Abstract
Dide-Botcazo syndrome is an extreme neurological emergency. It is distinguished by bilateral cortical blindness and memory disturbances with anosognosia, which remains a subject of debate if it should be included in the definition. Ischemic stroke of the posterior regions is the main etiology, hence the severity of the visual prognosis in the absence of rapid treatment in the acute phase. We report the case of a patient who has developed the syndrome with bi-occipital ischemia who consulted late because of anosognosia. The diagnosis was confirmed by neuroimaging. As the patient was not eligible for reperfusion treatments by intravenous thrombolysis and/or mechanical thrombectomy, the management of the disease was non-specific and symptomatic, with an evolution that was marked by bilateral cortical blindness and regression of the other symptoms.
Introduction
The syndrome of Dide-Botcazo is a rare clinical syndrome proposed by Dide and Botcazo in 1902. characterized by cortical blindness, amnesia, and topographical disorientation, it is observed mainly in bilateral occipital ischemic strokes [1,2]. It is a diagnostic and therapeutic emergency that may be eligible for intravenous thrombolysis or mechanical thrombectomy for patients who come within the conventional time limit. We report a case.
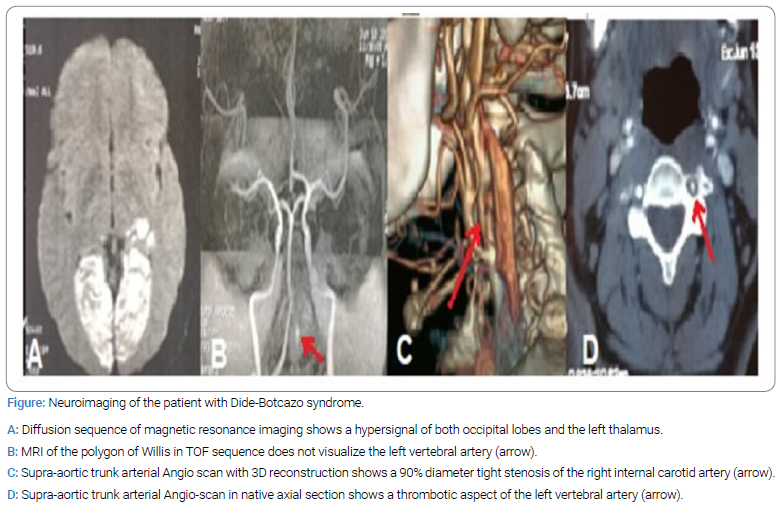
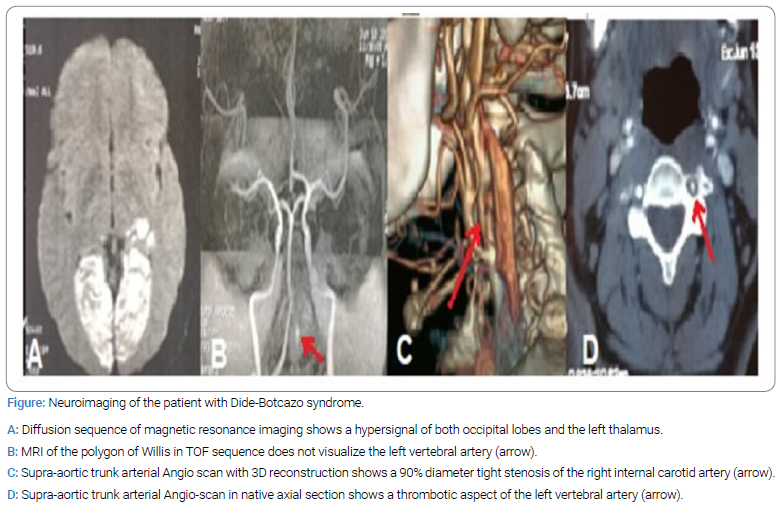
Observation: A 54-year-old woman with a history of inadequately controlled insulin-resistant diabetes mellitus consulted for symptoms evolving for 24 hours, consisting of a sudden bilateral and severe visual acuity loss and forgetfulness with non-recognition of these disorders. At admission to a stroke unit, the patient had a satisfactory hemodynamic condition, a capillary glycemia of 2.5 g/l, and a body mass index of 27 kg/m2. The neurological examination showed a global bilateral visual field amputation with a normal pupillary reflex with negative menace response, an anosognosia (lack of awareness of the deficit), a retrograde amnesia with confabulations, which were a cause of non-recognition of blindness and, therefore a delay in consulting. The initial ophthalmologic evaluation found a visual acuity of 0/10 and a bilateral cataract that interfered with the examination of the ocular fundus. The CT scan and MRI scan of the brain showed a bilateral occipital acute ischemic stroke with cerebellar and left thalamic ischemic areas; MRI and CT, angiography of the supra-aortic arteries showed the absence of arterial flow in the two occipital arteries and the left vertebral artery, which are correlated with ischemic lesions, as well as a large atherosclerotic plaque of the right internal carotid artery, decreasing its diameter by 90% (Figure). The blood lipid profile showed hypercholesterolemia (LDL= 2.20 g/l), and the remaining etiological work-up, particularly cardiological, including electrocardiogram, transthoracic cardiac ultrasound, and Holter-ECG, were negative. The stroke was attributed to atherosclerosis. The management of the disease consisted of non-specific care, including glycemic control, preservation of good cerebral perfusion (average blood pressure at 160/90 mmHg and oxygen saturation greater than 94%), and removal of aggravating factors, as well as secondary prevention based on anti-platelet aggregation (aspirin 100 mg) and high dose of statins (Atorvastatin 80 mg). The evolution was marked by sequelae cortical blindness with preservation of very reduced tubular central vision, which was demonstrated on the follow-up ophthalmological evaluation. Otherwise, there was a total remission around the seventh day of hospitalization of memory disorders as well as confabulations and anosognosia. The latter was a limitation for the administration of neuropsychological tests at admission.
Discussion
Blindness of sudden and/or rapid onset is an extreme neuro-ophthalmologic emergency. This includes central blindness, which must be readily identified based on specific clinical features. The occipital lobe is the final visual pathway, and its lesion, especially bilateral, produces bilateral blindness in the primary state. The clinical features of Dide-Botcazo syndrome result from the disruption of the associative fascicles connecting visual areas to memory centers and the thalamus that controls topographic orientation. When associated with other symptoms of Dide-Bocatzo syndrome, it may be ignored or neglected by the patient’s entourage because the patient himself or herself does not recognize his visual deficit. This syndrome must be suspected as a priority in the presence of memory disorders, particularly anterograde, as well as anosognosia of central blindness. However, the differential diagnosis with Anton Babinski syndrome must be discussed, given the similarity of certain signs that remain unilateral and without memory disorders [3]. The most frequent etiology is ischemic stroke, for which the underlying lesion mechanism is mainly an embolic one, obstructing the top of the basilar artery or both posterior cerebral arteries, which are responsible for the vascularization of the visual cerebral areas [4,5]. The occurrence of atherosclerotic origin remains uncommon, and in 25% of cases, the stroke remains cryptogenic [6]. Management of such an emergency is typically done in a neurovascular unit by offering recanalization treatment - if eligible - by intravenous thrombolysis and/or mechanical thrombectomy in addition to non-specific measures. To our knowledge, we have not found any cases of IV thrombolysis in the literature, probably because of the delayed consultation due to misleading symptoms. Dide-Botcazo syndrome is not restricted to stroke, as other conditions such as trauma to the occipital area, migraine with a visual aura, and occipital neoplasms have been reported [7]. The neuro-psychosocial prognosis is often poor, as in our patient’s case, where she lost her sight due to late diagnosis and limited therapeutic possibilities [8].
Conclusion
Acute central visual disturbances are a diagnostic and therapeutic emergency that may benefit from fibrinolytic and endo-vascular therapies and must be promptly identified by the clinical practitioner, especially in neurological and ophthalmological emergencies, since the outcome can be modified. Sometimes, visual disturbances can be accompanied by amnesia and anosognosia, constituting Dide-Botcazo syndrome.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Dide-botcazo; Blindness; Ischemic stroke
Cite this article
Haddouali K, Sikkal A, Bellakhdar S, Otmani H, Rafai MA, El Moutawakil B. Dide-botcazo syndrome: a non-ophthalmologic blindness. Clin Case Rep J. 2023;4(4):1–3.
Copyright
© 2023 Kamal Haddouali. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).