Abstract
Most children affected with COVID-19 have mild symptoms; however, a small number of these children may develop Multisystem Inflammatory Syndrome (MIS-C). In most cases, this condition results in fast deterioration of the patient’s heath involving multiple organ systems, raised inflammatory markers, and gastrointestinal symptoms. Our 10-year-old male patient presented at first with an illness suggestive of viral gastroenteritis. He had a history of COVID-19 exposure but did not meet the criteria for diagnosis of MIS-C. However, he was admitted to the hospital a month later due to hypovolemic shock, meeting MIS-C criteria. Therefore, our case aims to highlight the importance of maintaining a high degree of suspicion for MIS-C and close monitoring for deterioration of patients with a history of COVID-19 infection and gastrointestinal symptoms, knowing that early detection is key to treatment in most developing countries.
Introduction
Most children affected with COVID-19 are asymptomatic or have mild symptoms. Therefore, only about 5%–10% of these children are hospitalized due to the severity of their symptoms [1]. This case report addresses one of these causes, temporally related to COVID-19 infection, Multisystem Inflammatory Syndrome in Children (MIS-C).
WHO defines MIS-C as [2].
- For ages 0 year–19 years with fever > 3 days and two of the following:
- Rash or conjunctivitis or mucocutaneous inflammation signs.
- Hypotension or shock.
- Features of myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities.
- Evidence of coagulopathy (by PT, PTT, and elevated D-dimers).
- Acute gastrointestinal problems.
Elevated inflammatory markers.
No other obvious microbial cause of inflammation.
Evidence of COVID-19 or likely contact with patients with COVID-19.
Case Presentation
Our 10-year-old male patient presented with fever, large volume diarrhea, and colicky abdominal pain in the last seven days. His blood cell counts and inflammatory markers were in the normal range. Stool studies did not indicate any abnormalities. He tested negative for a nasopharyngeal swab test for COVID-19. However, he had been treated for COVID-19 infection a month back as a contact of positively tested parents. His inflammatory markers had been raised at that time.
Along with abdominal symptoms, he was also diagnosed with having mild right-sided pleural effusion on ultrasound. Hence suspicion of tuberculosis was considered but ruled out after a negative MTB TrueNAT Rif test.
On ileocolonoscopy, mild nodularity was seen in the colon, suggestive of Crohn’s disease, but with the absence of granulomas on biopsy and negative ASCA antibodies and ANCA biomarkers, diagnosis of Inflammatory bowel disease was ruled out. The patient’s ileal biopsy showed crypt atrophy, inflammatory destruction of crypt glands, and mixed inflammatory cell infiltrate in lamina propria, suggestive of celiac disease, but the possibility was made unlikely by a negative tissue transglutaminase IgA test.
Thus, the patient was treated as a case of possible infectious gastroenteritis with IV fluids, antibiotics, antiemetics, and antacids for two days and discharged in stable condition.
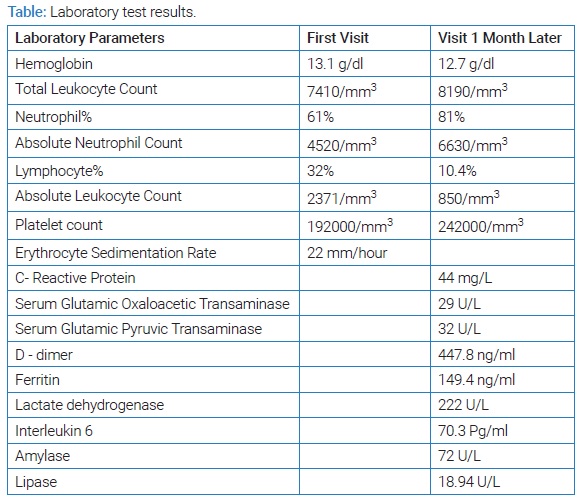
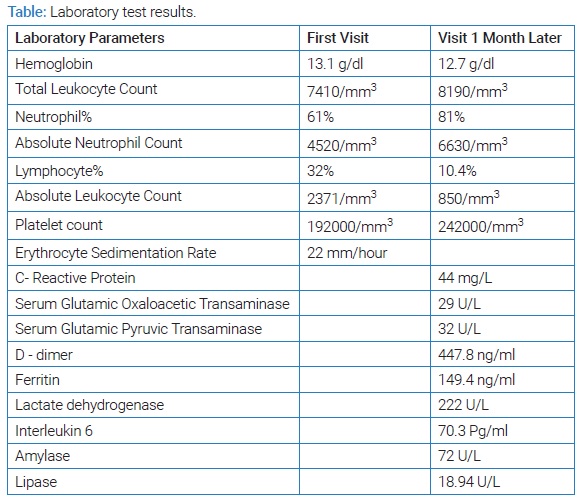
One month later, he presented to the hospital in hypovolemic shock and required ventilatory support (Table). At this time, there was a rise in inflammatory markers (CRP: 44, IL-6: 70.3 pg/ml, D-Dimer: 447.8 ng/ml), lymphopenia, thrombocytopenia, and persistence of previous symptoms.
With the presence of multisystem involvement and raised inflammatory markers, attention was shifted to the possibility of MIS-C. This was unusual as MIS-C is noted to occur 4 weeks–6 weeks after a COVID-19 infection, unlike in our patient who presented two months after a history of contact [1]. He tested positive for the COVID-19 antibody, making the diagnosis likely [1].
Treatment: The patient was treated with plenty of IV fluids, IVIG, and IV methylprednisolone [3]. He responded well to the IVIG and steroid treatment and was afebrile within 48 hours. His inflammatory markers decreased gradually, and ten days later, he was discharged. He was advised of regular outpatient follow-up for the next two weeks. His inflammatory marker levels receded to baseline, and his Echocardiogram results showed normal heart function.
Discussion
MIS-C diagnoses post COVID-19 infection emerged in the summer of 2020, with several case reports of children exhibiting a condition suggestive of Kawasaki’s disease or toxic shock syndrome. It was suggested that an immune response produced in children post COVID-19 infection ultimately led to systemic involvement and not a direct cellular injury by the virus itself. This is supported by the effectiveness of immunosuppressants in treating the condition [4].
Although a patient of MIS-C may exhibit a range of symptoms, gastrointestinal symptoms are more commonly observed than others. Gastrointestinal manifestations are now known to be present in almost 50% of patients of MIS-C [5], most of which consist of abdominal pain, vomiting, and diarrhea, similar to our patient. This is because SARS-Cov-2 can infect enterocytes by binding the angiotensin-converting enzyme two receptors, causing gastrointestinal symptoms [5]. Toubiana et al., in their study of 21 patients of Kawasaki, like multisystem inflammatory syndrome post-COVID-19 infection, reported that all of their patients had early gastrointestinal symptoms like diarrhea, nausea, and vomiting [6].
This patient’s second admission and subsequent complication could have been avoided by keeping a high index of suspicion for MIS-C in a case of persistent diarrhea with a history of COVID-19 infection/ close contact, especially in view of a history of raised inflammatory markers [1]. These cases are rare but severe, which should require cases of prior COVID-19 infection and gastrointestinal symptoms to be monitored for deterioration after supportive treatment of gastrointestinal symptoms. Once MIS-C presentation sets in, patients’ symptoms often worsen quickly, and they require intubation and ventilatory support, equipment that is not easily available outside of large cities in developing countries. Therefore, a high index of suspicion for MIS-C is the need of the hour, especially in the presence of rising COVID-19 cases. This will facilitate early detection in low-level and mid-level income countries and lead to a favorable prognosis.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Inflammatory syndrome; Gastrointestinal manifestations; COVID-19
Cite this article
Bhavsar J, Chakra N, Tetarbe S, Shah I. Diagnosis of multisystem inflammatory syndrome in children with gastrointestinal manifestations. Clin Case Rep J. 2022;3(7):1–3.
Copyright
© 2022 Bhavsar J. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).