Abstract
Acute Esophageal Necrosis is an uncommon disorder that is assumed to have a multi-factor etiology. We present a case of a 60-year-old man who was admitted to the hospital for the management of diabetic ketoacidosis with cellulitis. Two weeks after the surgical treatment of the abscess, he presented one episode of hematemesis. The upper endoscopy revealed a black mucosa with circumferential necrosis of the esophagus and duodenal ulcers. The patient was managed with supportive care and proton pump inhibitors, but unfortunately, he died two days later.
Abbreviations
AEN: Acute Esophageal Necrosis; DKA: Diabetic Ketoacidosis; EGJ: Esophagogastric Junction; EGD: Esophagogastroduodenoscopy; PPI: Proton Pump Inhibitor
Introduction
Acute Esophageal Necrosis (AEN) is a rare multi-name disorder, also called necrotizing esophagitis, black esophagus, or Gurvits syndrome. It is the consequence of the combination of factors that promote ischemia of the esophagus, acid reflux, and alteration of mucosal defenses. The incidence of AEN is approximately 0.01%–0.28% of patients undergoing esophagogastroduodenoscopy [1,2]. We report a case of a diabetic patient with necrotizing esophagitis.
Case Presentation
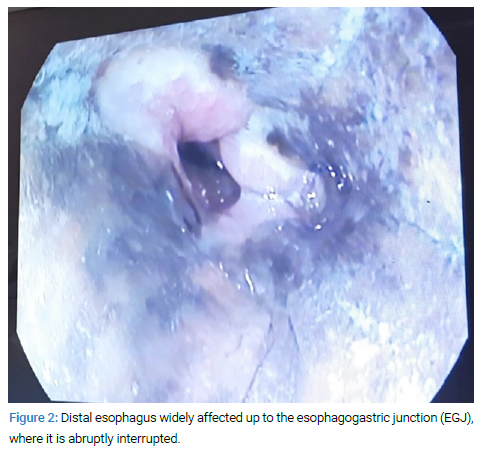
A male patient, in his sixties, with multiple cardiovascular risk factors (arterial hypertension, type 2 diabetes mellitus) and mild chronic kidney insufficiency presented to the Emergency Ward with a left inguinal cellulitis with surface necrotic tissue complicated by a subcutaneous abscess. An incision and drainage of the abscess were performed. A bacteriological examination of pus found Staphylococcus aureus. Two weeks later, he presented an episode of hematemesis (Table). The hemoglobin levels decreased from 7.2 g/dL to 5.9 g/dL. He received an intravenous normal saline infusion and blood transfusion. Intravenous omeprazole infusion was also started.
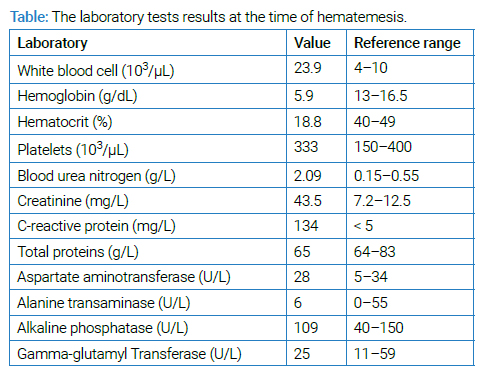
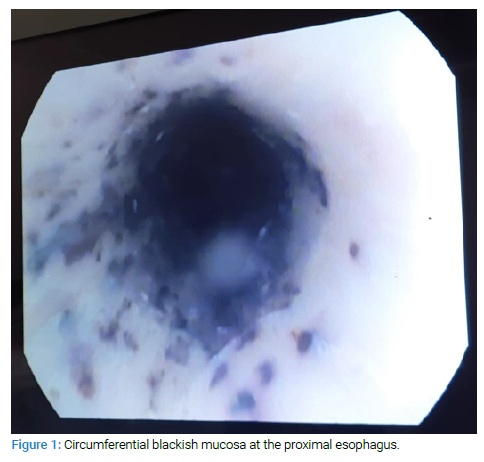
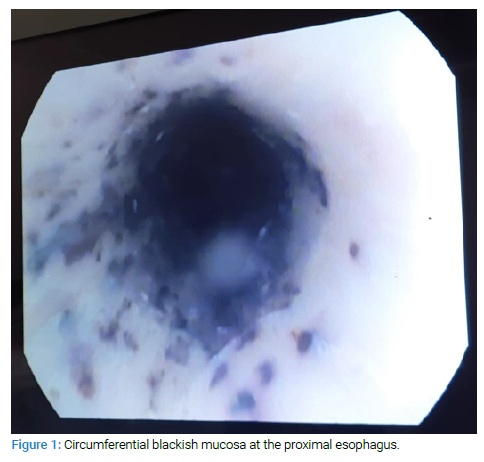
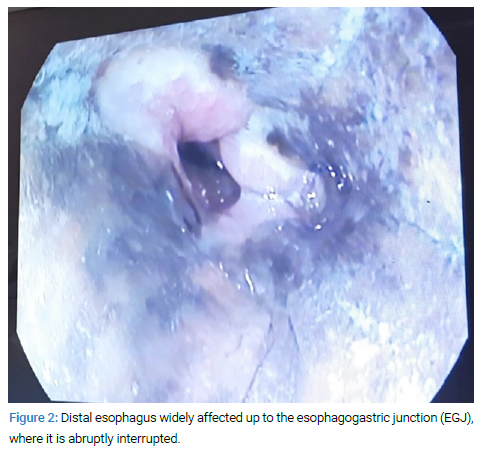
Urgent gastroscopy showed diffuse circumferential ulcerations and black mucosa affecting the esophagus from his proximal portion (Figure 1) to his distal portion, at 20 cm to 35 cm from the incisor teeth. The lesions progressively worsened. The lesions ended at the eso-gastric junction (Figure 2). Erosions and small ulcerations were detected in the duodenum as well.
In this case, the treatment was based on the use of antibiotics and a high-dose proton pump inhibitor associated with the management of ketoacidosis. Even if there was good glycemic control using insulin therapy and there was no rebleeding, the patient, unfortunately, subsequently succumbed to a septic shock after two days.
Discussion
This clinical syndrome usually affects males with an average age of 67 years [3]. It generally develops within the framework of severe systemic disease as a result of a combination of tissue hypoperfusion, gastric reflux, and altered defenses of the mucosa. Several risk factors have been identified, like cardiovascular risk factors (including diabetes mellitus, hypertension, and dyslipidemia), congestive heart failure, chronic kidney disease, chronic pulmonary disease, and liver cirrhosis. There are other risk factors less frequent such as malignancies and post-operative status [2,4]. Diabetic ketoacidosis may unleash AEN. DKA can cause low circulatory volume on its own by osmotic diuresis leading to a deep loss of fluid. In addition, DKA may induce gastroparesis, causing an increase in gastric reflux and subsequent mucous lesions.
It should be noted that COVID-19-related thrombosis can contribute to ischaemic lesions in the distal esophagus. Therefore COVID-19 infection can be added to the list of AEN risk factors [5]. Schizas et al. study showed that the distal esophagus is almost constantly affected (92.9%), with frequent progression of the disease to the middle part of the esophagus (64.3%) [6].
The distal third of the esophagus is the most vulnerable and easily affected segment because of its lower blood supply. Duodenal lesions might also be noticed because of the presence of common branches depending on the coeliac plexus [3].
The classic clinical signs are hematemesis and/or melena with abdominal pain, which may be associated with other signs like dysphagia and vomiting [7]. The development of AEN is thought to be rapid; that is why clinicians should consider AEN and carry out timely EGD if a diabetes patient with a severely elevated glucose level complains of unendurable heartburn, even when signs of upper gastrointestinal bleeding are absent or a recent EGD was unremarkable [8].
The classic endoscopic presentation is the black appearance of the distal esophagus with a clear limit of esophageal necrosis at the gastroesophageal junction. Ulcerations and esophageal necrosis are often seen after ingestion of the irritant and caustic product, which is why proper questioning should be undertaken to rule out this possibility. The biopsy of observed lesions may be useful to confirm the diagnosis by excluding other etiologies of similar appearance [3].
The treatment is initially based on supportive care with digestive tract rest and PPIs [2]. Therapeutic management consists in correcting anemia by blood transfusion with resuscitation measures for hypoperfusion and relieving the pain. Enteral nutrition should be avoided. Parenteral nutrition can be used until the resumption of oral feeding [9].
The use of high-dose IPPs within the initial phase and even after remission is recommended to reduce the risk of late complications. The use of antibiotics is not systematic and should be handled with caution, as publications have reported the potential for AEN development after using some antibiotics such as Clindamycin [10]. Antifungal and antiviral drugs can also be used, according to the indications. The placement of a nasogastric tube on an injured mucosa must be avoided because of the risk of perforation.
The uncomplicated AEN evolves in two phases. The initial phase is characterized by the blackish appearance of the distal esophageal mucosa. In contrast, the second phase is the healing stage, and it is characterized by friable pink mucosa surmounted by necrotic pseudomembranes with some residual black spots [1]. The esophagus usually regains its normal endoscopic appearance approximately 7 days to 14 days later. The delay of complete remission varies according to the patient’s overall condition [3].
Perforation is the most lethal complication of necrotizing esophagitis and, luckily, is extremely rare. It is required surgical treatment [11]. Stenosis formation is also observed in the chronic stage of the disease in some patients.
AEN mortality rate is about 32% [12]; this high rate is probably due to severe underlying diseases. So the estimated specific mortality of AEN is approximately 6% [7].
Conclusion
AEN is an unusual cause of upper gastrointestinal bleeding and can be life-threatening. It concerns mostly elderly patients with multiple comorbidities such as diabetes, hypertension, and chronic kidney insufficiency. The treatment is based on the management of the underlying condition associated with high-dose proton pump inhibitors and supportive care.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Acute esophageal necrosis; Upper gastrointestinal bleeding; Management; Outcome; Case report
Cite this article
Merzouk S, Bouhamou F, Salihoun M, Acharki M, Kabbaj N. Acute esophageal necrosis: A rare and serious cause of digestive bleeding. Clin Case Rep J. 2023;4(3):1–3.
Copyright
© 2023 Soumaya Merzouk. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).