Posterior Circulation Ischemic Stroke in a COVID-19 Patient: A Case Report
* Brenner-Muslera E;
Arellano-González C;
Moreno-López R;
Nader-Kawachi J;
-
* Brenner-Muslera E: Intern at Hospital Médica Sur, Mexico City, Mexico.
-
Arellano-González C: Department of Internal Medicine, Hospital Médica Sur, Mexico City, Mexico.
-
Moreno-López R: Department of Internal Medicine, Hospital Médica Sur, Mexico City, Mexico.
-
Nader-Kawachi J: Department of Clinical Neurology, Hospital Médica Sur, Mexico City, Mexico.
-
Jul 04, 2023 |
-
Volume: 4 |
-
Issue: 3 |
-
Views: 2116 |
-
Downloads: 1991 |
Abstract
The SARS-CoV-2 disease is associated with several systemic conditions, including those that comprise the cerebrovascular system. In addition, stroke associated with COVID-19 has been related to multiple immune and non-immune mechanisms leading to thromboembolic and ischemic phenomena. We present the case of an initially COVID-19-antigen-positive female patient with no apparent relevant history attending the emergency department with symptoms of posterior circulation stroke. The patient had a favourable evolution during her hospitalization, presenting a complete recovery.
Abbreviations
MRI: Magnetic Resonance Imaging
Introduction
The COVID-19 virus is associated with diverse pulmonary and extrapulmonary manifestations. Many of their pathophysiological mechanisms are still unknown. Neurological conditions associated with COVID-19 include transverse myelitis, seizures, Guillain-Barré syndrome, neuropathy, and ischemic stroke, mainly from the anterior cerebral circulation territory [1]. The COVID-19 symptoms are often mild at onset, but when neurological complications occur, a grim outcome can accompany them [2].
The mechanisms associated with thromboembolism and ischemia include immune-mediated thrombophilia and hypercoagulability states, alterations in the renin-angiotensin-aldosterone axis, cardioembolism, cardiomyopathy, and neurovascular damage [3].
In this report, we present the case of a woman who had mild flu-like symptoms for eleven days after a positive SARS-CoV-2 antigen test and arriving at the emergency department with clinical manifestations compatible with posterior territory circulation stroke.
Case Presentation
Background: This case involves a 50-year-old woman with a long-standing history of hypothyroidism who receives levothyroxine treatment. She was otherwise healthy, with no reported cerebrovascular risk factors or history of migraines. The patient received complete vaccination with three doses of Pfizer, with her last dose administered 18 months before the onset of her current illness.
Thirteen days before her admission, the patient had close contact with a confirmed COVID-19 case. Two days after the contact, she experienced a severe, non-throbbing headache, retro-ocular pain, myalgias, arthralgias, dry cough, and fever. These symptoms progressively worsened over four days and gradually improved over a similar period. A COVID-19 antigen test yielded a positive result on the fourth day after symptom onset. Three hours before admission to the emergency room, upon awakening, the patient reported a sudden-onset bilateral non-throbbing occipital headache. The pain rapidly intensified, reaching an unbearable level within one minute. The patient also developed dysarthria, vertigo, and ataxia. She denied the presence of tinnitus, phosphenes, nausea, or vomiting, and there were no disturbances in consciousness; a persistent cough was the only remaining infection symptom at the time of admission. Vital signs were within normal range.
Neurological examination: The patient´s neurological examination showed scanning speech, vertigo, and erratic eye movements with multidirectional nystagmus, ataxia, and dysdiadochokinesia of the upper and lower right limbs. The first NIHSS score was 2 points. Meningeal signs were negative. Due to the sudden onset of symptoms, and the preponderance of negative over positive cerebellar symptomatology, the clinical diagnosis on admission was a hemispheric cerebellar syndrome of probable vascular etiology rather than a basilar migraine-like episode.
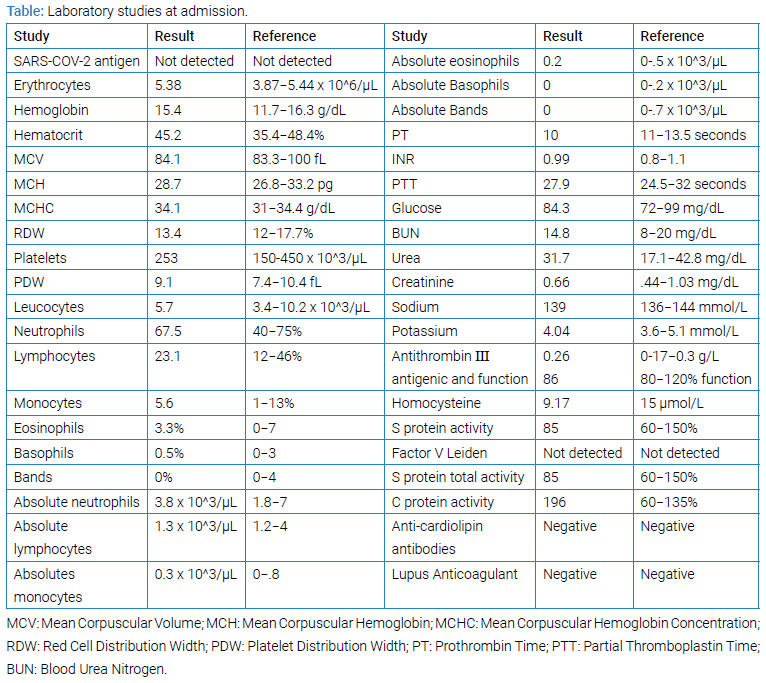
Clinical tests: Clinical tests performed upon arrival at the ER included a negative SARS-CoV-2 antigen test, a normal posteroanterior chest x-ray, and routine laboratories were normal (Table).
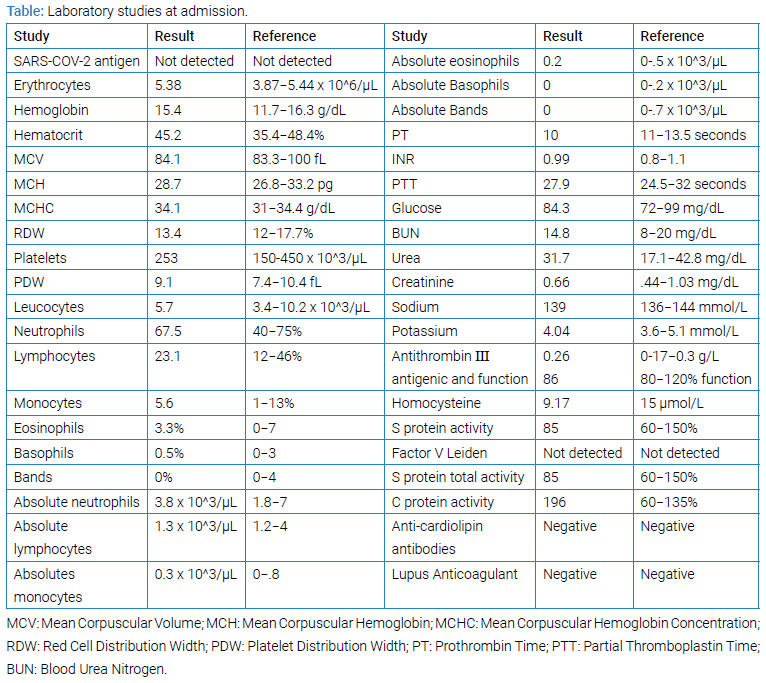
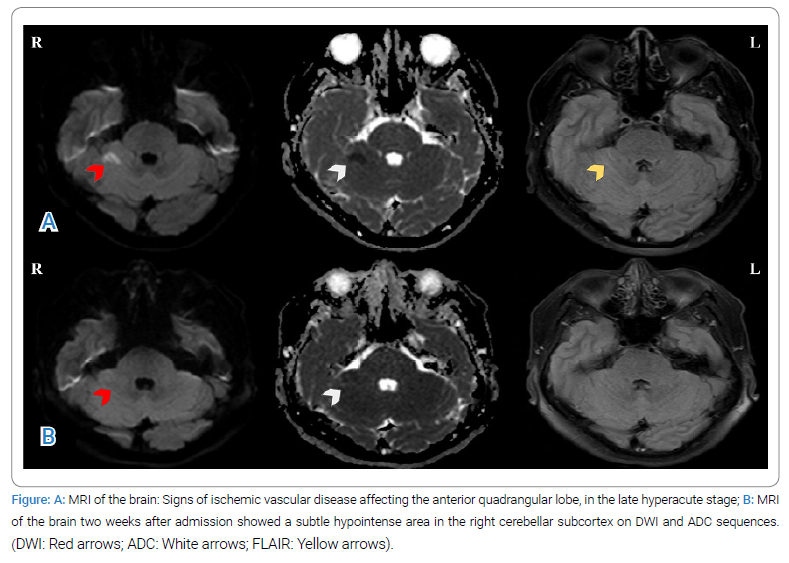
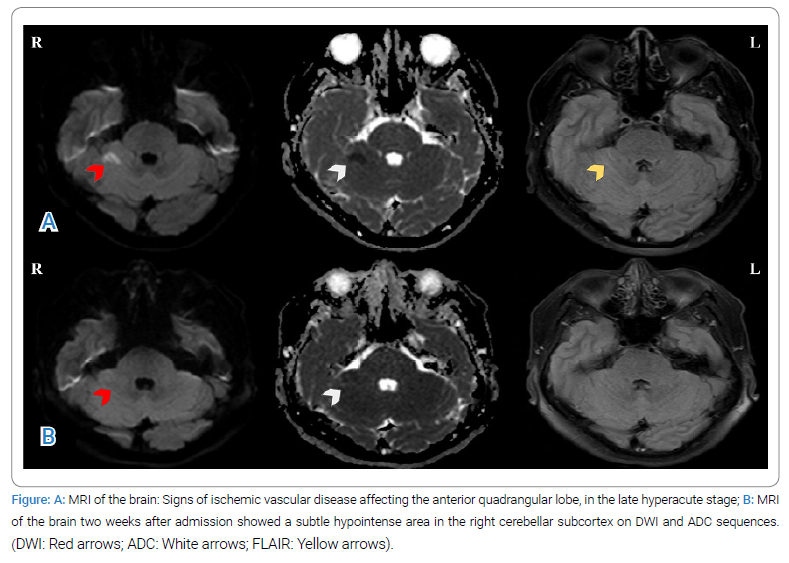
An MRI conducted 20 minutes later revealed areas of hyperintensity in the right cerebellar hemisphere on the DWI sequence, coincident with hypointensity on the ADC map sequences. Perfusion sequences showed increased mean transit time and decreased cerebral blood flow. These findings were congruent with a late hyperacute stroke in the territory of the right posteroinferior cerebellar artery (Figure A). Head and neck CT angiography revealed no abnormalities, and therefore, and therefore no further transcranial Doppler or cervical vessels ultrasonography examination was considered necessary to search for etiology, treatment, or follow-up. A 12-lead electrocardiogram demonstrated sinus rhythm without evidence of ischemic lesions or necrosis. Transthoracic echocardiography showed normal findings, and no interatrial septal shunts were detected with the contrast test. Given the normality of the transthoracic echocardiogram, transesophageal echocardiography was not considered for the etiological diagnosis.
Evolution: During hospitalization, constant cardiac and blood pressure monitoring was implemented. In the first 24 hours, the patient continued to experience headaches and paresthesia in the right arm while dual antiplatelet therapy began. The following day they marked a complete remission of symptoms. One day prior to discharge, an RT-PCR was conducted, yielding positive results for SARS-CoV-2. At the follow-up consultation one month after the acute event, the patient was asymptomatic without any deficits. A follow-up MRI performed two weeks later revealed a faint area of increased signal intensity in the subcortical region of the right cerebellum on FLAIR sequences (Figure B). No further COVID testing was conducted following the patient’s discharge.
Discussion
Recent literature on SARS-CoV-2 demonstrates that the condition is not limited to the respiratory system but has the potential to trigger systemic alterations in acute, subacute, and chronic phases [5]. Neurological manifestations range from signs and symptoms that do not impact life or functionality to severe conditions such as stroke, myelitis, or Guillain-Barré syndrome [6]. During the COVID-19 pandemic, ischemic and hemorrhagic stroke cases have been reported [7].
The present case presents specific demographic, clinical, topographical, and temporal characteristics that merit its analysis. Our patient has unusual demographic characteristics compared to other populations described throughout the pandemic. Generally, stroke patients are typically older than 66 years, male, and have cardiovascular comorbidities such as hypertension, diabetes, coronary syndrome, or atrial fibrillation [4]. However, in the present case, cardiovascular risk factors were not documented. Hematological studies conducted at hospital discharge to investigate procoagulant factors, including antithrombin III, factor V Leiden mutation, proteins C and S, antiphospholipid antibodies, and homocysteine, did not reveal any abnormalities. Therefore, the case was initially classified as an embolic stroke of undetermined origin [8].
Posterior fossa involvement is rare and reported in 3%–7% of all cases of COVID-19-associated stroke [9,10]. In Mexico, a study by Flores-Silva et al. showed that 0.8% of hospitalized COVID-19 patients presented with stroke, with most cases being ischemic and affecting the anterior circulation [11]. Prior to the pandemic, ischemia accounted for 52% of stroke cases in Mexico, with posterior circulation involvement at 17%. The high incidence of intracerebral hemorrhage was attributed to the prevalence of hypertension in the susceptible population [12,13]. Additionally, a study by López-Mena et al. analyzed stroke incidence among vaccinated patients, with a median age of 65 years and a median time of 2 days from vaccination to stroke. Acute ischemic stroke was the most common presentation, and most events occurred after the administration of the first dose [14].
Several pathophysiological mechanisms have been proposed to explain the development of thromboembolic events in COVID-19 patients. These mechanisms include increased coagulation pathway function, activation of proinflammatory and procoagulant pathways, endothelial damage, and subsequent thrombus formation [15]. Other pathogens, such as the Varicella zoster virus, have also been shown to induce vasculopathy, leading to thrombosis and ischemia through direct infection [16].
Vascular integrity disruption, bradykinin accumulation, and increased expression of adhesion molecules contribute to the development of a “procoagulant” endothelium [17]. Interleukin-8 levels have been linked to a sudden increase in the total number of neutrophils, which are associated with worse disease outcomes. Dapsone has shown potential in modulating cytokine levels and other proinflammatory factors, making it a promising approach for severe COVID-19 manifestations [18].
Hematogenous and neuronal dissemination of COVID-19 are proposed mechanisms that could explain the immune-mediated involvement of the nervous system. The widespread expression of the angiotensin-converting enzyme 2 receptor in the central nervous system, along with the compromise of the blood-brain barrier due to endothelial cell infection, leads to neuronal cell death. A vasculitic damage mechanism has also been hypothesized [6]. Large vessel disease, characterized by a high systemic inflammation pattern without evident coagulopathy, is associated with a better prognosis and lower disability [19].
The wide variability in the demographic and topographic characteristics of stroke in COVID-19 patients demonstrates the heterogeneity of the underlying pathophysiology. The most frequently described manifestations of COVID-19-associated stroke are hemiparesis (65.7%), altered mental status (51.4%), and dysarthria (34.3%). In the present case, only dysarthria was manifested [9]. Notable differences between our patient and the characteristics described in The Global COVID-19 Stroke Registry include a higher prevalence of ischemic stroke in males (37.9% of patients were female) and the absence of associated risk factors such as hypertension, obesity, or type 2 diabetes. Our patient manifested two of the three most common symptoms in patients with SARS-CoV-2 infection associated with stroke: fever (occurring in 55.2%) and cough (53.5%).
A case series by Meshref et al. highlighted the presence of overlapping coagulation alterations and inflammatory dysregulation in COVID-19-associated cerebrovascular events. For example, lymphopenia and elevated white blood cells were observed in almost all patients, and thrombocytosis and elevated procoagulant factors were also somewhat common findings. However, in this case, the patient did not show any abnormalities in the aforementioned laboratory tests [20]. Lastly, the patient was discharged completely asymptomatic, which is different from the 51% of patients who leave the hospital with severe disability rates [10].
Conclusions
We present a case of a woman who experienced a hyperacute stroke in the right PICA territory associated with SARS-CoV-2 infection. Despite thorough investigation, no clear etiology was identified.
As seen in other reports, the underlying mechanisms by which COVID-19 causes ischemic brain disease are not well understood. The distinctive clinical and demographic presentation of this case emphasizes the need for attentiveness to atypical neurovascular syndromes in the context of COVID-19. Furthermore, the disparity between negative antigen test results at the beginning of hospitalization and positive RT-PCR tests at discharge highlights the importance of exercising caution and employing more sensitive and specific early confirmation tests when necessary.
Acknowledgments
The authors would like to thank Alfredo Montenegro for aiding in the realization of this work.
Funding Sources: No funding was received for the realization of this work.
Ethics: Informed consent was obtained for this publication.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Sadeghmousavi S, Rezaei N. COVID-19 infection and stroke risk. Rev Neurosci. 2020;32(3):341–349.
- Tsuchiya T, Koizumi S, Tomioka A, Miyawaki S, Saito N. Acute ischemic stroke due to basilar artery occlusion with coronavirus disease 2019: a case report. NMC Case Rep J. 2021;8(1):579–585.
- Sagris D, Papanikolaou A, Kvernland A, Korompoki E, Frontera JA, Troxel AB, et al. COVID-19 and ischemic stroke. Eur J Neurol. 2021;28(11):3826–3836.
- Luo W, Liu X, Bao K, Huang C. Ischemic stroke associated with COVID-19: a systematic review and meta-analysis. J Neurol. 2022;269(4):1731–1740.
- Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032.
- Harapan BN, Yoo HJ. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19). J Neurol. 2021;268(9):3059–3071.
- Finsterer J, Scorza FA, Scorza CA, Fiorini AC. Ischemic stroke in 455 COVID-19 patients. Clinics (Sao Paulo). 2022;77:100012.
- Hart RG, Catanese L, Perera KS, Ntaios G, Connolly SJ. Embolic stroke of undetermined source: a systematic review and clinical update. Stroke. 2017;48(4):867–872.
- Yamakawa M, Kuno T, Mikami T, Takagi H, Gronseth G. Clinical Characteristics of stroke with COVID-19: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2020;29(12):105288.
- Ntaios G, Michel P, Georgiopoulos G, Guo Y, Li W, Xiong J, et al. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the Global COVID-19 stroke registry. Stroke. 2020;51(9):e254–e258.
- Flores-Silva FD, García-Grimshaw M, Valde´s-Ferrer SI, Vigueras-Hernández AP, Domínguez-Moreno R, Tristan Samaniego DP, et al. Neurologic manifestations in hospitalized patients with COVID-19 in Mexico City. PLoS ONE. 2021;16(4):e0247433.
- Ruiz-Sandoval JL, Chiquete E, Gárate-Carrillo A, Ochoa-Guzmán A, Arauz A; RENAMEVASC investigators. Spontaneous intracerebral hemorrhage in mexico: results from a multicenter Nationwide hospital-based registry on cerebrovascular disease (RENAMEVASC). Rev Neurol. 2011;53(12):705–712.
- Cantú Brito C, Ruiz Sandoval JL, Murillo Bonilla LM, Chiquete E, León Jiménez C, Arauz A, et al. Manejo agudo y pronóstico a un año en pacientes mexicanos con un primer infarto cerebral: resultados del estudio multicéntrico PREMIER. Rev neurol (Ed. impr.). 2010;641–649.
- López-Mena D, García-Grimshaw M, Saldivar-Dávila S, Hernandez-Vanegas LE, Saniger-Alba MDM, Gutiérrez-Romero A, et al. Stroke among SARS-CoV-2 vaccine recipients in Mexico: a Nationwide descriptive study. Neurology. 2022;98(19):e1933–e1941.
- Zakeri A, Jadhav AP, Sullenger BA, Nimjee SM. Ischemic stroke in COVID-19-positive patients: an overview of SARS-CoV-2 and thrombotic mechanisms for the neurointerventionalist. J Neurointerv Surg. 2021;13(3):202–206.
- Nagel MA, Mahalingam R, Cohrs RJ, Gilden D. Virus vasculopathy and stroke: an under-recognized cause and treatment target. Infect Disord Drug Targets. 2010;10(2):105–111.
- Perico L, Benigni A, Casiraghi F, Ng LFP, Renia L, Remuzzi G. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat Rev Nephrol. 2021;17(1):46–64.
- Diaz-Ruiz A, Nader-Kawachi J, Calderón-Estrella F, Mata-Bermudez A, Alvarez-Mejia L, Dapsone RC. More than an effective neuro and cytoprotective drug. Curr Neuropharmacol. 2022;20(1):194–210.
- Frisullo G, Scala I, Bellavia S, Broccolini A, Brunetti V, Morosetti R, et al. COVID-19 and stroke: from the cases to the causes. Rev Neurosci. 2021;32(6):659–669.
- Meshref M, Hewila IM, Khlidj Y, Korissi R, Shaheen N, Nashwan AJ, et al. COVID-19-associated cerebrovascular events: a case series study and a literature review of possible mechanisms. Case Rep Neurol. 2023;15(1):11–23.
Keywords
Cerebrovascular diseases; Ischemic stroke; COVID-19; SARS-CoV-2
Cite this article
Brenner-Muslera E, Arellano-González C, Moreno-López R, Nader-Kawachi J. Posterior circulation ischemic stroke in a COVID-19 patient: A case report. Clin Case Rep J. 2023;4(3):1–5.
Copyright
© 2023 Brenner-Muslera E. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).