Traumatic Iris Cyst Treated with YAG Laser: A Case Report
* Romero Estrada Jose;
Varela Gonzalez Roberto;
-
* Romero Estrada Jose: Department of Ocular Trauma, Ophthalmology, Unidad Nacional de Oftalmología, Guatemala.
-
Varela Gonzalez Roberto: Department of Ocular Trauma, Ophthalmology, Unidad Nacional de Oftalmología, Guatemala.
Abstract
We report a clinical case of an 8-year-old with a history of penetrating trauma in the right eye. Surgical innervation was performed due to a corneo-limbo-scleral wound. After one year, he presented to our department with decreased vision and discomfort in the right eye. Upon examination, a traumatic iris cyst is observed. The cyst was treated with Nd-YAG laser, obtaining a size reduction and visual acuity improvement.
Introduction
Cysts are epithelial-lined spaces with an idiopathic etiology and can present in a diversity of ways, such as a posterior epithelial cyst or free-floating cyst [1]. These are divided into primary and secondary cysts. Secondary cyst result of epithelial implantation by metastasis, uveitis, more commonly post-traumatic or postsurgical [2]. The most common secondary cysts are peripheral iris pigment epithelial cysts, up to 55% [3].
The clinical spectrum in which this post-traumatic cyst presents is diverse. Although the diagnosis is clinical, ultrasound biomicroscopy (UBM) has made it possible to study some of the features of these cysts [4]. For example, cysts may be observed when they remain small, stable, and asymptomatic [5].
Various surgical procedures for iris cysts have been reported, and the result depends on the size of the cyst, affected area of the anterior chamber, and prompt treatment [3]. Laser photocoagulation has been recommended as an alternative, less invasive treatment with fewer complications [6].
Case Presentation
An 8-year-old male with a history of penetrating trauma in the right eye, which caused a cornea-limbo-scleral wound, the patient went under surgery for reparation. The trauma was localized to the anterior segment, and lens and fundus examinations were normal. After several visitations patient had a positive evolution, so he was discharged from the trauma department to the pediatric department for annual follow-up.
The patient presents one year after the event to the clinic complaining of itching, burning sensation, discharge, and blur vision after one month of evolution. Visual acuity was 20/50 in the right eye and 20/20 in the left eye. A slit lamp examination of the right eye showed hyperemic conjunctiva and cornea clear, except for a leukoma in the site of the corneal wound reparation. In the anterior chamber, an iris cyst is seen just beneath the leukoma; this iris cyst was not documented after the trauma or follow-up. The rest of the examination did not show any other pathology.
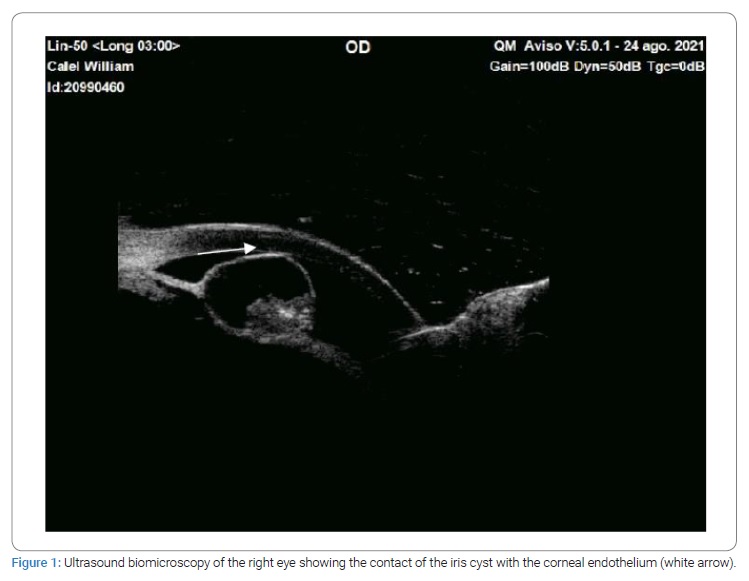
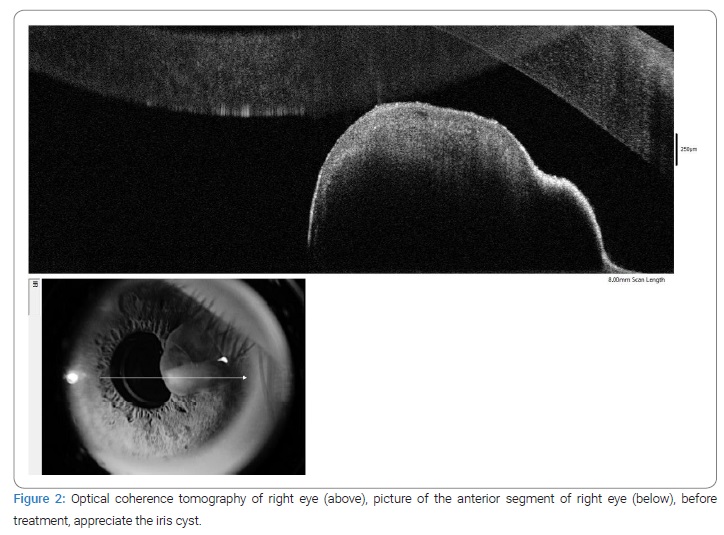
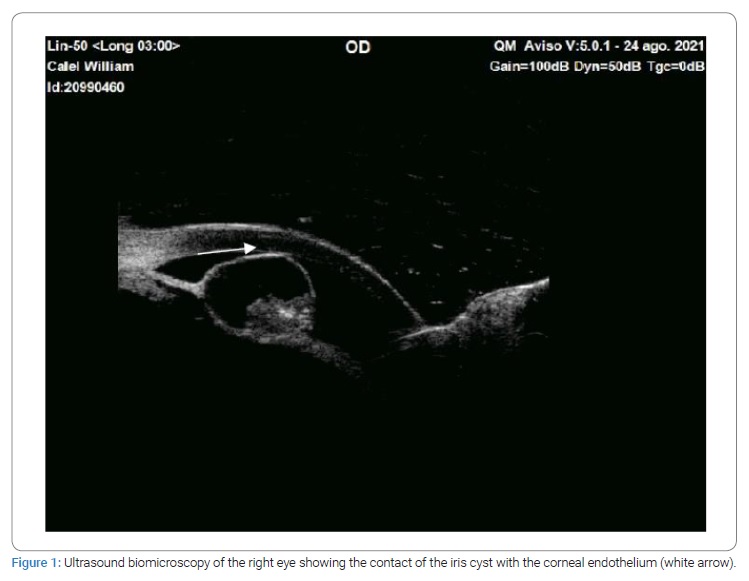
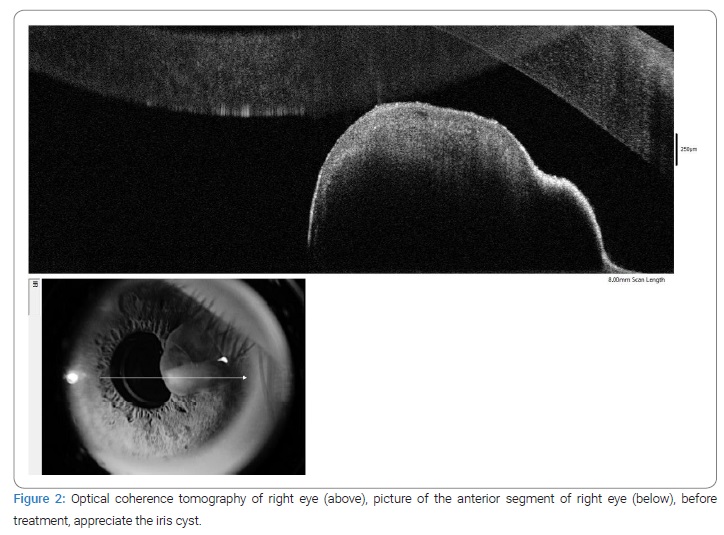
AUBM was performed on the patient (Figure 1), documenting a cystic mass from the iris that did not compromise the angle. In addition, an OCT of the anterior segment was requested, there it was found that the cyst was close to the corneal endothelium (Figure 2).
The patient was taken to YAG laser, three shoots with a power of 3.2 mJ, and a decrease in size was seen. Mild inflammation was observed after treatment, treated with tobramycin/dexamethasone every six hours for seven days.
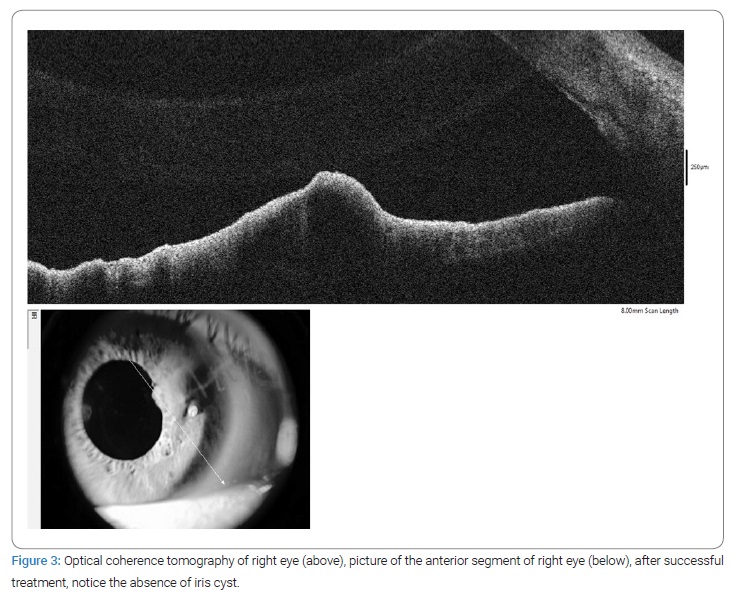
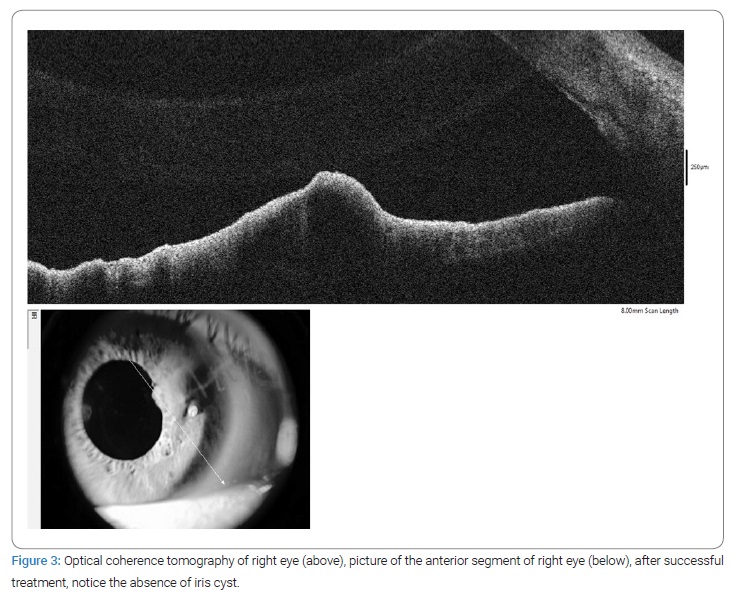
A week after the YAG laser and medical treatment, visual acuity and symptoms improved in the right eye to 20/30. In addition, a significant reduction was observed in the biomicroscopy; for documentation, an OCT was performed where we substantiate the absence of the cyst (Figure 3).
The IOP was evaluated with a non-contact tonometer and always remained within normal values before and after laser treatment.
Discussion
We decided to treat our patient with a non-invasive, almost painless procedure, to prevent a surgical procedure with general anesthesia and the inherent risks. Despite his age, the patient was cooperative, and the procedure went without complications.
Several treatments are available, most of them invasive; here, we present a case in which an alternative treatment was performed. This case represents a secondary iris cyst; the antecedent and the area of the trauma are suggestive. Also, trauma is the leading cause of secondary iris cyst [4].
The epithelium proliferation after trauma takes the form of three distinct varieties: serous, pearl cyst, or epithelial down growth [2,7]. The epithelium enters the anterior chamber via de wounds, and the environment provided by the iris induces cell proliferation [2].
Conclusions
Different approaches have been described for the treatment of iris cysts. Nd: YAG laser is a less-invasive approach to collapse the cyst. It is, in our opinion, more cost-effective than surgery and has fewer side effects than general anesthesia.
In our case, even though the patient was a minor, he was cooperative, and we were able to complete 3 Nd: YAG laser shots to the cyst with an immediate reduction in size.
Other pathologies should be considered, such as iris adenoma, iris nevus, and iris melanoma. The history, clinical characteristics, and complementary studies are of great importance to get a precise diagnosis.
We encourage making treatment decisions integrally, always considering patient comorbidities.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Siddharthan KS, Shah S, Reddy JK. Diagnosis and management of post - traumatic pearl iris cyst. TNOA J Ophthalmic Sci Res. 2021;59(2):193.
- Li HY, Li MJ, Xu ZY, Li JH, Zheng WL, Wu Y, et al. A secondary iris cyst with 3 years of asymptomatic period following a blunt ocular trauma. Eur J Ophthalmol. 2021;31(3):NP1–NP4.
- Gondhowiarjo TD, Artini W. Delayed treatment of secondary iris cyst due to blunt ocular trauma. J Case Reports. 2018;8(1):14–17.
- Gupta V, Rao A, Sinha A, Kumar N, Sihota R. Post-traumatic inclusion cysts of the iris: A longterm prospective case series. Acta Ophthalmol Scand. 2007;85(8):893–896.
- Haller JA, Stark WJ, Azab A, Thomsen RW, Gottsch JD. Surgical management of anterior chamber epithelial cysts. Am J Ophthalmol. 2003;135(3):309–313.
- Tsai JC, Arrindell EL, O’Day DM. Needle aspiration and endodiathermy treatment of epithelial inclusion cyst of the iris. Am J Ophthalmol. 2001;131(2):263–265.
- Venkateswaran N, Ching SST, Fischer W, Lee F, Yeaney G, Hindman HB. The diagnostic and therapeutic challenges of posttraumatic iris implantation cysts: illustrative case presentations and a review of the literature. Case Rep Ophthalmol Med. 2015;2015:375947.
Keywords
Ocular trauma; Iris cyst; YAG laser
Cite this article
Jose RE, Roberto VG. Traumatic iris cyst treated with YAG laser: a case report. Clin Case Rep J. 2022;3(6):1–4.
Copyright
© 2022 Romero Estrada Jose. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).