Abstract
Oral health is a source of psychological and physical comfort. A 59-year-old male patient presented five weeks after receiving the first dose of the Pfizer COVID-19 vaccine. He experienced physical and psychological distress, anxiety, fear, and pain from perioral swelling, cracked lips, numbness, and xerostomia. These signs and symptoms negatively affected his smile and overall facial expression. His condition worsened over time and included dryness around the mouth and chapped lips. Within four weeks of the first dose, he developed swollen lips and numbness in the skin around the lips and the gingiva-supporting teeth. Xerostomia, swelling and “heavy” lips, and gingival paresthesia worsened and then stabilized at five weeks post-vaccination; methylprednisolone, an anti-swelling medication, was prescribed in conjunction with ibuprofen, an anti-inflammatory medication. His physician suggested an allergic reaction to the Pfizer vaccine. At eight weeks, the patient’s condition appears stabilized, but the lip area is still swollen, numb, and slightly red. Supportive care alone in managing COVID-19 symptoms is insufficient in patients experiencing tongue and lip swelling, gingival paresthesia, and salivary malfunction. However, these inexpensive treatments may be effective, thereby reducing the risk of complications.
Introduction
COVID-19 vaccines can exert side effects, including long-term damage [1]. Temporary side effects should be recognized and managed effectively [2,3]. The oral effects of COVID-19 infection may be direct or indirect, resulting in dysgeusia (an altered or impaired sense of taste).
Xerostomia has been reported to be common among COVID-19 patients [4] and is a sign of dehydration, a contributing factor in COVID-19 infection. In addition, angiotensin-converting enzyme two has been reported to be the main site of entry of SARS-CoV-2 into the cell, supporting a hypothesis of viral-induced infection and inflammation as a cause of xerostomia. Therefore, xerostomia should be considered a possible clinical manifestation of COVID-19 [5].
Our patient developed soft-tissue lesions affecting the tongue, lips, palate, and oropharynx, as well as salivary gland involvement and xerostomia. It is unclear whether these lesions were an oral manifestation of systemic involvement or resulted from a direct viral connection to the adrenocorticotropic hormone receptor in the oral cavity. His soft-tissue lesions mimicked recurrent Herpes simplex, candidiasis, or geographic tongue. Oral mucosal lesions have been observed in COVID-19 patients [6,7], but whether these phenomena are symptoms of the disease or secondary effects is unknown.
The blisters on the patient’s lips and the lesions in keratinized tissue were consistent with those of Herpes simplex infection, although the patient denied a history of herpetic infection. In addition, he had lesions compatible with erythema multiforme, suggesting a link between COVID-19 infection or vaccine and oral ulceration and blistering. However, these signs may go undetected if an intraoral examination is not conducted during hospital admission. Although the relationship between the vaccine and erythema multiforme-like lesions has not been confirmed, the vaccine could potentially trigger a silent herpes virus infection to manifest as a form of erythema multiforme [8].
Since the Food and Drug Administration’s emergency use authorization of the Pfizer-BioNTech COVID-19 vaccine, many side effects have been reported in the medical literature, including oral symptoms such as swelling and xerostomia. The present case report aims to inform the scientific community about this potential side effect of the vaccine.
The etiology of the hypersensitivity reaction is unknown. Contributing factors include hygiene products such as toothpaste and over-the-counter mouth rinses. However, these products have been in widespread use for decades with no allergic reactions, and the literature does not support hygiene products as the cause of paresthesia or xerostomia. Our patient reported using Colgate toothpaste and Listerine mouthwash for more than a year prior to the first dose of the Pfizer vaccine. The chronic nature of his condition suggests that the hypersensitivity is a delayed reaction to the vaccine.
The patient reported no significant medical history besides daily atorvastatin (20 mg) for hypercholesteremia. To manage the swelling and inflammation even in the absence of a known etiology, we prescribed a Medrol dose pack (methylprednisone)in combination with the analgesic ibuprofen [9], as supportive care alone is insufficient [10].
This case report suggests dentist involvement in the diagnosis and treatment planning of gingival side effects of the Pfizer vaccine [6]. Oral lesions affecting the gingiva are often undetected, as intraoral examinations are not typical during hospital admissions [7].
Case Presentation
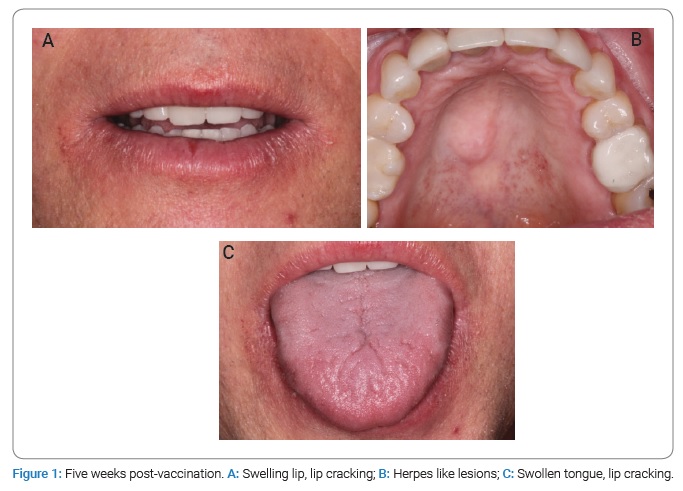
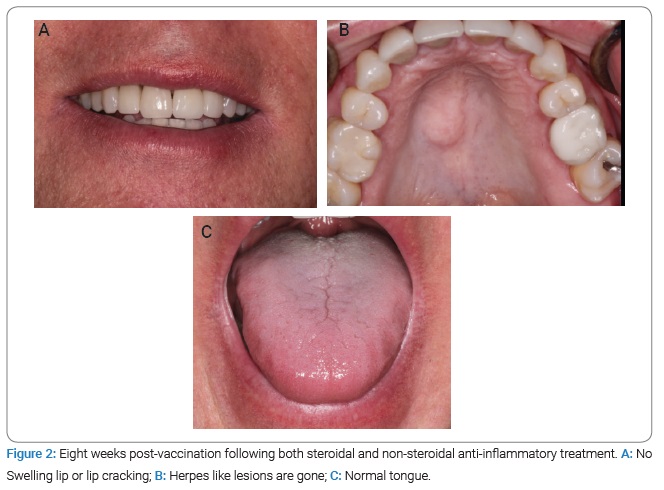
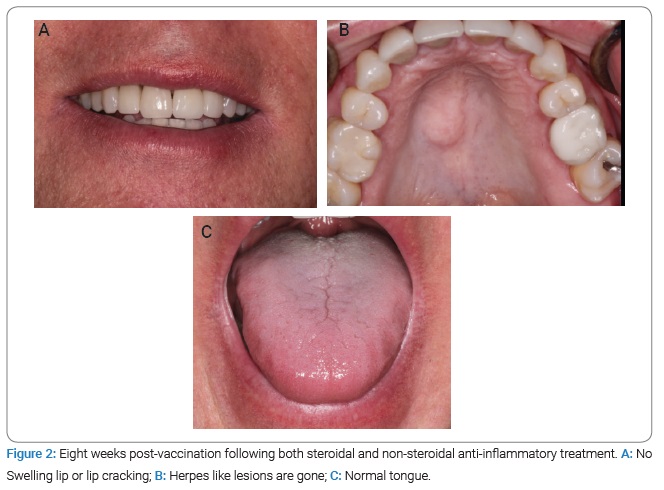
A 59-year-old American male patient presented with apparently vaccine-induced oral and perioral swelling, paresthesia, and xerostomia. The patient stated that he developed a reaction to the first dose of the Pfizer COVID-19 vaccine approximately 14 days after the injection. The patient presented with swollen lips and tongue, cracked lips, numbness of the gingiva supporting anterior teeth, and xerostomia (Figure 1). The patient did not specifically complain of dysgeusia but did develop a series of soft-tissue lesions in the palate (both hard and soft), lips, and oropharynx. The lesions could have resulted from a secondary infection related to the patient’s compromised immune system rather than directly from the coronavirus itself (Figure 2).
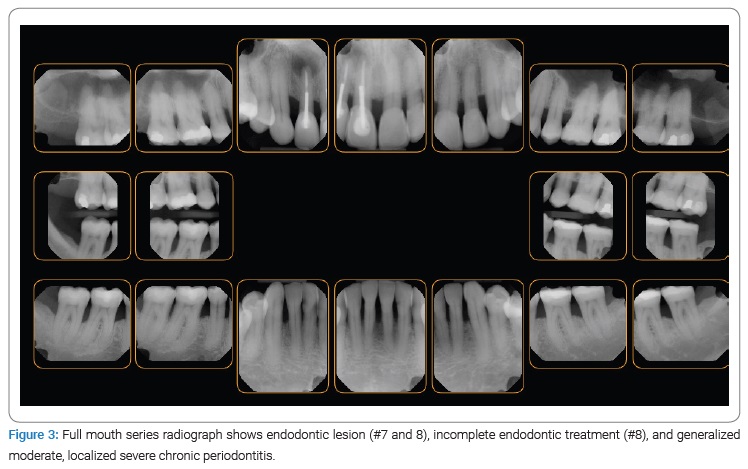
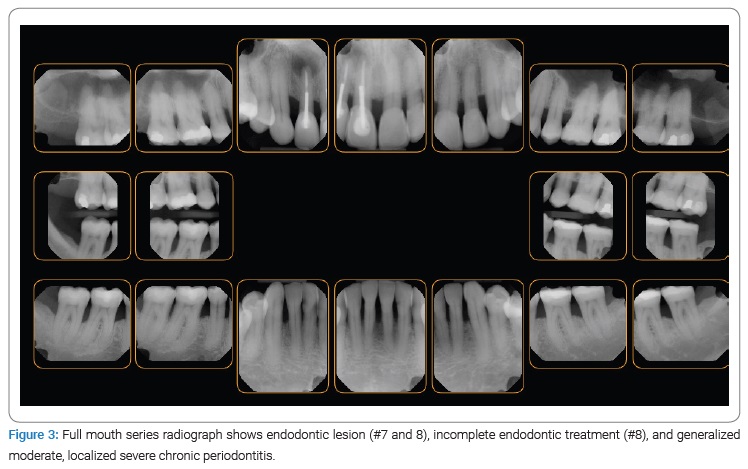
Clinical and radiographic evaluation disclosed missing teeth (#1, 5, 12, 16, 17, 21, 28, and 32), a history of orthodontic treatment, generalized moderate but localized severe gingival recession/abfraction, missing interdental papilla (#6–14 and 21–27), endodontic concerns (#7 and 8), vertical and horizontal bone loss, and occlusal disharmony (Figure 3).
Chief Complaint: “Lip cracking, tongue and lip swelling, numbness (back left and right of tongue, gingival, outside of lips), and dry mouth.”
Diagnosis: Vaccine-induced oral and perioral swelling, paresthesia, and xerostomia, periapical periodontitis (#7 and 8), incomplete endodontic treatment (#8), generalized moderate, localized severe chronic periodontitis, gingival deformity, abfraction, migration of teeth, and occlusal trauma.
Medical Considerations: None.
Allergies: Hay fever, T: 97.9°F, BP: 129/83 mmHg, pulse: 62/min.
Etiology: Vaccine, plaque, calculus, occlusal trauma, and ineffective oral hygiene.
Therapy: Follow-up on vaccine-induced swelling, cone-beam computed tomography, biopsy, gingival grafting for teeth with gingival recession, night guard, and endodontic consultation.
Status: Cone-beam computed tomography did not disclose any abnormality other than the endodontic lesion for teeth #7 and 8.
Conclusion
This is a rare case report of an oral manifestation of systemic disease. This report aims to highlight a possible link between the first dose of the Pfizer vaccine and oral and perioral swelling, cracked lips, numbness, and xerostomia. Awareness of orofacial manifestations of vaccine-induced unintended outcomes will improve recognition and management of these adverse effects.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Paresthesia; COVID-19; Xerostomia
Cite this article
Soolari A. Vaccine-induced oral and perioral swelling, paresthesia, and xerostomia. Clin Case Rep J. 2022;3(8):1–4.
Copyright
© 2022 Ahmad Soolari. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).