Massive Bilateral Infrapatellar Bursitis: A Rare Manifestation
* Tyler Madden;
* Matt Pate;
Doug Rossi;
Drew Albert;
Sebastian Paz Kitschke;
Karl Roberts;
-
* Tyler Madden: Department of Orthopedics & Rheumatology, Spectrum Health – Michigan State University, Grand Rapids, MI 49503, United States.
-
* Matt Pate: Department of Orthopedics & Rheumatology, Spectrum Health – Michigan State University, Grand Rapids, MI 49503, United States.
-
Doug Rossi: Department of Orthopedics & Rheumatology, Spectrum Health – Michigan State University, Grand Rapids, MI 49503, United States.
-
Drew Albert: Department of Orthopedics & Rheumatology, Spectrum Health – Michigan State University, Grand Rapids, MI 49503, United States.
-
Sebastian Paz Kitschke: Department of Medicine, Michigan State University College of Human Medicine, Grand Rapids, MI 49503, United States.
-
Karl Roberts: Department of Orthopedics & Rheumatology, Spectrum Health – Michigan State University, Grand Rapids, MI 49503, United States.
Abstract
Background: Bursitis is inflammation and/or swelling of the synovial-lined sac-like structure around joints. A typical presentation would include pain, swelling, and warmth to the bursae, which typically resolves with conservative measures. However, rarely chronic bursitis can mimic more serious conditions, such as synovial sarcomas. This particular case highlights the broad spectrum of how bursitis may present, the importance of distinguishing severe cases of bursitis from sarcomas, as well as surgical treatment as an option for refractory cases.
Case Presentation: We present a rare manifestation of chronic bursitis in a 49-year-old male due to chronic work-related trauma. Nonoperative options, including aspirations, have failed in this patient, and he was eventually treated with bilateral open bursectomy, essentially curing him of his bursitis.
Conclusion: Chronic bursitis, if left untreated, may progress to a massive state, causing significant impairment in quality of life and daily function.
Introduction
Bursitis is inflammation and swelling of the synovial-lined sac-like structure, which does not communicate with the knee joint. Bursae function to reduce friction between structures, as in the case of the infrapatellar bursa, which minimizes trauma to the patellar tendon that may occur during jumping or kneeling [1]. The four major bursae surrounding the knee joint include the prepatellar, suprapatellar, infrapatellar, and pes anserine bursa. Prepatellar and infrapatellar bursitis, in particular, are usually related to acute trauma, overuse, or abnormal biomechanics of the knee, which may be observed in individuals who engage in frequent kneeling or in patients with cerebral palsy [2]. It is a clinical diagnosis based on physical exam findings, which may include pain, swelling, and warmth of the bursa. It may also be present in the context of crystal disease, infection, or other systemic forms of arthritis. Bursa with chronic inflammation may have calcifications or become a solid mass with minimal fluid content [1,3]. The majority of patients will experience resolution of their bursitis with NSAID use and avoidance of inciting events, such as kneeling. However, symptoms may not resolve and may progress over several years, particularly if the occupation poses a continual risk of progression. This will be demonstrated in our case report of massive, chronic bilateral infrapatellar bursitis.
Case Presentation
We describe a 49-year-old male with a past medical history of obesity and hypertension who presented to a Midwest Hospital-Based Orthopedic Clinic in the United States complaining of bilateral infrapatellar fluid-filled masses for 12 years. These masses were mildly painful with kneeling but were otherwise nonpainful. He had been evaluated at an outside orthopedic office and had both knees aspirated several times, only to have the masses return after several days. It is unknown if this fluid underwent further analysis as this was done outside our hospital system. Previous radiographs did not show any obvious bony abnormality concerning malignancy. The patient previously had a surgical discussion with an orthopedic surgeon outside of our institution; however, due to work scheduling conflicts during the COVID pandemic, he could not schedule his surgery.
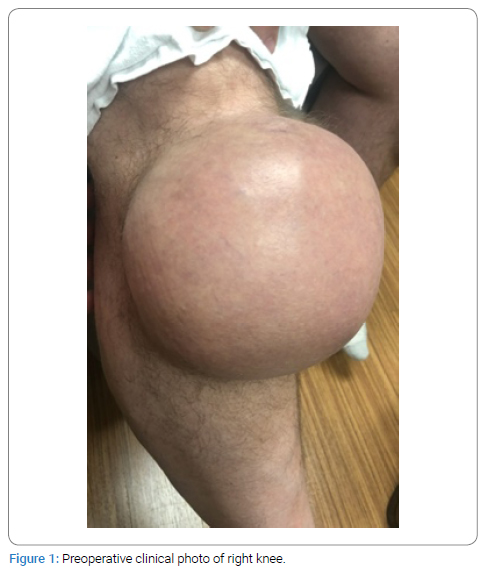
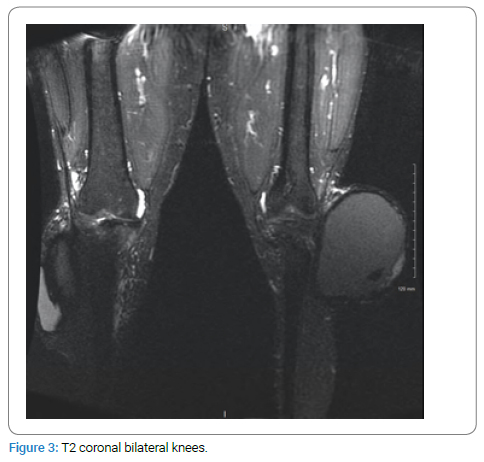
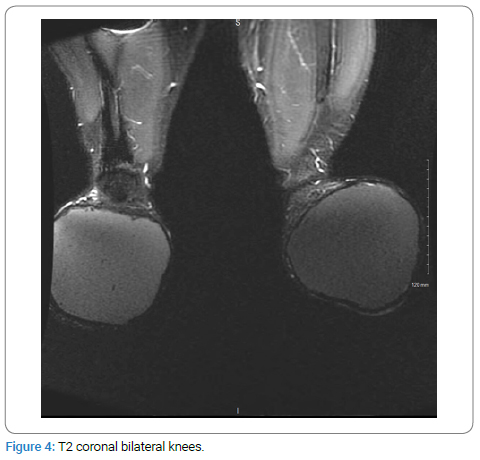
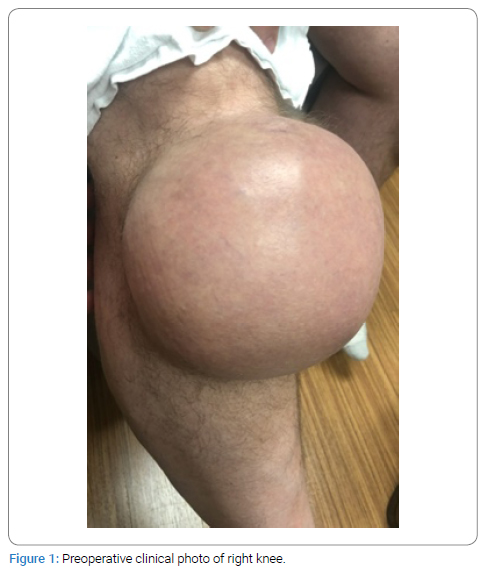
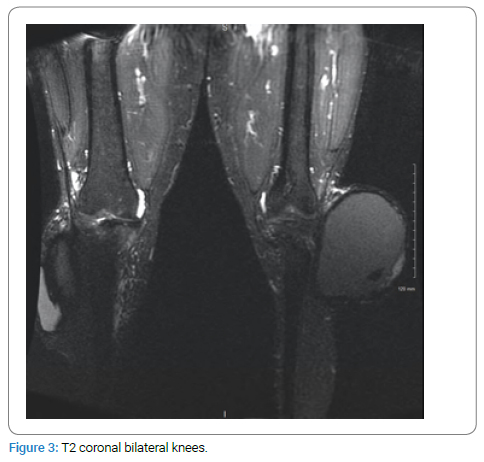
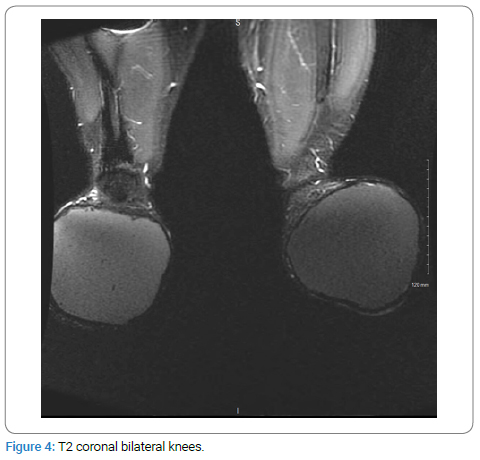
On physical examination, the patient demonstrated massive bilateral infrapatellar masses (Figure 1,Figure 2). Both were compressible, non-tender to palpation, and without erythema. The overlying skin was intact, and there was no active drainage. Active and passive knee extension and flexion were intact and nonpainful from 0 to 90 degrees. MRIs had been obtained three years prior (Figure 3,Figure 4) and demonstrated massively distended infrapatellar bursae with a homogeneous appearance. There were no signs of osteomyelitis or occult fracture. Given this homogenous appearance with no solid enhancing component and the presence of bilateral masses identical in appearance, it was felt to be more consistent with chronic infrapatellar bursitis and less concerning for an oncologic process.

Furthermore, the patient’s presentation did not appear to be consistent with an infectious etiology such as septic arthritis, given the lack of erythema, no pain with range of motion or weight bearing, and no tenderness on palpation. For this reason, an infectious workup including WBC, CRP, and ESR differed. We discussed these findings with our hospital’s orthopedic oncologist, who shared a low suspicion of an oncologic process.
After a discussion of the risks and benefits of treatment options with the patient, it was decided to proceed with an open bursectomy.
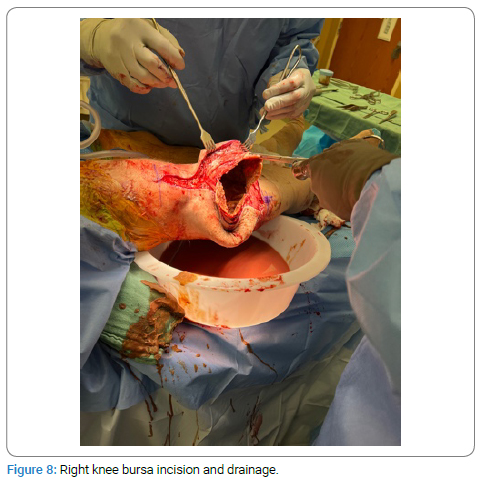
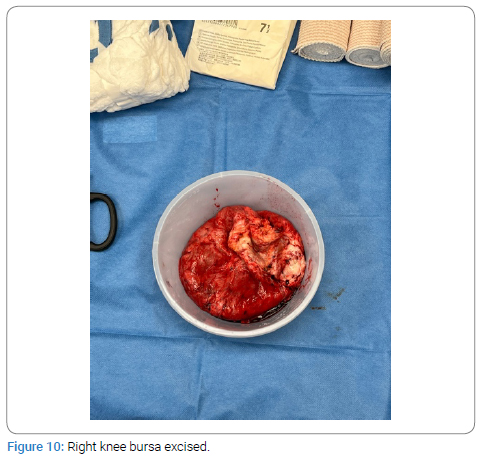
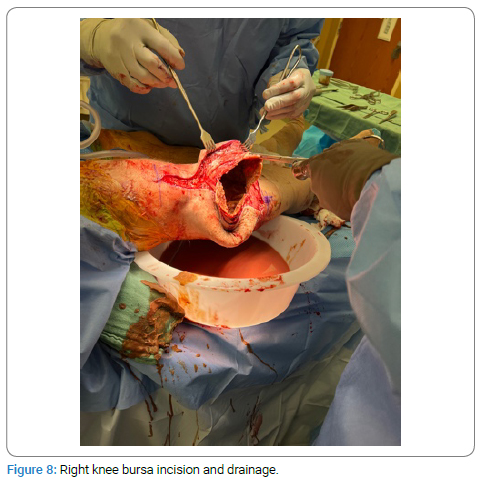
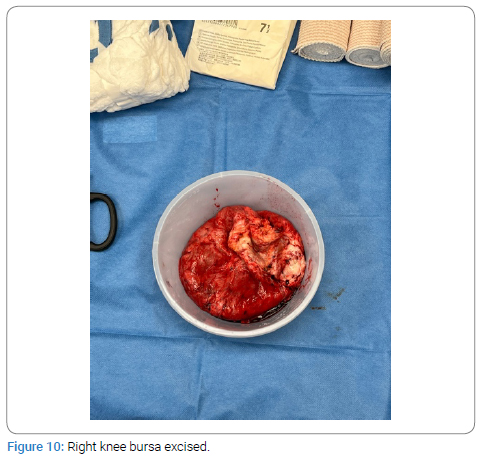
Surgical Technique: The patient was positioned supine on the operating table. General anesthesia was administered. Bilateral tourniquets were placed at the upper thigh. A midline incision was first made over the right knee, starting from the superior pole of the patella to 2 cm distal to the bursal swelling (Figure 5,Figure 6). The entire bursal sac was enucleated, preserving full-thickness skin circumferentially. Careful dissection was performed, and no evidence of deep communication of the bursal sac or fluid into the knee joint or deep tissues was found. The anterior compartment fascia, patellar tendon, and joint capsule were all noted to be intact and uninvolved. The bursa was incised, copious amounts of brown turbid fluid were expressed, and a large volume was collected and sent for fluid analysis and culture (Figure 7,Figure 8). Using sharp dissection, the bursal sac was also excised and sent for pathologic analysis (Figure 9,Figure 10). The excised bursa was measured at 14 cm x 14 cm. The remaining wound was irrigated with pulse lavage. Attention was turned to the left knee, and an identical approach was utilized (Figure 11). The left bursa sac was measured at 15 cm x 18 cm (Figure 12,Figure 13). After the bursal excision, a large amount of redundant, full-thickness-viable appearing skin was noted on both sides of the incision. Excess skin was excised, and the wound was closed in a layered fashion using a combination of interrupted 2-0 vicryl and running 3-0 nylon baseball stitch (Figure 14).








30 cc of 0.5% bupivacaine was injected around each surgical wound respectively for a total of 60 cc. Sterile compressive dressings were applied to each lower extremity. The patient tolerated the procedure well, and no complications were encountered. The total operating time was 246 minutes.
Postoperative Course: Tissue biopsies of the left and right knee bursa showed fibrous tissue with hemosiderin deposition, granulation tissue, and cholesterol clefting, consistent with chronic bursitis. The medical cytology report demonstrated acellular amorphous material bilaterally without evidence of malignancy. Staphylococcus Epidermidis with WBCs were found on the body fluid culture. Fungal, AFB and Anaerobic cultures were negative for organisms.
At the patient’s two-week postoperative visit, he had been maintaining compressive wraps diligently and denied significant discomfort. A small fluid collection over his left knee had been reaccumulating distal the incision, which was thought to be a small postoperative hematoma or seroma rather than a recurrence. There was no erythema or tenderness to this knee. The right knee was also without recurrence. Both incisions were well healed bilaterally without evidence of wound dehiscence. A decision was made with the patient to aspirate the small mass on the left knee. Approximately 180 cc of serosanguinous fluid was aspirated, with no purulence noted. No other complications were noted at that time, and there have been no further fluid accumulations to date. At the three-month follow-up, the seroma had disappeared (Figures 15a and 15b). He reported minimal pain and returned to work as a butcher full-time. The right knee was also well-healed with no evidence of recurrence (Figures 16a and 16b). He was able to bear weight on the knee and maintain knee flexion and extension from 0 to 90 degrees.


Discussion
There have been few cases of chronic infrapatellar bursitis reported in the literature. McCarthy et al. described a patient with bilateral infrapatellar bursitis with heavy calcifications and suggested that it was due to repeated episodes of hemorrhagic events to the infrapatellar bursa [1]. Consistent with the current literature and our clinical case, repeated traumatic hemorrhagic events appear to pose a risk factor for chronic bursitis. While there have been discussions regarding unilateral massive prepatellar bursitis, to our knowledge, this is the first case report in the literature demonstrating massive bilateral infrapatellar bursitis of this magnitude.
The presence of bursitis in the workforce has been previously reported as relatively low. Le Manac’h et al. investigated 3710 French workers between 2002 and 2005 and demonstrated a prevalence of uni or bilateral bursitis as 0.6% [0.2–0.9] in men and 0.2% [0.0–0.6] in women, with the highest prevalence observed in the construction sector and the food and meat processing industry. In light of this study, our patient was at higher risk for developing bursitis, given his male sex and occupation as a meat processor [4].
Early recognition and diagnosis of a mass around the knee is essential, as many bony and soft tissue tumors may present in a similar manner, and early diagnosis is pivotal in optimizing prognosis. In addition, two cases of calcific hemorrhagic bursitis have been reported in the literature with dystrophic calcifications within the lesion mimicking a synovial sarcoma, again highlighting the importance of including soft tissue sarcomas in the differential [5]. Schubert also uncovered a case of femoral osteochondroma presenting as bursitis and ischiofemoral impingement [6]. In light of possible similar presentations, a multidisciplinary approach may be beneficial to confirm the distinction between massive bursitis and a possible oncological cause, which we achieved in our case after a thorough discussion with the hospital’s orthopedic oncologist. Several clinical data points were utilized to make this determination. Firstly, MRIs noted no communication with the underlying bone or joint and showed a homogenous appearance within the infrapatellar bursae without a consolidated mass. Second, the fact that the masses were bilateral and without systemic symptoms such as weight loss and fatigue made a tumor diagnosis less likely.
The most common complications described in the literature with open bursectomy, particularly in the treatment of open olecranon bursectomies, include skin healing issues and recurrence [7–11]. These complications were reported as high as 27% and 22%, respectively, in a study by Degreef and Smet [10]. It was felt that our patient’s postoperative fluid collection was a seroma rather than a recurrence because the entire bursa was removed, making recurrence unlikely, and the seroma resolved on its own after aspiration. Unfortunately, current literature has found no difference in reducing postoperative seromas with compressive dressings and immobilization. Effective strategies which may help our patients include closed-suction drains, sharp or ultrasonic dissection during surgery rather than cautery, and other techniques [12,13].
Quayle and Robinson also reported neuropraxia to the infrapatellar branch of the saphenous nerve [9]. These complications have been mitigated in multiple other studies through the use of an endoscopic approach [7,8,11]. While endoscopic and open management for the treatment of prepatellar bursitis has both been described in the literature with similar outcomes of recurrence and slightly lower wound complications in the endoscopic cohorts [7–8], this has not been discussed in the setting of massive bursitis. Though considered, it was decided that the risk of inability to excise the entire bursa endoscopically in addition to the distorted anatomy from the size of the bursae with risk of damage to surrounding structures was high, and therefore, it would be more favorable to perform the open bursectomy.
Conclusion
Though a relatively benign process, bursitis can progress to become a limiting condition. Early diagnosis is important for guiding management and ensuring more worrisome conditions are excluded from the differential. With various nonoperative therapies, including activity modification, nonsteroidal anti-inflammatories, compression, and aspiration, the majority of cases of bursitis can be treated without surgery. However, if untreated or with failed nonoperative management, a bursectomy can be utilized through an endoscopic or open approach. This case highlights the need for early diagnosis and treatment to prevent progression to a massive state, requiring prolonged surgery.
Declarations
Ethics approval and consent to participate: N/A.
Consent for publication: Patient consent was obtained over the telephone to write and publish this manuscript.
All data generated or analysed during this study are included in this published article.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- McCarthy EM, Murphy C-L, Doran MF, Cunnane G. Infrapatellar bursitis: an occupational legacy. J Clin Rheumatol. 2011;17(1):49–50.
- Siegel HJ, Lopez-Ben R, Pitt MJ, Dunham WK. Massive prepatellar bursitis in cerebral palsy. J Surg Orthop Adv. 2007;16(1):23–26.
- Arora S, Batra S, Rao S, Maini L, Gautam VK. “A 40-year-old female with painless, slow growing prepatellar mass”. J Clin Orthop Trauma. 2014;5(4):274–279.
- Le Manac’h AP, Ha C, Descatha A, Imbernon E, Roquelaure Y. Prevalence of knee bursitis in the workforce. Occup Med (Lond). 2012;62:658–660.
- Stahnke M, Mangham DC, Davies AM. Calcific haemorrhagic bursitis anterior to the knee mimicking a soft tissue sarcoma: report of two cases. Skeletal Radiol. 2004;33(6):363–366.
- Schubert T, Navez M, Galant C, Docquier PL, Acid S, Lecouvet FE. Femoral osteochondroma responsible for ischiofemoral impingement, bursitis, and secondary lipoma arborescens mimicking malignant transformation. Acta Radiol Open. 2019;8(12):2058460119892409.
- Meric G, Sargin S, Atik A, Budeyri A, Ulusal AE. Endoscopic versus open bursectomy for prepatellar and olecranon bursitis. Cureus. 2018;10(3):e2374.
- Kerr DR, Carpenter CW. Arthroscopic resection of olecranon and prepatellar bursae. Arthroscopy. 1990;6(2):86–88.
- Quayle JB, Robinson MP. An operation for chronic prepatellar bursitis. J Bone Joint Surg Br. 1976;58-B(4):504–506.
- Degreef I, De Smet L. Complications following resection of the olecranon bursa. Acta Orthop Belg. 2006;72(4):400–403.
- Ogilvie-Harris DJ, Gilbart M. Endoscopic bursal resection: the olecranon bursa and prepatellar bursa. Arthroscopy. 2000;16(3):249–253.
- Papanikolaou A, Minger E, Pais MA, Constantinescu M, Olariu R, Grobbelaar A, et al. Management of postoperative seroma: recommendations based on a 12-year retrospective study. J Clin Med. 2022;11(17):5062.
- Janis JE, Khansa L, Khansa I. Strategies for postoperative seroma prevention: a systematic review. Plast Reconstr Surg. 2016;138(1):240–252.
Keywords
Infrapatellar bursitis; Chronic bursitis; Sarcoma; Refractory
Cite this article
Madden T, Pate M, Rossi D, Albert D, Kitschke SP, Roberts K. Massive bilateral infrapatellar bursitis: a rare manifestation. Clin Case Rep J. 2023;4(3):1–7.
Copyright
© 2023 Adam Bowen. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).