Abstract
Prosthetic joint infection is an undesired complication following primary arthroplasty. Bacterial arthritis of the ankle following an aortoenteric fistula has been previously reported. However, to the best of our knowledge, there are no reports of Prosthetic Joint Infection (PJI) associated with bacteremia due to a Secondary Aortoenteric Fistula, as in this case report. Although rare, Secondary Aortoenteric Fistula should be considered when treating a prosthetic joint infection after aortic reconstructive surgery.
Abbreviations
EGD: Esophagogastroduodenoscopy; MRSE: Methicillin-Resistant Staphylococcus epidermidis; SAEF: Secondary Aortoenteric Fistula; TKA: Total Knee Arthroplasty; WBC: White Blood Cell
Introduction
Late infection after Total Knee Arthroplasty (TKA) is an infection that occurs in the joint replaced by TKA ≥1 year postoperatively [1]. The incidence of infection following primary TKA is reportedly between 0.7% and 1.0%, with 65% of infections occurring within the first postoperative year [2,3]. Joint infections after arthroplasty can result from the contiguous or hematogenous spread [4,5]. This article presents a rare case of late infection after TKA associated with bacteremia caused by Secondary Aortoenteric Fistula (SAEF).
Case Presentation
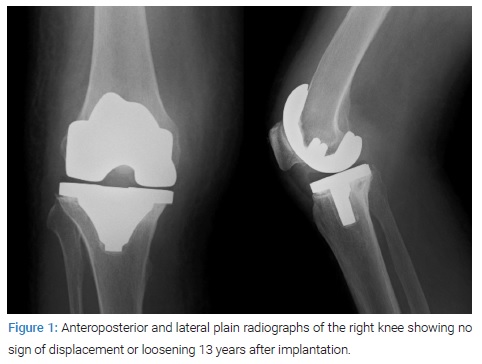
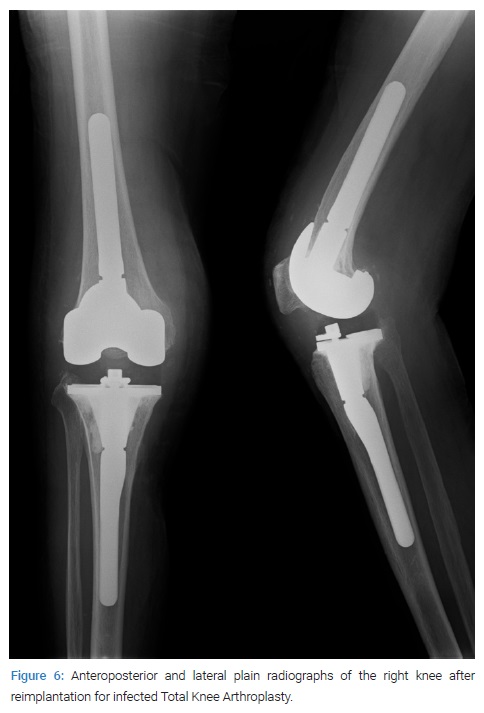
An 82-year-old woman, who had undergone right TKA 13 years ago, presented to our hospital with a 1-week history of worsening pain and swelling in the right knee. Her medical history also included an aortoiliac aneurysm treated with an aortic bifurcation graft and unstable angina treated with coronary stent placement three years earlier. Physical examination revealed a mild fever (37.6oC) and joint effusion in the right knee, and no wound was seen around the patient’s knee. There were no abdominal symptoms or oral disease that could cause sepsis. However, inflammatory markers in the blood test were significantly raised. The White Blood Cell (WBC) count was 13,630/µL, the C-reactive protein level was 38.25 mg/L, and the ESR was 115 mm. Radiographs showed no hardware complications or osteolysis (Figure 1). Late infection after TKA was suspected, and intravenous cefazolin (3 g/day) administration was initiated after collecting blood and joint fluid samples for microbiological analysis. The knee aspirate had a WBC count of 71,500/mm3. According to 2018 validated and score-based International Consensus Meeting (ICM) definition for PJI, this case did not meet the major criteria. However, blood tests showed elevated CRP and ESR and elevated leukocytes in the synovial fluid; thus, the patient was diagnosed with PJI according to that criteria [6]. Streptococcus anginosus, Haemophilusparain fluenzae, Neisseria species, and Veillonella species were isolated from the joint fluid, and Enterobacter cloacae from the blood culture. Intravenous cefazolin was changed to meropenem (2 g/day) due to the antibiotic sensitivity test results.
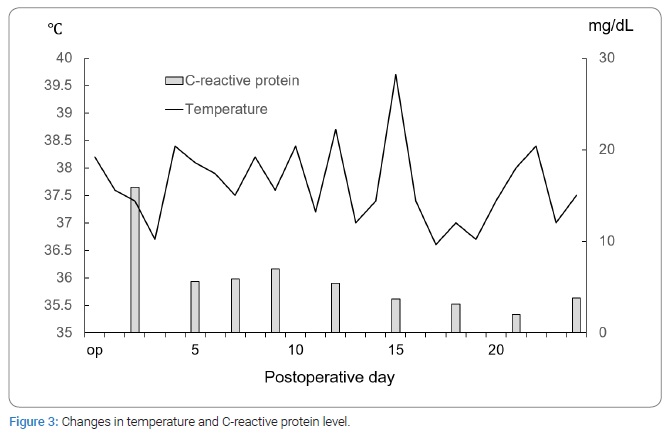
Irrigation and debridement were performed to treat the infection of TKA. Intraoperatively, extensive purulence was observed in the knee; hence, all components of TKA were removed, and antibiotic-loaded bone cement spacers were inserted (Figure 2). Cement spacers were made using 40 g of cement containing 4 g of imipenem/cilastatin. Intraoperative tissue and joint fluid were negative for infection. After the operation, knee pain and swelling improved. However, following the initial surgery, the patient complained of fever and chilled several times (Figure 3).

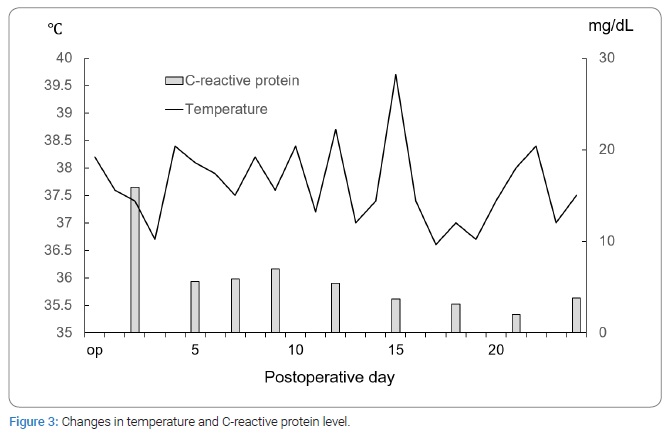
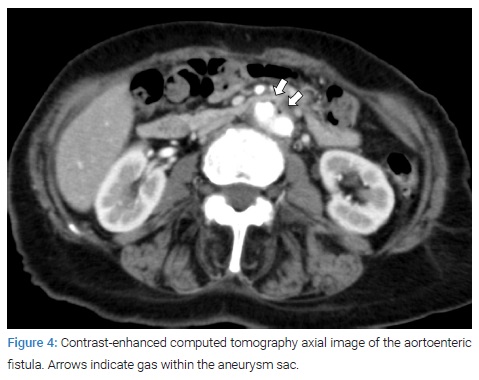
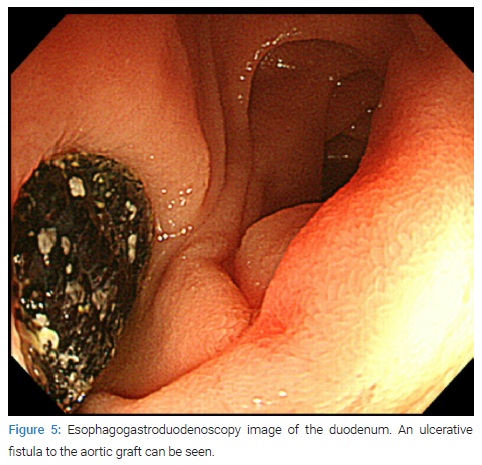
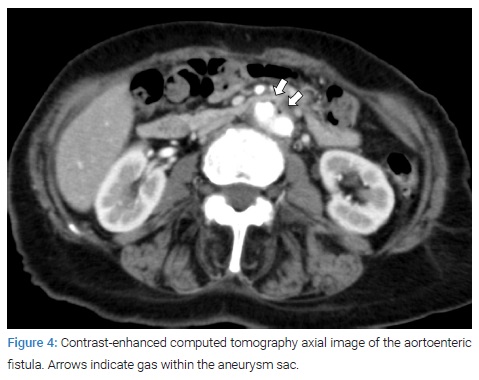
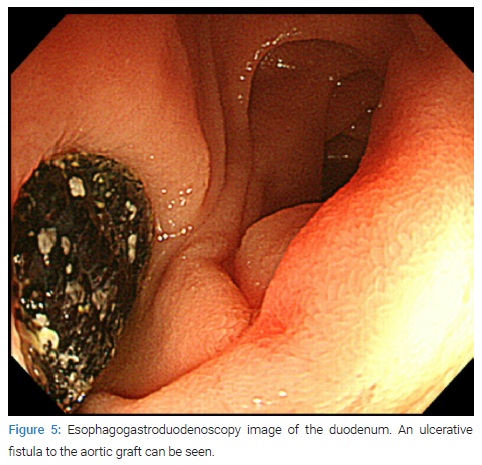
Methicillin-resistant Staphylococcus epidermidis (MRSE) was isolated from blood samples obtained on postoperative days 15 and 22 when the patient reported fever. We suspected other unknown infectious diseases, and contrast-enhanced thoracoabdominal computed tomography was performed on postoperative day 24, revealing gas buildup within the aneurysm sac (Figure 4). Emergency Esophagogastroduodenoscopy (EGD) was performed due to suspected communication between the duodenum and the aorta. EGD revealed an ulcerative fistula to the aortic graft in the duodenum (Figure 5).
The patient was diagnosed with SAEF. We performed primary closure of the duodenum, reimplantation of blood vessel prosthesis, and omentopexy. MRSE and Enterococcus faecium were isolated from the intraoperative tissue. Intravenous meropenem was continued until after cardiovascular surgery. After cardiovascular surgery, antibiotics were discontinued on post-operative week one.
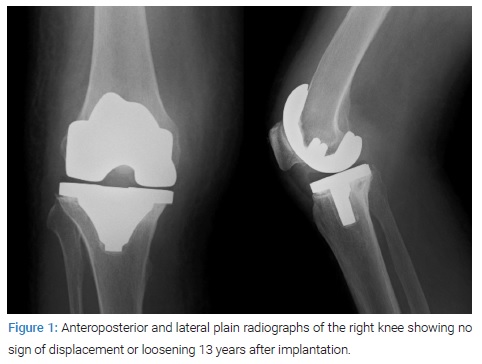
Two months after the aortic re-replacement, revision TKA was performed (Figure 6). Intraoperative cultures were negative. Meropenem (1.5 g/day) was used during the perioperative period of revision arthroplasty. No antibiotics were administered after the revision surgery. One month after the re-replacement operation, the WBC count was 5,610/µL, and the C-reactive protein level was 0.08 mg/L.
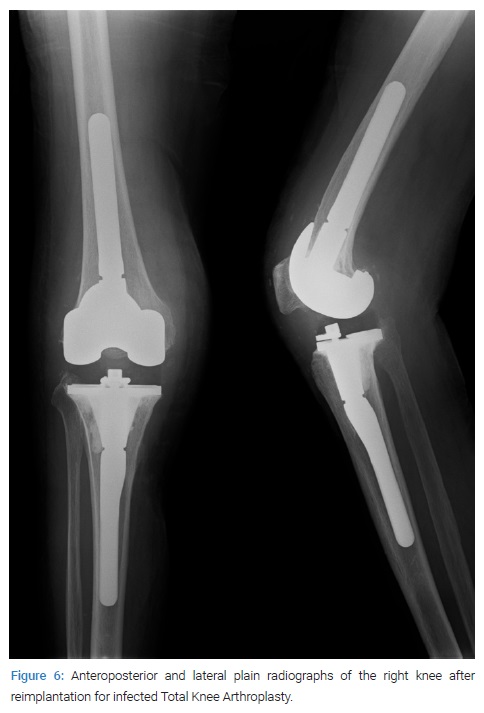
Five years after the revision TKA, the patient reported no clinical signs of recurring infection and could walk with a T-cane without pain. In addition, no evidence of loosening was seen in the radiographs.
Written informed consent was obtained from the patient for print and electronic publication of this case report. In addition, this study was approved by our institution’s institutional review board and ethics committee.
Discussion
Infection is one of the most undesired complications after TKA. To the best of our knowledge, this report presents the first case of late infection after TKA related to SAEF. Infection after TKA occurs as a result of contiguous or hematogenous spread [3]. Hematogenous spread seems to be caused by distant infective sources, with the most frequent sources of bacteremia being the skin (15%), teeth (11%), and gastrointestinal tract (9%) [7]. In this case, a bacterial culture of joint aspiration fluid showed positive findings for some bacterial species common to the normal flora of the oral cavity. The patient had no dental diseases. The source of bacteremia might be an intestinal fistula caused by a blood vessel prosthesis; however, the source of infection was difficult to determine. A previous study reported a case of ankle arthritis as a consequence of aortoenteric fistula [8]; however, the current study is the first report of a late infection after TKA related to aortoenteric fistula. If clinicians suspect a bacteremia associated with a prosthetic joint infection after vascular replacement, the aortoenteric fistula should be considered a potential bacteremia source.
An aortoenteric fistula is a communication between the aorta and the intestinal tract. The incidence of SAEF is estimated to be between 0.6%–2.0% [9]. Therefore, SAEF can occur as a complication of an aortic reconstructive surgical procedure, regardless of the implantation of an aortic stent graft. The cause of SAEF is mainly attributed to chronic perigraft infection or prolonged pressure on the bowel by grafts [9–12]. Gastrointestinal bleeding is the most frequent symptom in most SAEF cases, and sepsis occurs in approximately half of the patients on first consultation [13–15]. On contrast-enhanced computed tomography, the following features can be considered evidence of graft infection: peri-graft or intraluminal gas, perigraft soft-tissue thickening or fluid, loss of tissue planes, disruption of the aneurysmal wrap, and pseudoaneurysm or extravasation of contrast material [9,16]. Since viewing the distal portion of the duodenum with a standard upper endoscope is challenging, a longer endoscope (an enteroscope) should be used to visualize this area [17]. Graft removal and axillobifemoral bypass or graft removal and reimplantation of artificial graft are commonly performed for SAEF. However, the perioperative mortality rate is relatively high (22%–42%) [13]. Endovascular therapy has also been used in recent years, but additional surgery is required for gastrointestinal lesions [18].
The patient, in this case, received a cement spacer, and reimplantation of TKA was performed after diagnosis and treatment of the SAEF. Five years after TKA reimplantation, no signs of recurrent infection have been noted. The pathogenic bacteria, in this case, were S. anginosus, H. parainfluenzae, Neisseria species, and Veillonella species, which are unusual causative agents of infection after TKA; thus, the conventional treatment procedure for infection after TKA had to be selected.
Conclusion
Late infection after Total Knee Arthroplasty might be associated with Secondary Aortoenteric Fistula. Clinicians should suspect SAEF in patients with bacteremia after implantation of cement spacers with antibiotics for infections of arthroplasty and aortic reconstructive surgery.
Declarations
Ethics approval: This study was performed per the principles of the Declaration of Helsinki and was approved by our institution’s institutional review board and ethics committee.
Consent for publication: Informed consent was obtained from the patient to publish this case report. Availability of data and materials.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Knee arthroplasty; Aortoenteric fistulae; Prosthetic joint infection
Cite this article
Sakaguchi T, Mishima S, Ishizuka S, Oba H, Mizuno T, Kawashima I, et al. Late infection of total knee arthroplasty associated with aortoenteric fistulae. Clin Case Rep J. 2023;4(1):1–5.
Copyright
© 2023 Shinya Ishizuka. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).