Abstract
Solitary Fibrous Tumors (SFT) are rare fibroblastic mesenchymal neoplasms that most often arise from the visceral pleura, abdomen/pelvis, extremities, and neck. However, SFTs have been reported at any anatomical site. Solitary fibrous tumors occurred in patients over a wide age range with a median age of 60 years. Most SFTs have an indolent course, but 11% to 22% of the SFTs show a more aggressive behavior with distant metastasis and malignant transformation.
Here, we report a rare clinical presentation of a benign SFT in the right breast in a relatively young woman. We described the clinical, radiographic, histopathological, and immunohistochemical findings. Furthermore, we provide a brief literature review on differential diagnosis, prognostic factors, and treatment of SFTs.
Introduction
A Solitary Fibrous Tumor (SFT) is a rare fibroblastic mesenchymal neoplasm. SFTs are characterized by haphazardly arranged spindled cells. The differential diagnosis of spindle cell lesions includes inflammatory myofibroblastic tumor, nodular fasciitis, fibromatosis, reactive spindle cell nodule, leiomyoma, spindle cell metaplastic carcinoma, and myoepithelioma. Although SFTs occur most commonly in the visceral pleura, several anatomical sites of involvement have been reported.
This report described the clinical, radiographic, histopathological, and immunohistochemical findings of a 42-year-old woman with a mammary SFT. Only 30 cases of mammary SFTs have been described so far. Furthermore, we provide a brief literature review on differential diagnosis, prognostic factors, and treatment of SFTs.
Case Presentation
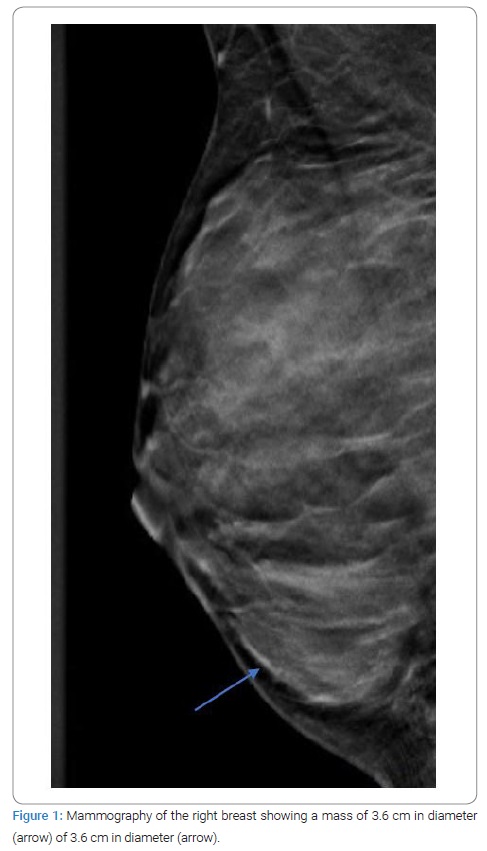
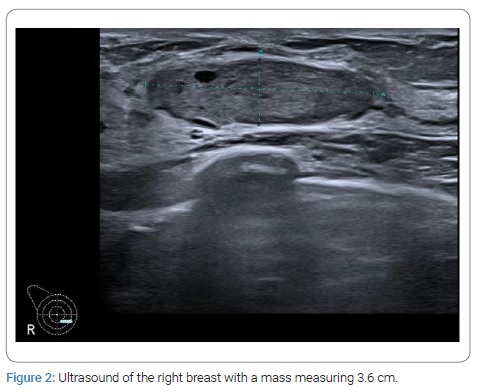
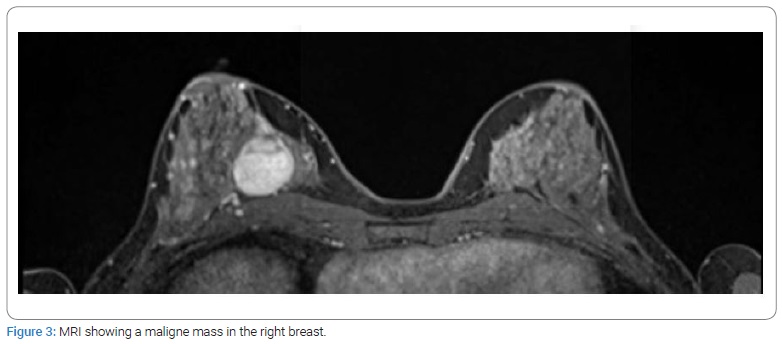
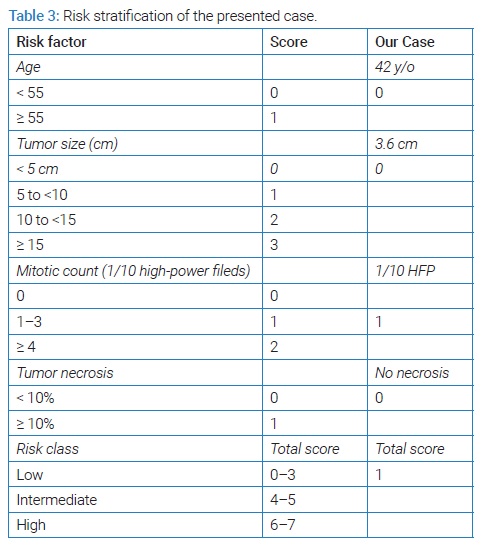
A 42-year-old woman with no medical history attended the outpatient clinic in February 2021. She recently discovered a palpable nodule in her left breast. A painless, firm, and mobile mass originating from above the nipple-areolar complex in the left breast measuring 1.5 cm in diameter was noted on physical examination and was highly suspect for a fibroadenoma. There were no palpable abnormalities in the right breast. Besides the palpable mass of the left breast, ultrasound examination and mammography also showed a mass measuring 3.6 cm in the medial inner quadrant of the right breast (Figure 1,Figure 2) (assessed as BI-RADS 3). The magnetic resonance imaging findings found a malignant mass with fast contrast enhancement. The mass was assessed as BI-RADS 5 (Figure 3).
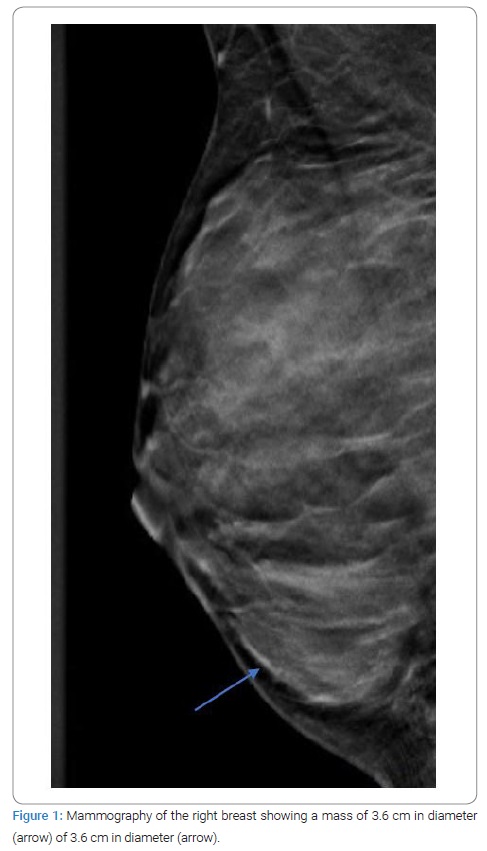
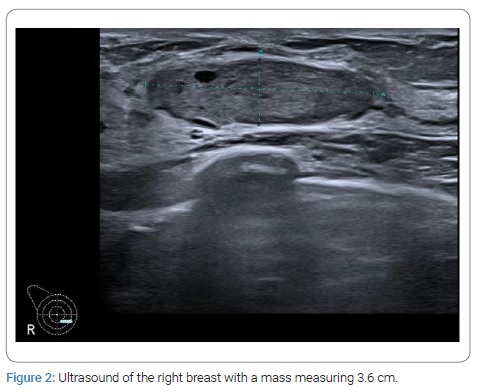
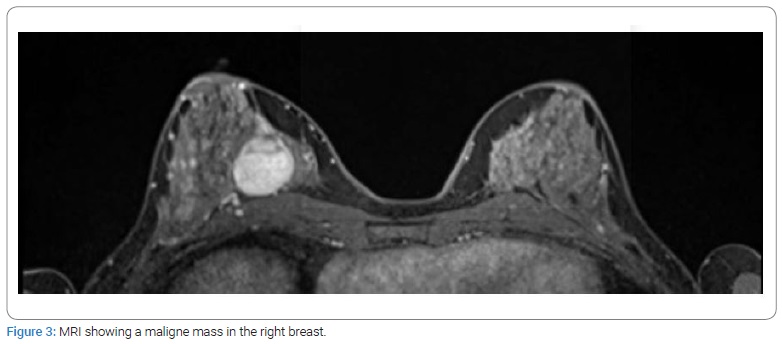
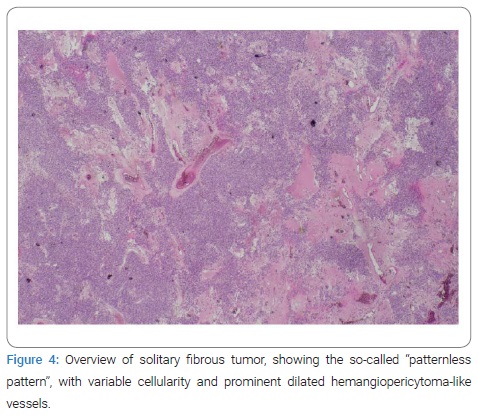
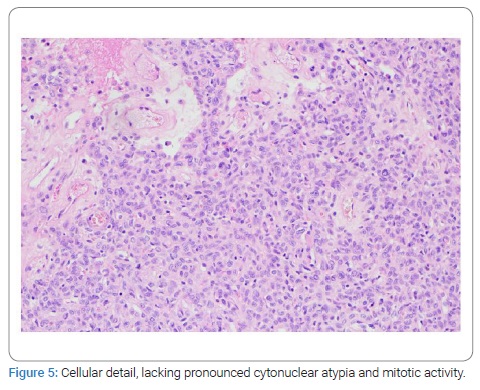
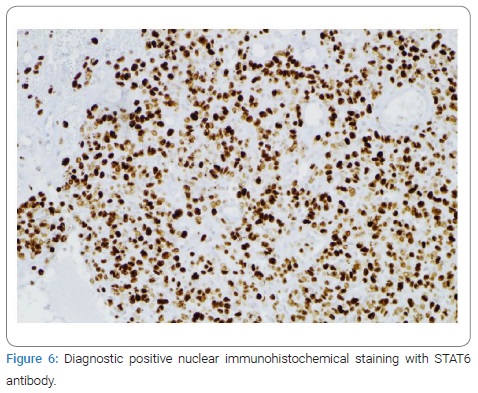
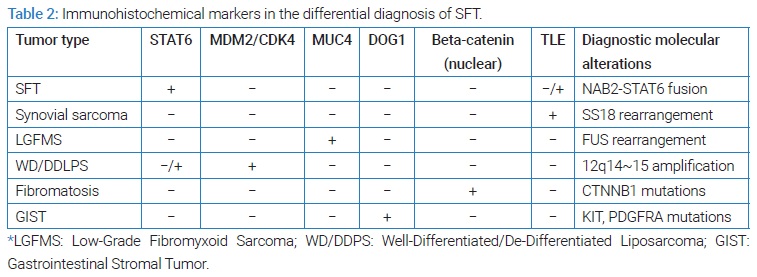
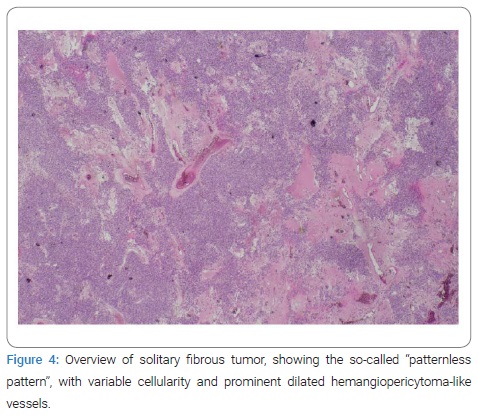
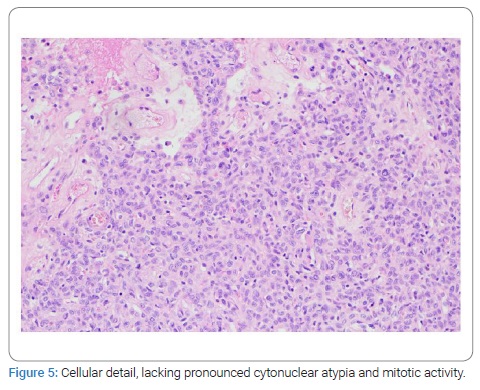
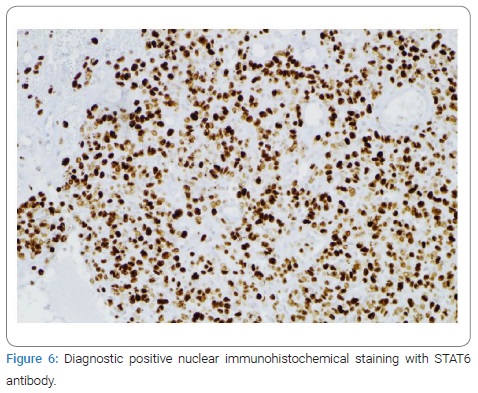
Image-guided core needle biopsy of both masses was performed. The histologic diagnosis of the mass in the left breast favored a fibroadenoma. The histologic findings of the mass in the right breast showed hypercellular tissue built out of lumpish cells without any recognizable structure (Figure 4). The cells showed no atypical nuclei or mitotic activity (Figure 5). The immunophenotype was as follows: few weak enhancing nuclei in the endoplasmic reticulum, positive for CD34, RB1, and STAT6, negative for SMA, P63, calponin, CK5, CK14, S100, CD31 (expect the small vessels) and desmin. Based on the morphology, together with the strong nuclear STAT6 immunostaining (Figure 6), a solitary fibrous tumor was diagnosed. Consideration was also given to a possible diagnosis of well-differentiated liposarcoma, but there would be more mitotic activity and atypia in that case.
Computed tomography of the thorax was negative for lymph adenopathy and showed no signs of pulmonary metastases. Wide excision of the mass was performed. The final pathologic assessment confirmed the diagnosis of a (low-risk) SFT. Therefore, adjuvant therapy was not indicated. A follow-up by mammography 3 months and 7 months after surgical excision showed no recurrence in the right breast.
Discussion
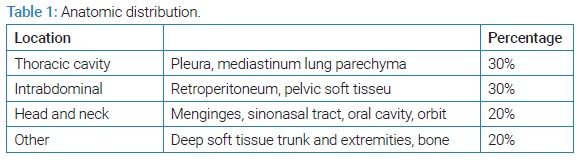
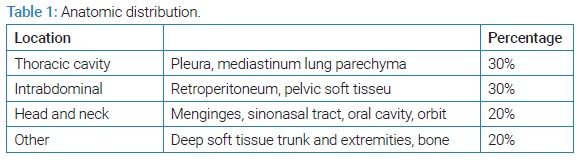
SFT is a rare fibroblastic mesenchymal neoplasm that most often arises from the visceral pleura. However, SFTs may occur at any anatomical site, including superficial and deep soft tissues and within visceral organs and bone (see Table 1) [1]. Although SFTs mostly emerge in the fifth to seventh decades, they may arise at any age.
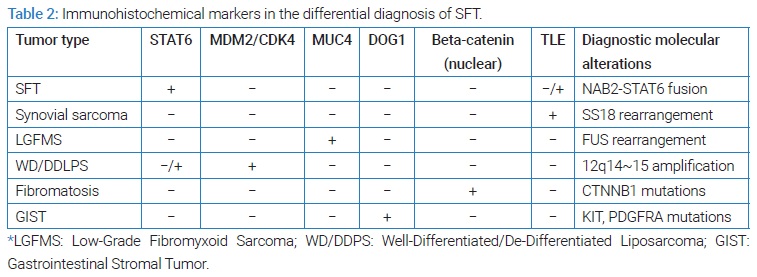
Literature research in MEDLINE, EMBASE, Google Scholar, and Pubmed was performed. The search terms solitary fibrous tumor, mamma, and breast were used. A wide range of soft tissue neoplasm must be considered in the differential diagnosis of breast spindles cell lesions, such as an inflammatory myofibroblastic tumor, nodular fasciitis, fibromatosis, reactive spindle cell nodule, leiomyoma, spindle cell metaplastic carcinoma and myoepithelioma. Microscopically, fibroblasts and connective tissue are organized in a so-called patternless design that is characterized by a random distribution of spindle cells and collagen fibrils [2]. Immunohistochemistry is a useful tool to differentiate SFT from all these other tumors; (see Table 2) [3,4]. SFT typically shows a strong and diffuse expression of CD34 and nuclear STAT 6 [1,2].
Jung et al. presented 2019 an overview of 27 cases of breast SFTs [5]. To our knowledge, three more case reports have been published since 2019 about SFT in the breast [6–8]. An overview of these 30 cases can be found in (Supplementary Table). The median size is noted between 7 cm–10 cm, so SFTs of de breast are relatively small (90% < 5 cm). The age range of the patients is between 38 years to 88 years [7–19].
This overview showed only 4 cases of breast SFT with a malignant course [5,7,8,16]. Most SFTs behave in an indolent clinical course; however, 10% to 22% SFTs have a malignant course [1]. Malignant behavior is characterized as an SFT with distant metastasis or local recurrence. Houdt et al. performed a retrospective analysis of 81 SFT patients who underwent surgical resection to analyze prognostic values, recurrence rate, and metastasis formation [17]. The local recurrence rate was 29%, with a median time to recurrent disease of 50 months. The metastasis formation was 34%, with a median time of 44 months to metastasis formation. Positive resection margins were the only factor significantly associated with the local recurrence rate [20]. Houdt et al. found that a high mitotic rate or a tumor size > 10 cm is associated with higher metastasis risk but not with local recurrence rate.
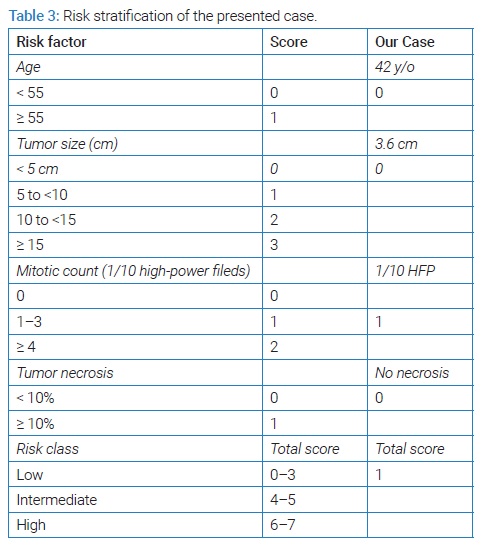
In 2017 Demicco et al. developed a risk stratification model to predict metastatic risk for SFT incorporating patient age, tumor size, and mitotic activity to predict the risk of metastasis, (see Table 3) [21]. The case presented was a patient with low metastatic risk. Demicco et al. revealed no metastasis at 10 years in the low-risk group. The intermediate-risk group had only a 10% risk of metastasis at 5 years and 10 years, and the high-risk group had a 73% risk of metastasis at 5 years. However, no data was provided on the metastasis outcome at 10 years in the high-risk group. In fact, limited studies are available on the late recurrence of SFTs [22], so prolonged follow-up (> 10 years) may be advisable.
Surgery is the first line of treatment for SFT, regardless of the risk profile. With a 10-year survival rate being reported between 54% and 89% after complete en-block surgical resection with clear margins. For the approximately 20%–30% of SFT cases at the limit of resectability, with distant metastasis or local recurrence, options for effective treatment are limited. Chemotherapy has typically been used in the advanced or metastatic setting. However, data on the activity of standard cytotoxic drugs are scarce. Anthracycline-based is the most investigated regimen with reported progression-free survival of 3 months–5 months and objective response rate ranging from 10.5% to 20% [23]. SFT cases could benefit from neoadjuvant Radiotherapy (RT). Haas et al. conducted a retrospective observational study of 549 SFT patients submitted to surgery alone or surgery plus postoperative RT with a median follow-up of 52 months [24]. Combining RT with surgery is significantly associated with a reduced risk of local failures after correction for the mitotic count and surgical margins (HR, 0.19: P = 0.029) but not with a longer overall survival (HR, 1.11: P = 0.704).
Conclusion
In conclusion, we report a rare case of a woman with a Solitary Fibrous Tumor of the breast with a low-grade risk for metastasis in the long term. Management of SFT in the breast should be discussed in a multidisciplinary soft tissue oncology board. Complete surgical resection is the gold standard of treatment, potentially followed with adjuvant radiotherapy or chemotherapy in high-risk patients. Follow-up should be long-term concerning the paucity of recurrence risk studies.
Declarations
Author contributions: Aarts F conceived of the presented idea. Hawinkels IMNW drafted the manuscript. Aarts F revised the article critically. Both authors read and approved the final manuscript.
Acknowledgments: None.
Informed Consent: Written informed consent was obtained from the patient for the publication of this report.
Funding: None.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Supplementary Table References
- Salemis NS. Solitary fibrous tumor of the breast: a case report and the review of the literature. Breast J. 2018;24(1):78–81.
- Song HS, Lee JY, Kim SY, Lee BH, Kim YS, Kim JW, et al. Solitary fibrous tumor of the male breast: a case report with imaging findings. Iran J Radiol. Epub 2018 Jun 17. http://doi.org/10.5812/iranjradiol.65607.
- Brenes J, Moreno A, Merchán MJ, Montes M, Ciudad MJ, Riola C, et al. Solitary fibrous tumor of the breast: a rare neoplasm. Breast J. 2018;24(3):417–419.
- Magro G, Spadola S, Motta F, Palazzo J, Catalano F, Vecchio GM, et al. STAT6 expression in spindle cell lesions of the breast: an immunohistochemical study of 48 cases. Pathol Res Pract. 2018;214(10):1544–1549.
- Magro G, Angelico G, Righi A, Benini S, Salvatorelli L, Palazzo J. Utility of STAT6 and 13q14 deletion in the classification of the benign spindle cell stromal tumors of the breast. Hum Pathol 2018;81:55–64.
- Magro G, Angelico G, Leone G, Palazzo J. Solitary fibrous tumor of the breast: report of a case with emphasis on diagnostic role of STAT6 immunostaining. Pathol Res Pract. 2016;212(5):463–467.
- Magro G, Bisceglia M, Michal M, Eusebi V. Spindle cell lipoma-like tumor, solitary fibrous tumor and myofibroblastoma of the breast: a clinico-pathological analysis of 13 cases in favor of a unifying histogenetic concept. Virchows Arch. 2002;440(3):249–60.
- Magro G, Sidoni A, Bisceglia M. Solitary fibrous tumour of the breast: distinction from myofibroblastoma. Histopathology. 2000;37(2):189–91.
- Park BN, Woo OH, Kim C, Cho KR, Seo BK. Recurrent solitary fibrous tumor of the breast: magnetic resonance imaging and pathologic findings. Breast J. 2018;24(6):1064–1065.
- Tsai SY, Hsu CY, Chou YH, Lai YC, Lin YH, Wang HK, et al. Solitary fibrous tumor of the breast: a case report and review of the literature. J Clin Ultrasound. 2017;45(6):350–354.
- Riola-Parada C, Jiménez-Ballvé A, Serrano-Palacio A, Cabrera-Martín MN, Brenes-Sánchez JM, Carreras-Delgado JL. Solitary fibrous breast tumour: contribution of 18F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol. 2017;36(1):61–62.
- Rhee SJ, Ryu JK, Han SA, Won KY. Solitary fibrous tumor of the breast: a case report and review of the literature. J Med Ultrason (2001). 2016;43(1):125–128.
- Han Y, Zhang Q, Yu X, Han X, Wang H, Xu Y, et al. Immunohistochemical detection of STAT6, CD34, CD99 and BCL-2 for diagnosing solitary fibrous tumors/hemangiopericytomas. Int J Clin Exp Pathol. 2015;8(10):13166–13175.
- Yang LH, Dai SD, Li QC, Xu HT, Jiang GY, Zhang Y, et al. Malignant solitary fibrous tumor of breast: a rare case report. Int J Clin Exp Pathol. 2014;7(7):4461–4466.
- Wignall OJ, Moskovic EC, Thway K, Thomas JM. Solitary fibrous tumors of the soft tissues: review of the imaging and clinical features with histopathologic correlation. AJR Am J Roentgenol. 2010;195(1):W55–W62.
- Rovera F, Imbriglio G, Limonta G, Marelli M, La Rosa S, Sessa F, et al. Solitary fibrous tumor of the male breast: a case report and review of the literature. World J Surg Oncol 2008;6:16.
- Meguerditchian AN, Malik DA, Hicks DG, Kulkarni S. Solitary fibrous tumor of the breast and mammary myofibroblastoma: the same lesion? Breast J. 2008;14(3):287–292.
- Falconieri G, Lamovec J, Mirra M, Pizzolitto S. Solitary fibrous tumor of the mammary gland: a potential pitfall in breast pathology. Ann Diagn Pathol. 2004;8(3):121–125.
- Bombonati A, Parra JS, Schwartz GF, Palazzo JP. Solitary fibrous tumor of the breast. Breast J. 2003;9(3):251.
- Salomão DR, Crotty TB, Nascimento AG. Myofibroblastoma and solitary fibrous tumour of the breast: histopathologic and immunohistochemical studies. Breast. 2001;10(1):49–54.
- Khalifa MA, Montgomery EA, Azumi N, Gomes MN, Zeman RK, Min KW, et al. Solitary fibrous tumors: a series of lesions, some in unusual sites. South Med J. 1997;90(8):793–799.
- Damiani S, Miettinen M, Peterse JL, Eusebi V. Solitary fibrous tumour (myofibroblastoma) of the breast. Virchows Arch. 1994;425(1):89–92.
- Nitta T, Kimura K, Tominaga T, Ikari A, Takashima Y, Hirata A, et al. Malignant solitary fibrous tumor of the breast. Breast J. 2021;27(4):391–393.
- Barco I, González C, Vallejo E, Pessarrodona A, Giménez N, García-Fernández A. Malignant solitary fibrous tumour of the breast mimicking a benign tumor. Clin Pathol. 2019;12:2632010X19868462.
- Dubois C, Nika E, Hoffmann P, Delouche A, Michy T, Philippe AC. Solitary fibrous tumor of the breast: A rare entity. Breast J. 2020;26(2):289–290.
- Dragoumis D, Desiris K, Kyropoulou A, Malandri M, Assimaki A, Tsiftsoglou A. Hemangiopericytoma/solitary fibrous tumor of pectoralis major muscle mimicking a breast mass. Int J Surg Case Rep. 2013;4(3):338–341.
- Cho WC, Mandavilli S. Intratumoral extramedullary hematopoiesis in solitary fibrous tumor of the breast. Breast J. Breast J. 2020;26(4):755–758.
Keywords
Solitary; Fibrous; Tumor; Breast; Fibroblastic; Mesenchymal; CD 34; STAT6
Cite this article
Hawinkels IMNW, Aarts F. Solitary fibrous tumor of the breast, a rarity: A case report and review of literature. Clin Case Rep J. 2022;3(8):1–8.
Copyright
© 2022 IMNW Hawinkels. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).