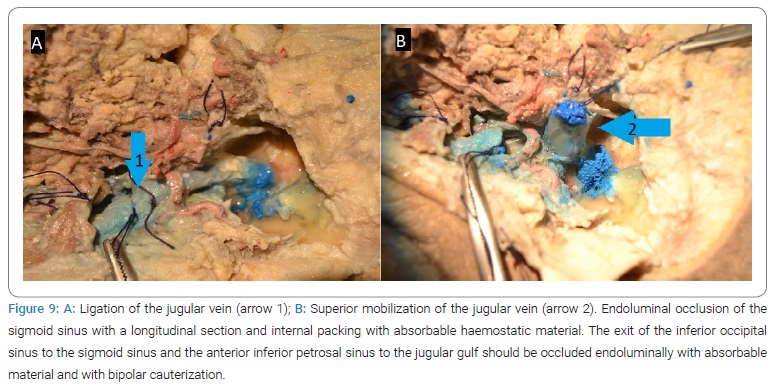
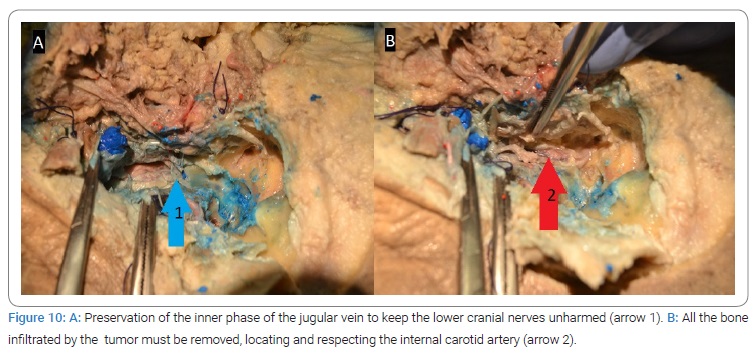
7. Jugular foramen time (Figure 9,Figure 10):
7a. Jugularvein ligation with superior mobilization (Figure 9A/B). Endoluminal occlusion of the sigmoid sinus with a longitudinal section and internal packing with resorbable hemostatic material. The exit of the inferior occipital sinus to the sigmoid sinus and the anterior inferior petrous sinus to the jugulargulf should be occluded endoluminally with absorbable material and bipolar cauterization.
7b. Preservation of the inner phase of the jugularvein to keep the lower cranial nerves unharmed (Figure 10A). All bone infiltrated by the tumor must be removed, locating and respecting the internal carotid artery (Figure 10B).
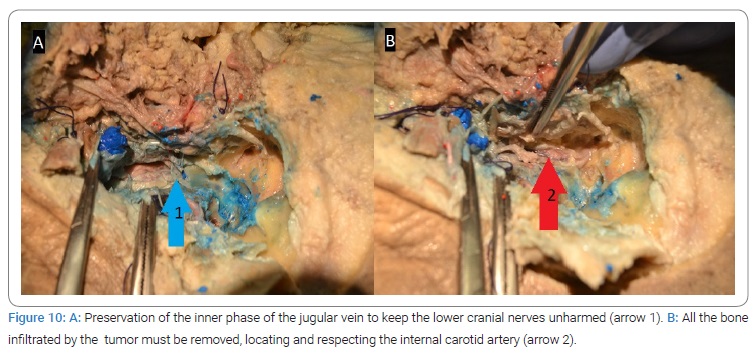
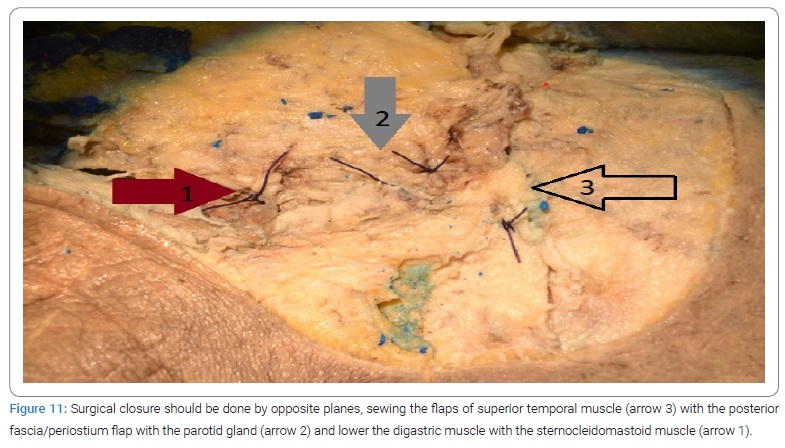
8. Surgical closure time:
8a. After tumor removal eustachian tube must be occluded with periosteum and muscle, and the mastoid hole should be filled with abdominal fat. Finally, opposite planes should do surgical closure (Figure 11).
Conclusion
Clinical diagnosis of Jugulotympanic Paraganglioma (JTPG) requires a multidisciplinary study and a therapeutic indication adjusted to each patient. The Infra Labyrinthine (ITFA) approach requires adequate training to minimize surgical damage to the facial nerve (careful rerouting) and low cranial nerves (keeping the posterior wall of the jugularvein at its exit through the jugular foramen). Control the lateral venous sinus and its afferences (occipital sinus and superior and inferior petrosal sinus), locate and respect the internal carotid artery, and the complete excision of the tumor. The limitations of the technique are the tumor size, location, and the grade of involvement of the internal carotid artery by the tumor, which require endovascular techniques of stenting. Moreover, other kinds of approaches for total removal (amplified IFTA or IFTB in C3 and C4 Fish´s modified classification with one or two surgery times if there is or no endocranial or intradural affection), or combination with radiotherapy and other treatments in partial resections or inoperable tumors. In our experience, the planning and preparation of the surgery on a human specimen were fundamental for its realization. Therefore, we recommend this way of proceeding to improve the quality of care and surgical outcomes.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Cite this article
Rubio Segarra V, Díaz Fernández A, Pont Colomer E, Delvasto Ureña AL, Pérez Moltó FJ. A clinical case of jugulotympanic paraganglioma C1: how surgery was managed. Clin Case Rep J. 2022;3(6):1–8.