Are Red Stools after Red Dragon Fruit (Selenicereus costaricensis) Ingestion a Red Herring? – Case Report and Clinical Pearls for Recognition
* Eugene Kwong Fei Leong;
Yew A;
Lin NS;
-
* Eugene Kwong Fei Leong: Department of Surgery, University Surgical Cluster, National University Hospital, Singapore.
-
Yew A: Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
-
Lin NS: Department of Surgery, University Surgical Cluster, National University Hospital, Singapore.
-
Nov 02, 2022 |
-
Volume: 3 |
-
Issue: 8 |
-
Views: 153319 |
-
Downloads: 4694 |
Abstract
Haematochezia is the most common presentation of lower gastrointestinal bleeding and is a frequent diagnosis resulting in admission or outpatient attendance to gastroenterology and colorectal services. We report the first case of hospital admission with a benign presentation of blood-red stools following red dragon fruit ingestion and details of his evaluation, including biochemistries and endoscopy. We review the available literature regarding the fruit and betacyanins and offer clinical pearls to aid in differentiating this benign occurrence from more common and dangerous causes of red-colored stools.
Introduction
Haematochezia is the most common presentation of lower gastrointestinal bleeding and is a frequent diagnosis resulting in admission or outpatient attendance to gastroenterology and colorectal services. Common causes of per rectal bleeding include diverticular bleeding, hemorrhoids, colorectal malignancy, colonic and rectal polyps, colitis, inflammatory bowel disease, anal fissures, and vascular malformations [1,2]. Less common causes include hemorrhagic enteritis, bacterial or amoebic dysentery, vasculitides such as Henoch-Schonlein purpura, intestinal amyloidosis, and blood dyscrasias such as hemophilia or leukemia [3]. Known mimics of haematochezia with red discoloration of stool include ingestion of beets, red food coloring, cherry syrup, and medications such as cefdinir or rifampicin [3,4].
About half of patients with per rectal bleeding presenting to the emergency department are admitted, and 80% of lower gastrointestinal bleeding stops spontaneously. Overall mortality ranges from 2% to 4%, and the mean length of stay for admitted patients varies from 5.4 days to 7.2 days [1,2,5].
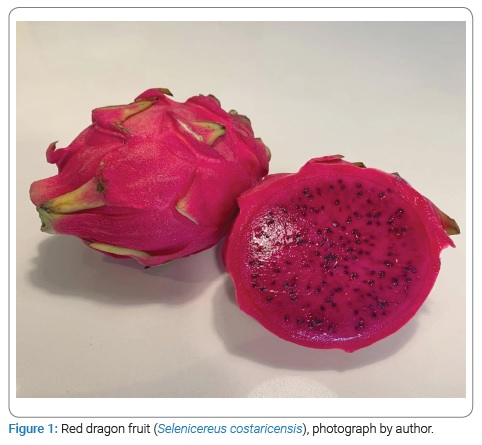
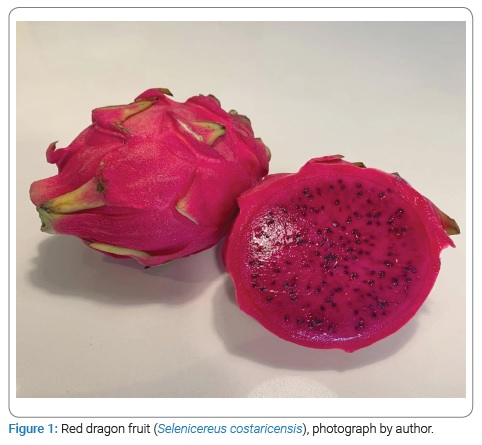
The red dragon fruit (Selenicereus costaricensis, previously Hyloreus costaricensis), also known as the Costa Rican pitaya fruit, belongs to the climbing Cactaceae family and most often takes on an oval shape (Figure 1). Several varieties of dragon fruit are grown – the pulp of the fruit may be red or white in color, and the skin can be red or yellow. The seeds of the fruit resemble that of the kiwifruit and are embedded within the fruit pulp [6].
The dragon fruit is cultivated and consumed worldwide due to its sweet flavor and increasing interest in pharmaco-therapeutic benefits as a “wonder fruit” [6,7]. The postulated activity of the fruit’s phytoconstituents includes nutraceutical (vitamins B1, B2, B3, and C), anti-oxidant (gallic acid, vanillic acid, syringic acid, protocatechuic acid, p-hydroxybenzoic acid, p-coumaric acid, lycopene, β-carotene), anti-microbial (betacyanin), anti-cancer (β-amyrin, β-sitosterol, stigmast-4-en-3-one) and anti-diabetic effects (flavonoids) [6–12]. In addition, Pitaya fruits are rich in micronutrients such as calcium and zinc while also containing high concentrations of betacyanin within the pulp and peel of the fruit [6].
To the authors’ knowledge, this is the first case report documenting hospital admission with a benign presentation of blood-red stools following red dragon fruit ingestion. We review the available literature regarding the fruit and betacyanins and offer clinical pearls to aid in differentiating this benign occurrence from more common and dangerous causes of red-colored stools.
Case Presentation
Our patient is a 74-year-old Chinese gentleman who was admitted to our hospital’s colorectal department with red-colored stools for evaluation of per rectal bleeding.
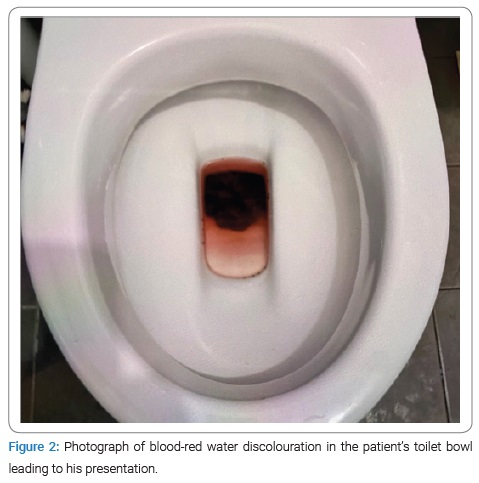
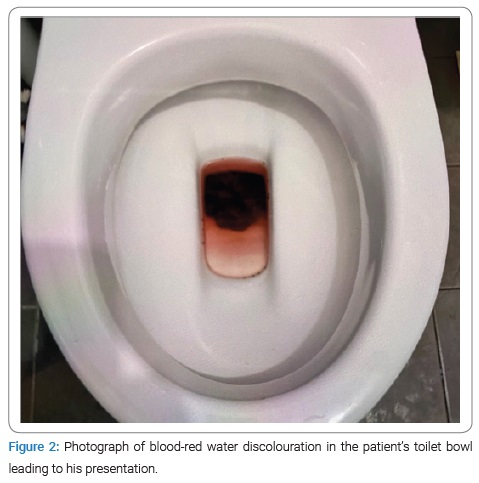
He reported a one-day history of bloodred water discoloration in his toilet bowl after painless defecation of formed stools (Figure 2) The patient did not notice the passage of fresh red blood or maroon stools. He denied anal pain, constipation, changes in bowel habits, tenesmus, abdominal pain, fever, or constitutional symptoms such as weight loss and anorexia. He reported that his urine appeared concentrated and orange in color but denied any bloodred urine. The patient reported a past medical history of well-controlled hypertension and ischaemic heart disease with previous percutaneous coronary intervention eight years ago. He was on aspirin anti-platelet therapy at 100 milligrams every morning and was a teetotaller and non-smoker. A colonoscopy performed nine years ago was unremarkable, and the patient had rubber band ligation performed for hemorrhoids in the same setting. He did not have any previous abdominal surgery or personal or family history of malignancy. The patient did not have a history of bleeding diathesis or hematological disorders. On closer review of his history, it was noted that the patient had consumed about three whole red dragon fruits in the preceding day as he had read that it would help with the prevention of developing type 2 diabetes mellitus. Abdominal examination was negative for tenderness, peritonism, masses, hernia, or surgical scars. On inspection of the perineal region, there was no anal fissure, perianal abscesses, or fistula tracts. There were red stains on digital rectal examination but no rectal masses or altered blood. Proctoscopy revealed congested internal hemorrhoids in the left lateral, right anterior, and right posterior columns, but there was no blood, contact bleeding, or stigmata of recent hemorrhage.
The patient was hemodynamically stable in the ward without tachycardia, hypotension, or fever. His initial hemoglobin was normal at 13.0 g/L and remained stable on a repeat reading the following morning. Platelet count and coagulation tests were within normal range. Urinalysis and microscopy did not reveal any haematuria. The patient was allowed a diet and discharged on the second day of admission without the need for fluid boluses or transfusion of blood products. Stool occult blood testing was not performed as the patient’s clinical picture was not suggestive of significant gastrointestinal bleeding, and early endoscopy had been arranged. The patient reported another episode of passing red stools on the day of discharge from the hospital but returned to the passage of brown-formed stools on day three of his initial presentation.
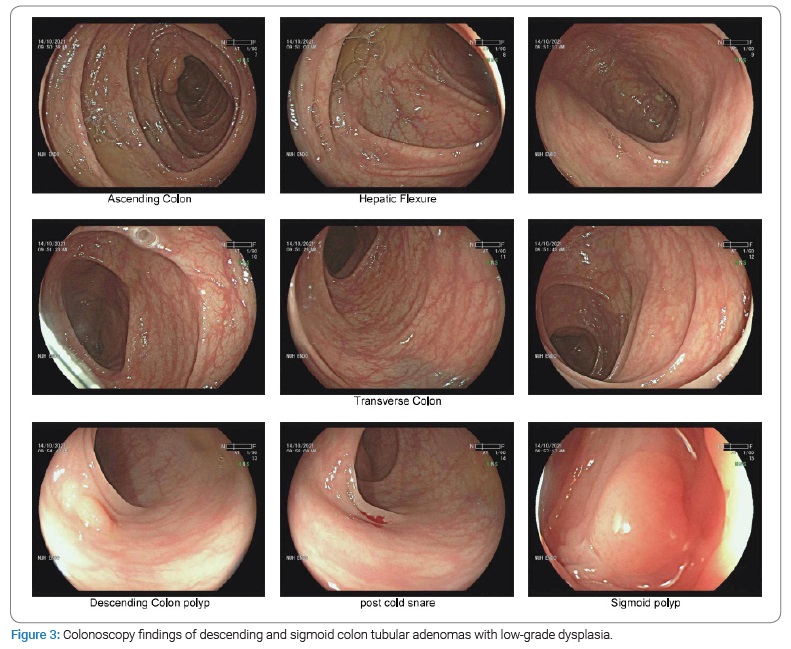
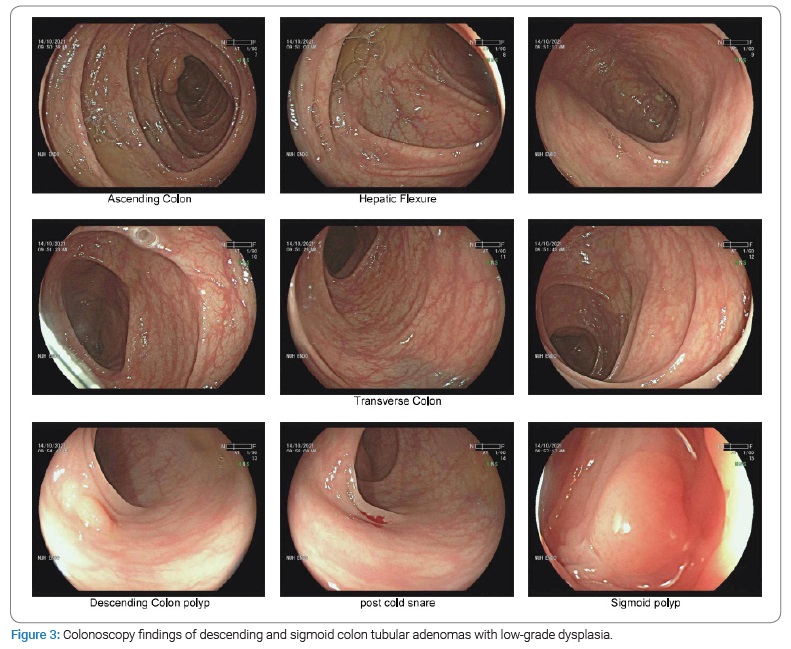
Outpatient colonoscopy revealed only two descending and sigmoid colon sessile polyps of two- and three-millimeter size, respectively (Figure 3). Notably, there was no colonic diverticula or cancer seen. Pathological assessment after polypectomy confirmed complete removal with clear margins of two tubular adenomas containing low-grade dysplasia.
He remained well at follow-ups 3 months, 6 months, and 12 months after his admission. Informed consent was obtained from the patient for the publication of his case and relevant clinical and endoscopic images for the purposes of research and medical education.
Discussion
Studies have demonstrated that the red-fleshed variety of dragon fruit has a high concentration of betacyanins, ranging between 25.6 milligrams to 49.9 milligrams per kilogram of fruit, depending on the location of origin [12]. Beetroots contain even higher concentrations of betalains, which are a heterogeneous group of readily water-soluble compounds, including red-violet betacyanin and yellow betaxanthins. In red beetroots, betanin and its isomer C15 betanin are the most prevalent betalains and give the fruit its typical red color. The concentration of betanin typically measures up to 300 milligrams–600 milligrams per kilogram of fruit [13]. As a result, 10%–14% of the general population develops beeturia or the excretion of red-colored urine after consumption of red beetroot fruit or juice [14]. The red discoloration results from the urinary excretion of betalains and their metabolites [15]. Studies have demonstrated that beeturia is more common in iron deficiency and co-ingestion of oxalate-rich food due to increased intestinal uptake of betacyanins [14,16].
While there have been no studies on the mechanism of stool discolouration with red dragon fruit ingestion, there have been two post-mortem case reports of purple colonic discoloration attributed to the ingestion of large amounts of beetroot [17,18]. The purple discoloration of the colon was deepest on surfaces exposed to intra-luminal fecal content. It was removed with dialysis, suggesting coloration by an ingested compound readily soluble in water, such as betanin. In addition, liquid chromatography high-resolution mass spectrometry confirmed three ingredients of beetroot in the colonic tissue – betanin, isobetanin, and aglycone betanidine [17].
With the growing recognition of dragon fruit as a “wonder fruit” due to the myriad of phytoconstituents and postulated pharmaco-therapeutic benefits [6–12], it is very likely that consumption of the fruit will continue to increase worldwide as the number of people seeking alternative strategies for the treatment of conditions such as cancer and diabetes increases alongside growing health literacy, including the patient in our case report.
It is thus valuable to recognize the potential presentation of red dragon fruit ingestion with red-colored stools, as described in our case report. While the patient in our case report was found to have congested internal hemorrhoids on a background of anti-platelet therapy for ischaemic heart disease, an alternative cause for his presentation is suggested by the following reasons:
- Short one-day history of symptoms with a strong temporal relation to ingestion of significant volumes of red dragon fruit.
- Absence of a preceding history of cirrhosis, peptic ulcer disease, diverticular bleeding, or recent bleeding hemorrhoids.
- Absence of hemodynamic instability, the necessity of fluid boluses or blood transfusion, decreased hemoglobin level on repeat phlebotomy, or frank passage of altered blood to suggest diverticular bleeding or massive upper gastrointestinal tract bleeding.
- Absence of contact bleeding of hemorrhoids or stigmata of recent hemorrhage upon bedside proctoscopy.
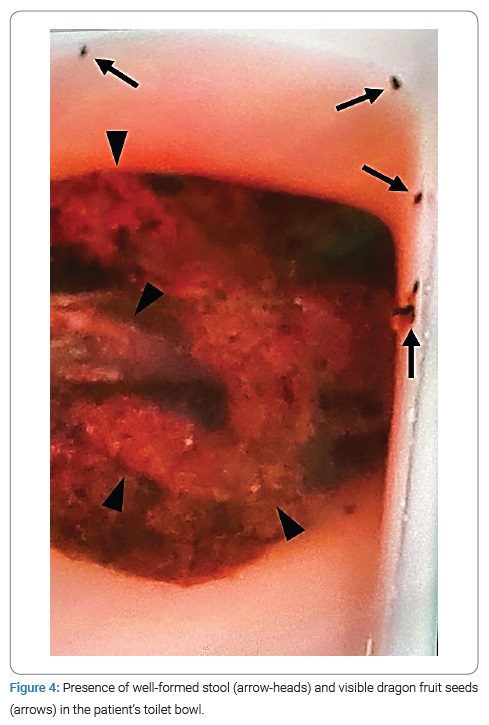
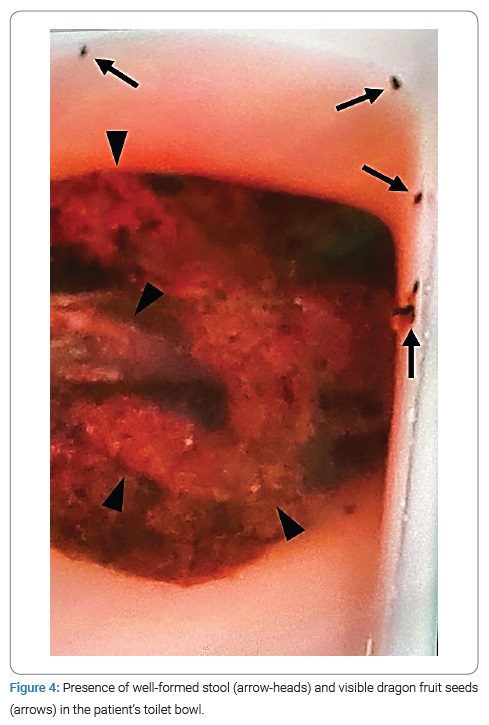
- Presence of formed stool and visible dragon fruit seeds in a photograph taken by the patient of his toilet bowl shortly before presenting to the hospital (Figure 4).
- Confirmation of an absence of diverticula, cancer, and vascular malformations during eventual outpatient colonoscopy.
Nevertheless, the authors recommend a thorough history and examination, including digital rectal examination and proctoscopy, hemodynamic and biochemical monitoring in a setting appropriate to the patient’s medical condition, and consideration of the patient’s symptom constellation and medical history when faced with admission or consult for per rectal bleeding. While early recognition may potentially spare the patient from invasive investigations such as endoscopy, red stool discoloration from significant ingestion of betacyanin-rich food such as red dragonfruit or beetroot remains a benign condition that should not be a forefront competitor of other more dangerous and insidious pathologies. Quantitative measurement of betalains such as betanin in serum, urine, or stool to support this benign diagnosis remains challenging and unlikely to see widespread employment in the clinical setting due to a complicated extraction process and the need for high-performance liquid chromatography with mass spectrometry detection [19]. Fecal occult blood testing was not performed on our patient as the clinical picture was inconsistent with significant gastrointestinal bleeding, and an early endoscopy had been arranged for him. While red dragon fruit has not been described to be among the peroxidase-rich fruits which confound guaiac-based fecal occult blood testing, the use of modern fecal immunohistochemistry testing will be useful in excluding true per rectal bleeding, should it be available [20]. Colonoscopy remains essential in colorectal cancer screening and in the diagnostic evaluation of haematochezia [1,2,5]. This was performed for the patient in our case report with the finding of benign colonic adenomas.
Declarations
Funding: No funding was involved.
Ethics Approval: No ethics review board or ethics approval was sought for this case report as the patient had provided consent and there was no human experimentation involved.
Consent to Participate: The case patient has given written and verbal consent for the publication of images and medical information for the furtherance of medical research and education.
Consent for Publication: The case patient has given written and verbal consent for the publication of images and medical information for the furtherance of medical research and education.
Availability of Data: Not applicable.
Code Availability: Not applicable.
Authors Contributions
Leong EKF was responsible for literature review, writing and paper revision.
Yew A was responsible for literature review, paper revision and critique.
Lin NS was responsible for formulation of the article, paper revision, critique and quality assessment.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Fok KY, Murugesan JR, Maher R, Engel A. Management of per rectal bleeding is resource intensive. ANZ J Surg. 2019;89(4):E113–E116.
- Barnert J, Messmann H. Diagnosis and management of lower gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2009;6(11):637–646.
- Pfeiffer ML, Du Pont H, Ochoa TJ. The patient presenting with acute dysentery--a systematic review. J Infect. 2012;64(4):374–386.
- Sharma T, Lamsal R. Cefdinir Induced Red Stool: Harmless Antibiotic Side Effect Awareness for Parents. Biomed J Sci & Tech Res. 2020;27(3).
- Schmulewitz N, Fisher DA, Rockey DC. Early colonoscopy for acute lower GI bleeding predicts shorter hospital stay: a retrospective study of experience in a single center. Gastrointest Endosc. 2003;58(6):841–846.
- Joshi M, Prabhakar B. Phytoconstituents and pharmaco‐therapeutic benefits of pitaya: A wonder fruit. Journal of Food Biochemistry. 2020;44(7):e13260.
- Dartsch PC, Kler A, Kriesl E. Antioxidative and antiinflammatory potential of different functional drink concepts in vitro. Phytother Res. 2008;23(2):165–171.
- Luo H, Cai Y, Peng Z, Liu T, Yang S. Chemical composition and in vitro evaluation of the cytotoxic and antioxidant activities of supercritical carbon dioxide extracts of pitaya (dragon fruit) peel. Chem Cent J. 2014;8(1):1.
- Charoensiri R, Kongkachuichai R, Suknicom S, Sungpuag P. Beta-carotene, lycopene, and alpha-tocopherol contents of selected Thai fruits. Food Chemistry. 2009;113(1):202–207.
- Wichienchot S, Jatupornpipat M, Rastall RA. Oligosaccharides of pitaya (dragon fruit) flesh and their prebiotic properties. Food Chemistry. 2010;120(3):850–857.
- Poolsup N, Suksomboon NJ, Paw NJ. Effect of dragon fruit on glycemic control in prediabetes and type 2 diabetes: A systematic review and meta-analysis. PLOS ONE. 2017;12(9):e0184577.
- Paśko P, Galanty A, Zagrodzki P, Luksirikul P, Barasch D, Nemirovski A, et al. Dragon fruits as a reservoir of natural polyphenolics with chemopreventive properties. Molecules. 2021;26(8):2158.
- Aztatzi-Rugerio L, Granados-Balbuena SY, Zainos-Cuapio Y, Ocaranza-Sánchez E, Rojas-López M. Analysis of the degradation of betanin obtained from beetroot using Fourier transform infrared spectroscopy. J Food Sci Technol. 2019;56(8):3677–3686.
- Watts AR, Lennard MS, Mason SL, Tucker GT, Woods HF. Beeturia and the biological fate of beetroot pigments. Pharmacogenetics. 1993;3(6):302-311.
- Watson WC, Luke RG, Inall JA. Beeturia: Its Incidence and a Clue to Its Mechanism. BMJ. 1963;2(5363):971–973.
- Sotos JG. Beeturia and iron absorption. Lancet. 1999;354(9183):1032.
- Roemmelt AT, Franckenberg S, Steuer AE, Kraemer T. Purple discoloration of the colon found during autopsy: Identification of betanin, its aglycone and metabolites by liquid chromatography–high-resolution mass spectrometry. Forensic Sci Int. 2014;240:e1–e6.
- Cserni G, Kocsis L. The case of the purple colon. Virchows Archiv. 2008;452(6):703.
- Clifford T, Constantinou CM, Keane KM, West DJ, Howatson G, Stevenson EJ. The plasma bioavailability of nitrate and betanin from Beta vulgaris rubra in humans. Eur J Nutr. 2016;56(3):1245–1254.
- Konrad G. Dietary interventions for fecal occult blood test screening: systematic review of the literature. Can Fam Physician. 2010;56(3):229–238.
Keywords
Gastroenterology; General surgery; Gastrointestinal bleeding; Case report
Cite this article
Leong EKF, Yew A, Lin NS. Are red stools after red dragon fruit (Selenicereus costaricensis) Ingestion a red herring? – Case report and clinical pearls for recognition. Clin Case Rep J. 2022;3(8):1–5.
Copyright
© 2022 Eugene Kwong Fei Leong. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).