Case Reports of Clinical and Histologic Wound Healing Response with Multi-Tissue Extracellular Matrix with Cost Analysis Compared to Negative Pressure Wound Therapy
* Diaz-Valadez FD;
Griffin K;
Sasse KC;
-
* Diaz-Valadez FD: Department of Surgery, University of Nevada-Reno School of Medicine, Reno, NV, USA.
-
Griffin K: Department of Surgery, University of Nevada-Reno School of Medicine, Reno, NV, USA.
-
Sasse KC: Department of Surgery, University of Nevada-Reno School of Medicine, Reno, NV, USA.
-
May 10, 2023 |
-
Volume: 4 |
-
Issue: 2 |
-
Views: 5624 |
-
Downloads: 2142 |
Abstract
Introduction: Complex wounds present a clinical challenge to achieve functional restoration. Treatment may involve numerous materials, personnel, and procedures and be expensive. Multi-Tissue Platform (MTP) graft (Xcellistem, Stemsys Bio) is a regenerative Extracellular Matrix (ECM) derived from multiple ECM sources with diverse non-collagenous proteins fibronectin, elastin, and laminin.
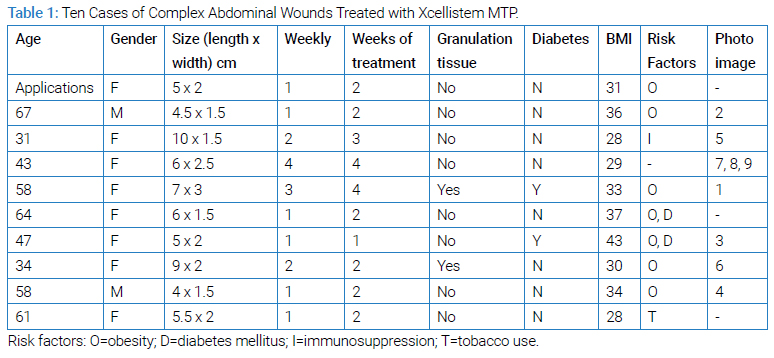
Case Series: Ten cases of complex abdominal wounds were treated with MTP material at a single institution until properly healed. In each case, the original surgery involved the placement of a multi-tissue graft, and three patients were treated with bedside graft material in subsequent weeks. Wound outcomes were examined, analyzed histologically, and used to compare the cost of care to Negative Pressure Wound Therapy (NPWT). In one case, a biopsy was obtained two weeks after the MTP graft application; the microscopic analysis was presented.
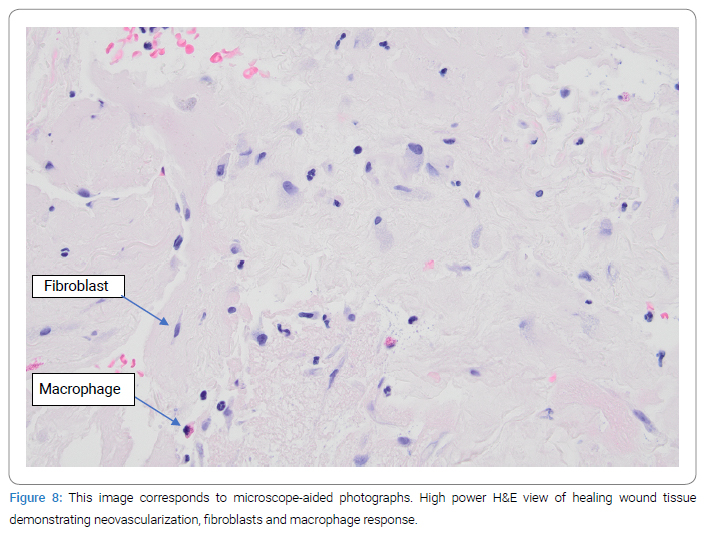
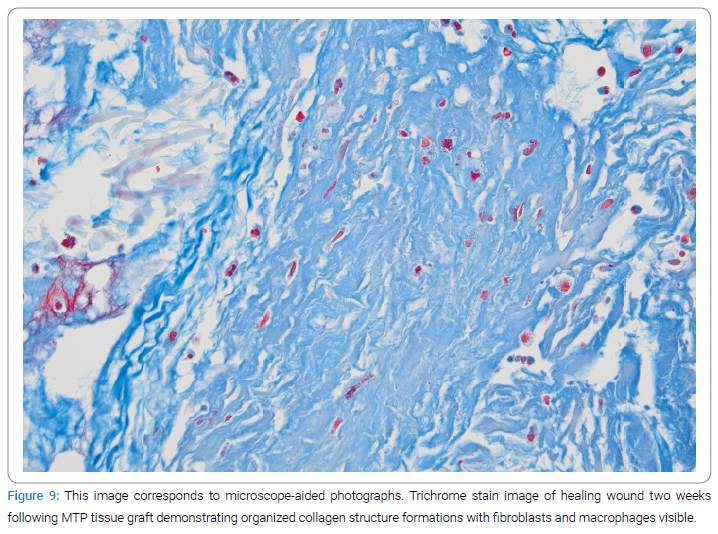
Results: Each patient achieved healing without complication; the median treatment time was 2.5 weeks. Xcellistem was applied to a representative wound for two weeks and later sampled for histological analysis. The sample contained a remodeling neutrophil response with collagen deposition, neovascularization, fibroblast presence, and macrophage presence and lacked foreign-body granulomas. The average cost of materials is $520 per week, compared to 533$ per week for NPWT at our institution.
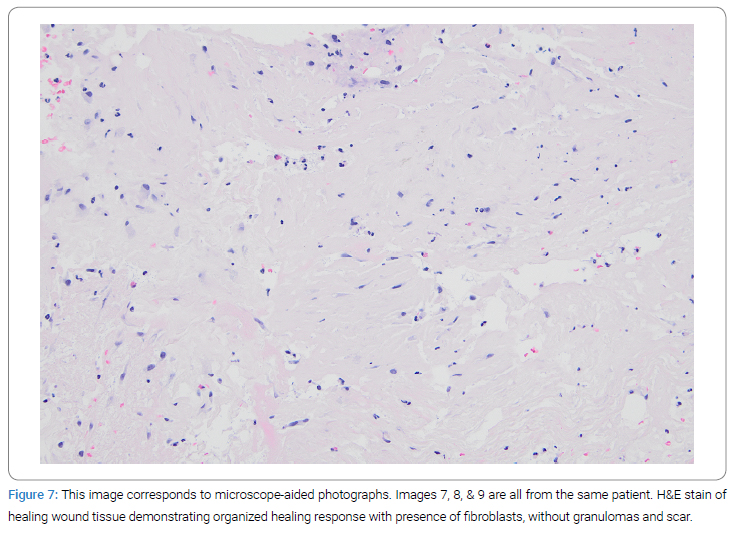
Discussion: Complex wounds represent a significant disability for patients as well as a challenging and costly treatment process. Similar to other studies, this case series found successful healing without complications, re-infection, or reoperation. Wound care with ECM materials may reduce the need for dressing changes, NPWT devices, and medical visits. The costs of MTP are lower than many bioresorbable materials or NPWT. The histological analysis illustrated a healing response that facilitated functional tissue remodeling instead of disorganized scarring.
Abbreviations
ECM: Extracellular Matrix; NPWT: Negative Pressure Wound Therapy; MTP: Multi-Tissue Platform
Introduction
Complex wounds (e.g., an acute or chronic injury to human skin tissue that does not respond to conventional treatments in a timely manner) present a clinical challenge to achieve complete healing and functional restoration. Wound cases that involve additional risk factors such as severe tissue necrosis, immunosuppression, tobacco abuse, Crohn’s disease, diabetes, and obesity pose increased risks of delayed healing, non-healing, reoperation, infection, and reinfection (i.e., when a person was infected, recovered, and later became infected again). In addition, the treatment of wounds is often costly, involving materials, personnel, and procedures. Xcellistem (Stemsys Bio) is a new regenerative extracellular Multi-Tissue Platform (MTP) graft matrix material derived from multiple Extracellular Matrix (ECM) sources. It has a diverse mix of ECM components, including substantial quantities of non-collagenous proteins such as fibronectin, elastin, and laminin [1]. Xcellistem has shown efficacy in facilitating the healing of wounds [1,2]. In this analysis, ten cases of complex abdominal wounds were treated with Xcellistem application at a single institution. The wound outcomes were examined, analyzed histologically, and used to compare the cost of care to Negative Pressure Wound Therapy (NPWT).
Case Series
In this retrospective cohort analysis, ten complex abdominal wall wounds were identified that required surgical debridement and the use of advanced wound therapy. All patients were given information about treatment options, the surgery, and associated risks. The ten patients agreed to the surgery and treatment plan. The complex wounds consisted of post-surgical wounds with significant tissue necrosis, locations of hardware removal, and panniculectomy dehiscence. In each case, the wound was debrided in the operating room with irrigation, sharp debridement of devitalized tissue, and followed by an assessment of the dimensions of the wound. Each wound was then treated with sterile MTP graft material sourced from Stemsys Bio and on the shelf at our hospital, which was applied in the operating room.
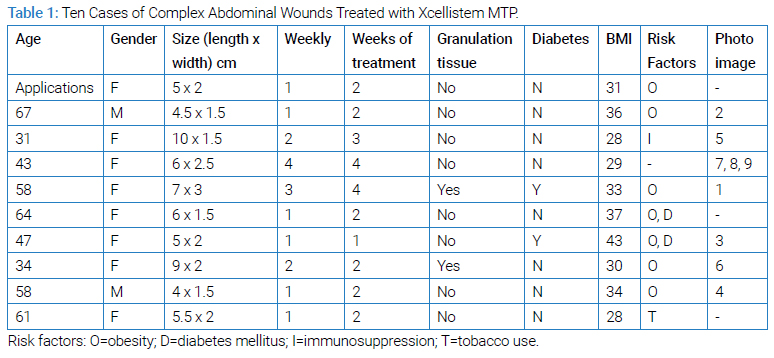
The dimensions of each wound and the patient characteristics are shown in (Table 1). No patient experienced sepsis or required prolonged hospitalization. In addition, none of the wounds were tumor-bearing or actively infected.
Results
During the initial surgery, wound debridement was performed, and the wound was assessed for its dimensions, depth, and any tunneling or recesses (Figure 1). MTP graft powder material was applied into each wound (Figure 2). The wound was then covered with Hydrogel or iodoform moist gauze, followed by a dry gauze dressing (Figure 3). The Xcellistem material and dressing were left in place for one week until the office examination approved the removal of the dressing (Figure 4).




In most cases, no further treatment was required, three-dimensional cavitary recesses exhibited a fill-in response, and a new dry gauze dressing was applied (Figure 5).

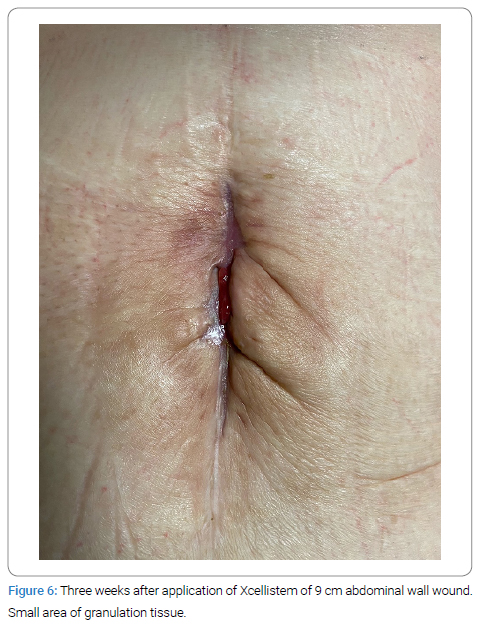
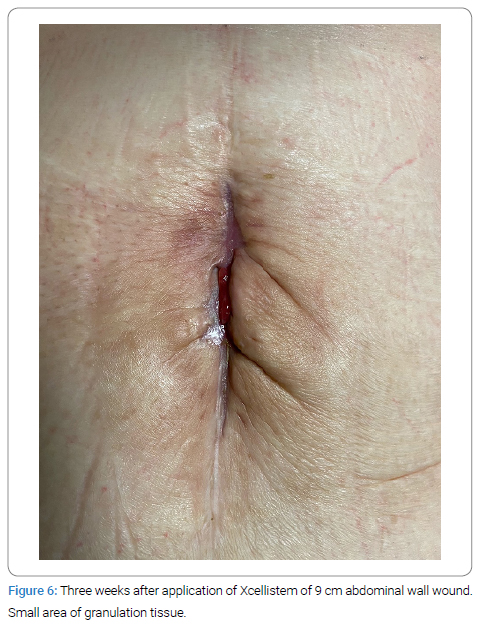
The median healing time for these complex wounds using weekly Xcellistem xenograft material applications was 2.5 weeks. In two cases, the wound healed with the formation of granulation tissue depicted in the image, which required no treatment (Figure 6). Patients’ safety was ensured by monitoring the long-term effects since each patient remained within our system. No patient required reoperation, antibiotics, or negative pressure devices, and none developed an infection. No patient is required to visit nurses, home wound care, visit additional wound centers, or the need to wear or carry a device. The cost for the material, including the initial graft and subsequent office treatments, was $520 per week.
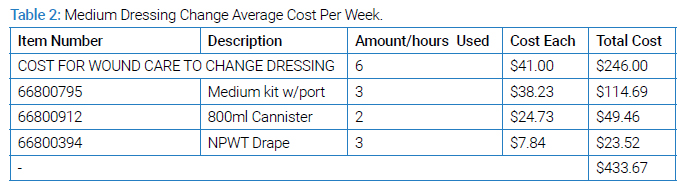
In the same center, an analysis was undertaken to examine the costs of wound care materials when using NPWT for comparable wounds. The costs per week of material for the NPWT protocol, utilizing three-times-per-week changes, for the Small, Medium (Table 2), Large, and Extra-Large systems are $410, $433, $782, and $932, respectively (excludes the cost of personnel labor).
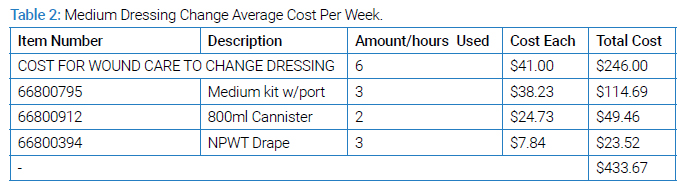
Based on the aggregate size measurements and the expertise of the wound care nursing staff at our institution, the ten cases represented here would initially require two small NPWT systems, three large, and five medium systems. The mean weekly cost for NPWT materials would be $533 per week.
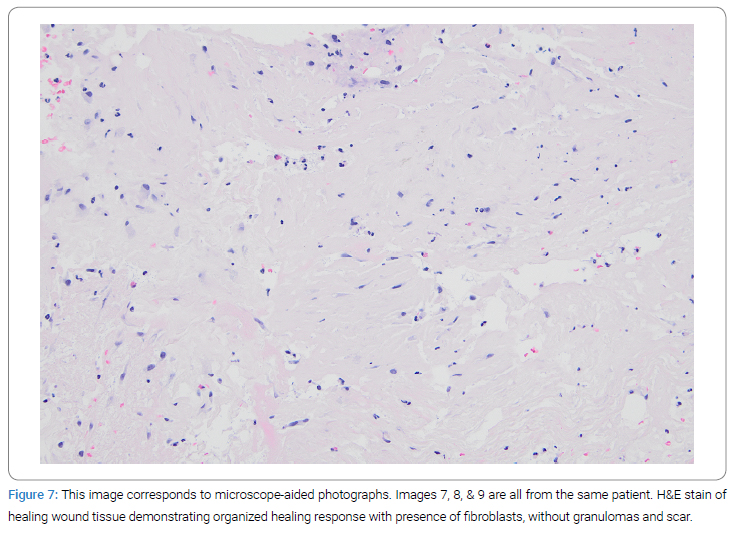
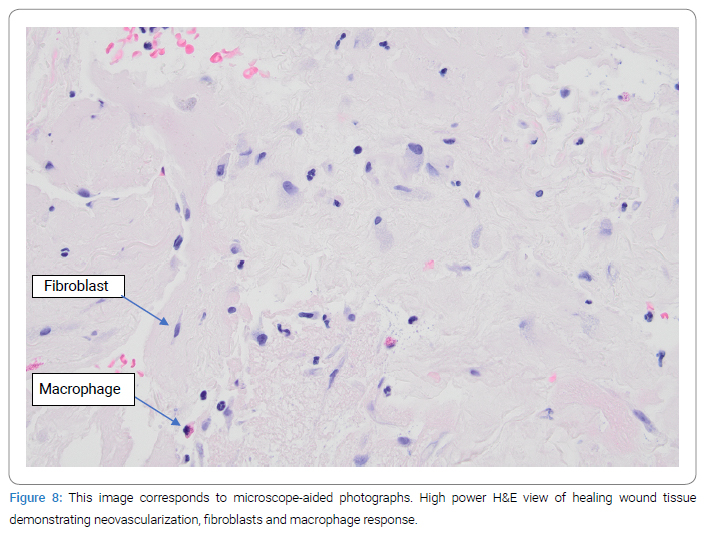
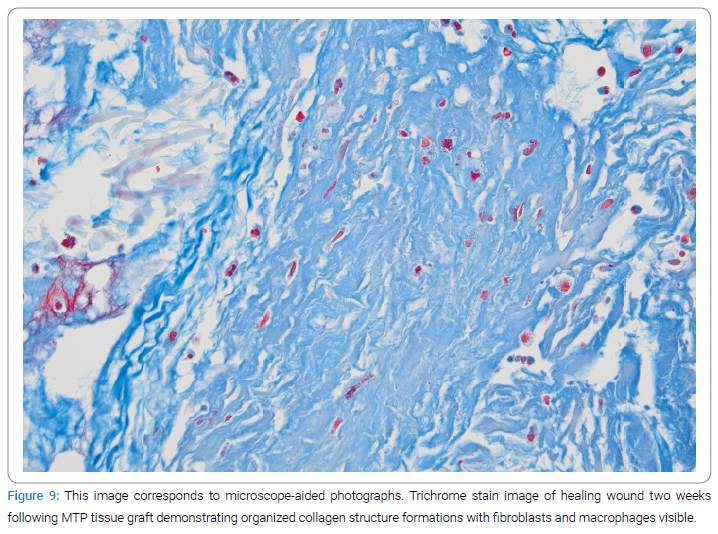
A biopsy of the wound that was in the process of healing was obtained from a single case/scar lesion two weeks after the placement of the MTP graft. The histological analysis illustrated a remodeling neutrophil response with collagen deposition, fibroblast, and macrophage presence, neovascularity, and lacking foreign-body granulomas (Figure 7). Hematoxylin and eosin stains on high power show an absence of granuloma, with evidence of neovascularization, fibroblast features (e.g., spindle-shaped cells, basophilic cytoplasm, and surrounding collagen deposition), and macrophage presence (Figure 8). Trichrome stains further illustrate the organized collagen deposition and functional tissue remodeling response (Figure 9).
Discussion
In this study, treatment of a diverse array of complex abdominal wounds using MTP graft application resulted in successful clinical healing without complications, re-infection, or reoperation. Areas of cavitary recesses remodeled and properly healed. The microscopic analysis demonstrates a favorable healing response.
ECMs have demonstrated effective healing outcomes throughout a wide range of wounds, such as open pilonidal wounds [3,4], infected wounds [2], hidradenitis suppurativa wounds [5], leg ulcers [6,7], combat military wounds [8], complex or chronic wounds [1,9–17], and large traumatic crush injuries [18]. Collagen matrices and bioactive signaling peptides have influenced the host response to favorably affect tissue remodeling and improve tissue functionality and speed of tissue recovery. Prior histologic studies of tissues treated with ECMs demonstrate less granulomas and scars with more functional remodeling, laminar collagen, and M2 macrophage response [4].
Current literature on innovative ECM treatments shows great promise in treating a wide variety of wounds. One study’s results demonstrate that patients treated with ECM material healed faster with a better success rate than historical controls for standard care [4], while another study specifically found that 95.7% of patient’s wounds closed within 12 weeks compared to 46% of those treated with standard care [6]. Numerous studies had a large, diverse set of wound etiologies that were successfully treated with proper ECM treatment [9,14,16,18]. Research teams have found evidence that proper ECM materials and treatment allow and promote the development of granulation tissue [16]. Although chronic soft tissue defects, infected wounds, and pilonidal sinus disease are infamous for their difficulty in healing, results from studies [2,3,12] have provided evidence that ECM material may improve the healing process, minimize common complications, and provide promising long-term outcomes compared to standard treatment. Good cosmetic outcomes, functional outcomes, and patient satisfaction were achieved when ECM materials were used for reconstructing defects with exposed vital structure [10] or used for surgical reconstruction of chronic soft tissue defects via tissue flaps [12]. One research team found that an ECM-derived bioscaffold may be a viable treatment for Volumetric Muscle Loss after demonstrating improvement in strength and function [13].
MTP powder has previously demonstrated effectiveness in achieving and accelerating wound healing across an array of tissues. The unique features of the multi-organ ECM include its potent chemotactic effect on host progenitor stem cells and macrophage M2 subtypes, which may play an essential role in the constructive remodeling of site-specific tissue [19]. In addition, MTP powder has been shown to be an effective wound treatment against wounds that have not responded to other treatments or are infected in a diverse range of wounds [1,2].
In this series, patients who have undergone treatment of their wounds using Xcellistem xenograft material did not have to carry or wear cumbersome negative pressure devices or tubing. In addition, none of the patients needed to perform dressing care at home, none were required to make frequent trips to a wound care center, nor did they have visiting nurses. Although the main focus of this case report was to examine the costs of the materials involved, it is worth noting that patients experience a lower burden of travel, intrusions, physical encumberments, and visits when using Xcellistem for wound healing than they would be using NPWT at this institution. Indications for MTP are for open soft tissue wounds, and contraindications thus far would be if a specific allergy appeared clinically. Treatment notes are the direct application of the MTP powder to wound surfaces, followed by the application of a moist dressing.
In this case series, ten abdominal wall wounds were treated with MTP powder and healed quickly without complication. Histologic analysis of a wound two weeks after MTP application shows a favorable remodeling response. In this single-center analysis, the median cost of materials per week using MTP graft is less than that of the costs per week using NPWT, based on contracted pricing within the same facility. Using the NPWT method, transportation and more personnel costs further increase the overall cost burden. Utilizing an MTP graft instead, a weekly or even bi-weekly dressing change is performed in the wound clinic or in the physician’s office, usually by a mid-level practitioner. Reducing the frequency of wound treatment seems to have little to no negative impact when weekly MTP graft application is the intended treatment plan. Thus, less material and less manpower costs are utilized than with NPWT, with excellent wound healing results.
Moving forward, future studies should aim for greater participant size and use a randomized, prospective, controlled trial comparing wound treatment protocols with NPWT or other approaches vs. Xcellistem. Using a randomized controlled trial may shed further light on the most cost-effective strategies for treating complex wounds. Rather than compare finances, future studies can examine therapeutic effects which may hold greater clinical significance. Future studies may also be worthwhile to explore cell surface markers on a wound via immunohistochemical detection to understand further the mechanism of promoting healing. Other molecules of research interest are inflammatory factors and expression of wound healing protein factors and their specific role in wound healing.
Conflict of Interest
Dr. Sasse serves on the Scientific Advisory Board of Regenerative Tissue Technologies Corporation.
References
- Kimmel H. The use of novel new multi-tissue biomaterial powder focused on cell signaling, in wound healing applications: a case series. Poster presented at: Symposium on Advanced Wound Care Fall; 2018 November 2-4; NV, USA. Fort Lauderdale: Wounds; 2018.
- Kimmel HM, Learn L, Corbisiero R. Infected wounds treated with multi-tissue platform (MTP) powder, a case series. [Internet]. Florida: Stemsys Bio; 2021.
- Chaffin AE, Dowling SG, Kosyk MS, Bosque BA. Surgical reconstruction of pilonidal sinus disease with concomitant extracellular matrix graft placement: a case series. J Wound Care. 2021;30(Sup7):S28–S34.
- Sasse KC, Brandt J, Lim DC, Ackerman E. Accelerated healing of complex open pilonidal wounds using MatriStem extracellular matrix xenograft: nine cases. J Surg Case Rep. 2013;2013(4):rjt025.
- Chaffin AE, Buckley MC. Extracellular matrix graft for the surgical management of Hurley stage III hidradenitis suppurativa: a pilot case series. J Wound Care. 2020;29(11):624–630.
- Bohn GA, Gass K. Leg ulcer treatment outcomes with new ovine collagen extracellular matrix dressing: a retrospective case series. Adv in Skin & Wound Care. 2014;27(10):448–454.
- de Fátima Cordeiro Petz F, Meier MJ, Roehrs H, Pott FS. Effectiveness of extracellular matrix dressings and topical agents in the treatment of leg ulcers: a systematic review protocol. JBI Database System Rev Implement Rep. 2018;16(5):1153–1160.
- Valerio IL, Campbell P, Sabino J, Dearth CL, Fleming M. The use of urinary bladder matrix in the treatment of trauma and combat casualty wound care. Regen Med. 2015;10(5):611–622.
- AbouIssa A, Mari W, Simman R. Clinical usage of an extracellular, collagen-rich matrix: a case series. Wounds. 2015;27(11):313–318.
- Bohn GA, Chaffin AE. Extracellular matrix graft for reconstruction over exposed structures: a pilot case series. J Wound Care. 2020;29(12):742–749.
- Cheung T, Laidley Z, Jones J, Wu S. Outcomes of an esterified hyaluronic acid matrix in the treatment of chronic lower extremity wounds: a case series. Wounds. 2018;30(12):367–371.
- Desvigne MN, Bauer K, Holifield K, Day K, Gilmore D, Wardman AL. Case report: surgical closure of chronic soft tissue defects using extracellular matrix graft augmented tissue flaps. Front Surg. 2021;7:559450.
- Dziki J, Badylak S, Yabroudi M, Sicari B, Ambrosio F, Stearns K, et al. An acellular biologic scaffold treatment for volumetric muscle loss: results of a 13-patient cohort study. NPJ Regenerative Medicine. 2016;1:16008.
- Lintzeris D, Vernon K, Percise H, Strickland A, Yarrow K, White A, et al. Effect of a new purified collagen matrix with polyhexamethylene biguanide on recalcitrant wounds of various etiologies: a case series. Wounds. 2018;30(3):72–78.
- Shin J, Park G, Lee J, Bae H. The effect of polydeoxyribonucleotide on chronic non-healing wound of an amputee: a case report. Ann Rehabil Med. 2018;42(4):630–633.
- Simman R, Mari W, Younes S, Wilson M. Use of hyaluronic acid-based biological bilaminar matrix in wound bed preparation: a case series. Eplasty. 2018;18:e17.
- Snyder D, Sullivan N, Margolis D, Schoelles K. Skin substitutes for treating chronic wounds. Rockville (MD): Agency for Healthcare Research and Quality (US); 2020.
- Collins RA, Zhu C, Daniel H, Puckett Y, Ronaghan CA. Crush injury with significant soft tissue loss managed utilising biological and dynamic tissue systems: a case study. J Wound Care. 2023;32(Sup2):S17–S19.
- Spiller KL, Freytes DO, Vunjak-Novakovic G. Macrophages modulate engineered human tissues for enhanced vascularization and healing. Ann Biomed Eng. 2015;43(3):616–627.
Keywords
Multitissue graft; Negative pressure wound therapy; Wound healing; Wound treatment, Xenograft
Cite this article
Diaz-Valadez FD, Griffin K, Sasse KC. Case reports of clinical and histologic wound healing response with multi-tissue extracellular matrix with cost analysis compared to negative pressure wound therapy. Clin Case Rep J. 2023;4(2):1–7.
Copyright
© 2023 Diaz-Valadez FD. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).