Abstract
Introduction: Squamous cell carcinoma of the parotid gland is a rare cancer comprising less than 1% of all salivary gland neoplasms. It is most often found on the palate.
We report a case of parotid localization that simulated necrotizing sialometaplasia.
Observation: The patient was MS, 24-year-old male who underwent surgery for necrotizing sialometaplasia of the left parotid gland, and it recurred three months after surgery. Reoperated for recurrence of a large left parotid mass. The histological reading of the surgical specimen concluded with a necrotizing sialometaplasia of the left parotid gland with doubtful deep borders. However, immunohistochemistry confirmed the doubtful diagnosis of squamous cell carcinoma of the parotid gland. Without further treatment, he died of hemorrhage.
Conclusion: Necrotizing sialometaplasia is a rare benign tumor of the salivary glands, most often located on the palate. Parotid localization can be the revealing mode of a squamous cell carcinoma whose diagnosis and treatment must be early.
Introduction
Salivary gland tumors are rare and account for approximately 3% of all head and neck tumors [1]. Most of these tumors affect the parotid gland in 25% of cases [2]. Squamous cell carcinoma of the parotid gland is a rare malignancy that accounts for less than 1% of all salivary gland neoplasms [3]. Parotid gland cancer is of great interest due to the diversity of clinical presentation and histologic and evolutionary features, which causes diagnostic difficulties and controversies in therapeutic treatment [2]. This study aims to describe a case of squamous cell carcinoma of the parotid gland, a histologic examination of which revealed necrotizing sialometaplasia, and to draw the attention of practitioners to this rare clinical entity.
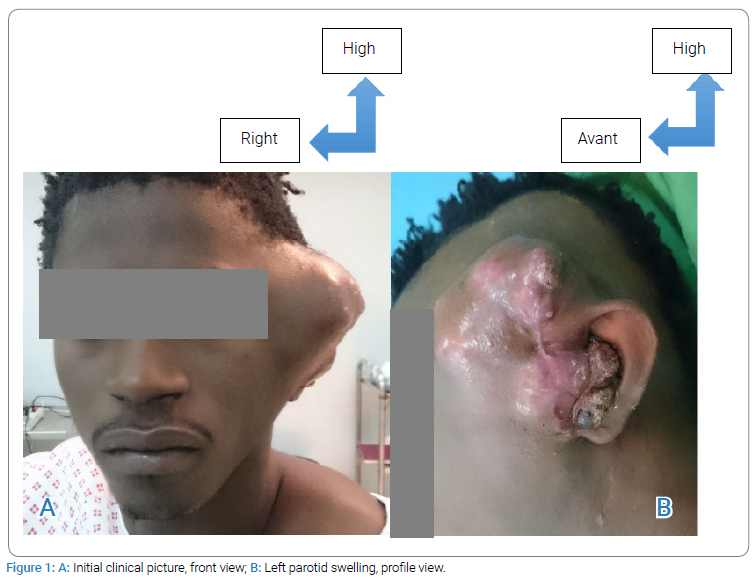
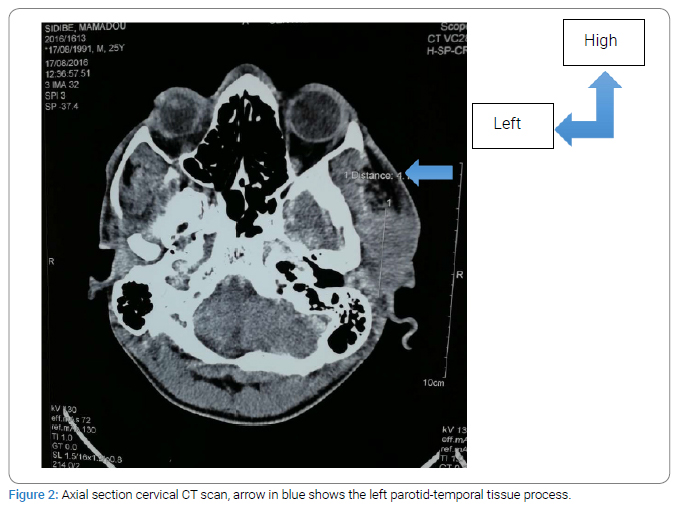
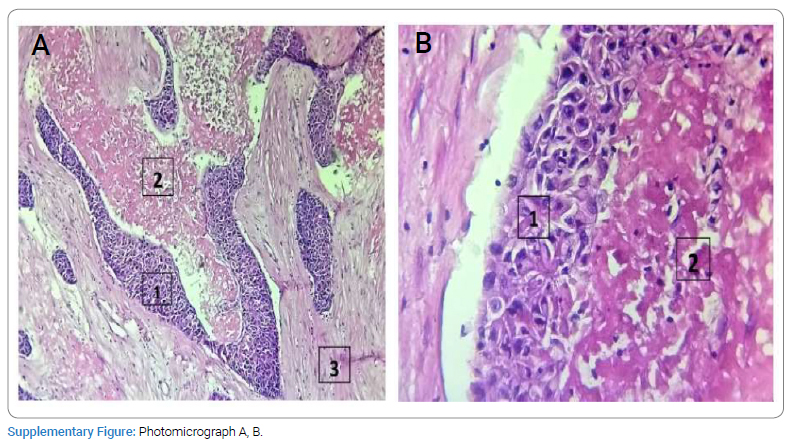
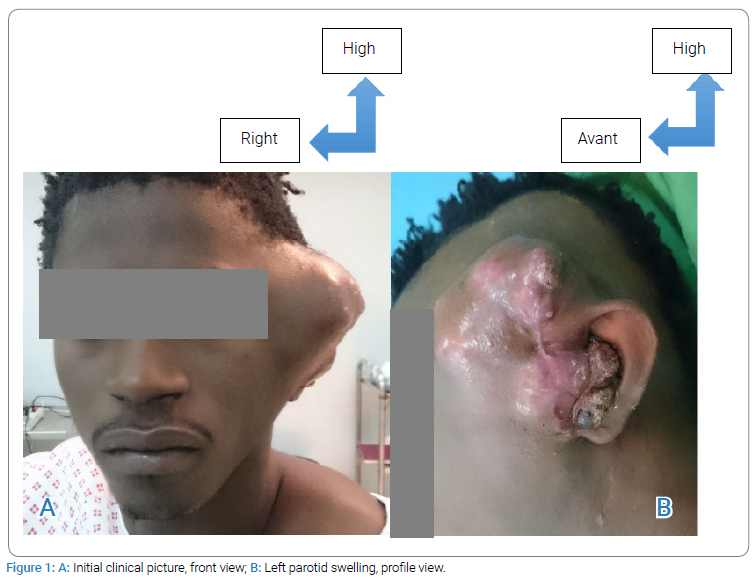
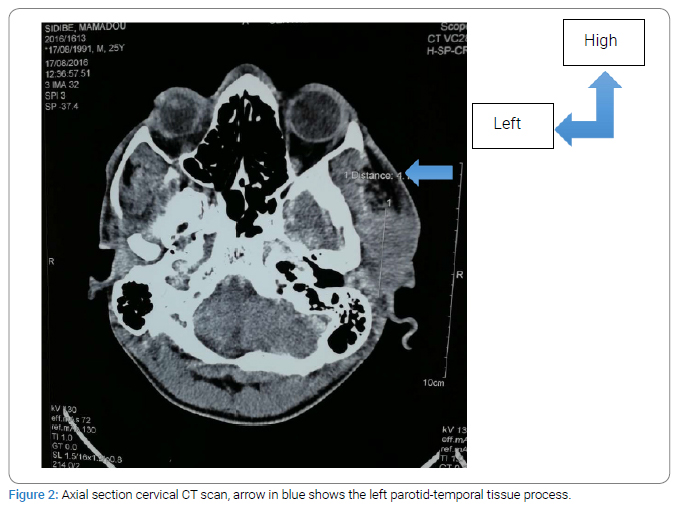
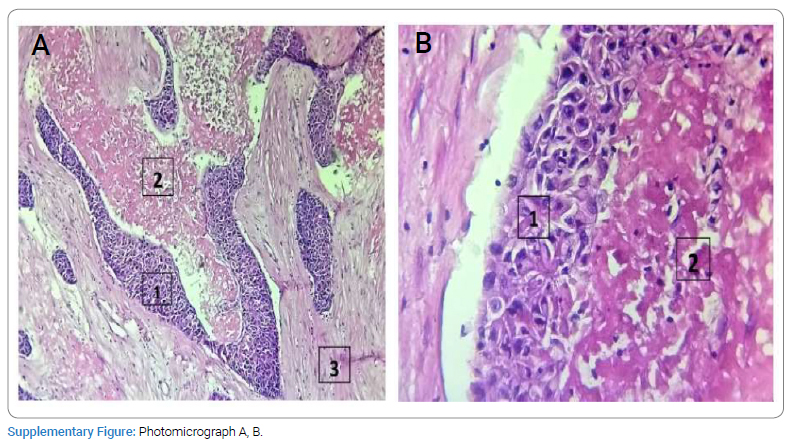
Medical examination: The patient is a 24-year-old male with multiple sclerosis, a history of conservative total parotidectomy of the left parotid gland, surgery performed at Piquinet Hospital for left parotid gland edema at nine months of its evolutionary continuation in the ENT department of the Idrissa Pouye General Hospital in Senegal with a histological result favoring necrotic sialometaplasia of the parotid gland. Clinical examination revealed a poly lobular left parotid-temporal mass infiltrating the skin opposite and filling the external auditory canal, which reappeared three months after surgery (Figure 1A, Figure 1B). The opposite parotid gland appeared healthy, and the lymph nodes were free. CT of the cervical spine showed a left parotid-temporal process measuring 58 mm x 41 mm x 22 mm with temporal bone lysis (Figure 2). A left parotidectomy with a homolateral triangular incision and transection of the temporomandibular branch of the facial nerve was performed (Figure 3A1, 3A2, Figure 3B). The postoperative course was complicated by a purulent infection, which was controlled with dual therapy for ten days. Histologic examination (Supplementary Figure) of the surgical material showed that the left parotid gland had necrotizing sialometaplasia with questionable deep borders. However, the case was submitted for PCR, and the decision to perform immunohistochemistry was important. Two blocks sent to the pathology laboratory of the European Hospital in Paris [CK5/6 (+) and P40/P63 (-)] confirmed the suspected diagnosis of squamous cell carcinoma of the parotid gland. Without further treatment, a year later, the disease progressed (Figure 4A, Figure 4B), and the patient died due to bleeding.


Discussion
The parotid gland’s Squamous Cell Carcinoma (SCC) is a rare malignancy with an estimated incidence of less than 1% of all salivary gland neoplasms [3]. This disease usually occurs in the sixth or seventh decade of life, mainly in men [4,5]. The literature reports an average age of 64 years and 72 years, with a male-to-female ratio 2:1 [6,1]. However, the peculiarity of our study is the occurrence of this tumor in a young patient in the second decade of life. This is contrary to the data presented in the study by Sahabi SM et al. in 2017 [1], where the average age of patients was 42 years, and there were almost 4 times more men than women. We did not find any risk factors for cancer in our patient. This is similar to the study by Bouaity B et al. [7] in 2016 in Morocco, who found no specific history in their patients. There is a clear difference in the study by Allouch I et al. in 2021 [8] in Rabat, who found that 15 patients (14%) had a risk factor for tobacco intoxication. In the 2013 study by Huang MW et al. [9], in most cases, parotid carcinoma manifests as a hard, painless mass that can be fixed or mobile, although about one-third of patients have a painful mass with or without facial paralysis. As in our case, the clinical examination revealed a painful mass infiltrating the surrounding skin without palpable adenopathy or facial paralysis that appeared nine months after the initial surgery, leading us to suspect a malignant rather than benign tumor. Contrary to the histologic result, which was in favor of necrotizing sialometaplasia of the parotid gland, which is an inflammatory ulcerative-ischemic necrotic lesion, it is most often localized in the palate, i.e., in 79% of cases, and only in 12% of cases - in the main salivary glands [10].
Three months after the start of treatment, a CT scan of the cervical spine was performed, which revealed a process in the parotid and temporal bone on the left without objective bone lysis. From a therapeutic point of view, given the continued progression and doubts about the histologic result and temporal bone lysis, we performed a left parotidectomy with a homolateral triangular incision. Macroscopically, the lesion appeared as a whitish poly lobular mass with a firm consistency surrounded by a highly inflammatory area similar to the consistency of wet sugar. Excision of the skin opposite showed lysis of the temporal bone with exposure of the dura mater of the temporal bone, affecting the cartilaginous auditory canal with the temporo-facial nerve, which was more or less carcinological confirmed. As in the literature, the treatment is radical surgery, postoperative radiation therapy, and follow-up périodique [6]. Despite proper treatment, preoperative facial nerve damage is an unfavorable prognostic factor: the recurrence rate within five years ranges from 10% to 25% [4].
Due to significant postoperative tissue loss and the suspicious nature of the tumor, the option of treating the wound by targeted excision was chosen.
The surgical material was re-submitted for pathologic examination, again concluding that it was necrotizing sialometaplasia with questionable deep borders and lack of margins. However, this condition may mimic a malignant lesion; clinically, at the ulcer stage, one may think of squamous cell carcinoma, but also the histological aspect very often leads to confusion with carcinomatous lesions in the background of areas of squamous cell metaplasia, which often appear as a continuity with epithelial ridges [11]. We found the same hypothesis in our surgical specimen, which was an infiltrating epithelial component on trabeculae of epidermoid cells in contact with extensive areas of ischemic necrosis.
In view of these diagnostic doubts, immunohistochemistry (IHC) was performed, which showed a positive result for cytokeratin CK5/6 and P40/P63(-), confirming the diagnosis of squamous cell carcinoma of the parotid gland. A year later, the patient experienced a tumor recurrence. However, total parotidectomy does not prevent further progression of the tumor due to its multiple growths. Postoperative radiation therapy is also recommended as it improves local disease control [4]. In our case, due to the patient’s low income, he was unable to take advantage of additional treatment. This led to tumor recurrence and decreased survival rate to 1 year in our patient. This is in contrast to the literature, where the five-year survival rate remains at 25%–30% [6].
Conclusion
Sialometaplasia is a benign hard palate lesion with an exclusive parotid location. However, it can be a manifestation of squamous cell carcinoma of the parotid gland, a malignant tumor with aggressive potential. Diagnosis and treatment should be early to avoid disfiguring surgeries and worsening the prognosis.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Squamous cell carcinoma; Necrotizing sialometaplasia; Parotid gland; Salivary glands
Cite this article
Diallo OA, Niang D, Randriamalala AN, Diouf MS, Diop A, Deguenonvo R, et al. Squamous cell carcinoma of the parotid gland simulating necrotizing sialometaplasia of the parotid gland in a case report. Clin Case Rep J. 2023;4(2):1–6.
Copyright
© 2023 Bay Karim Diallo. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).