Single Nerve Transfer in Case of Partial Pre-Ganglionic Injury C5 and Avulsion Injury C6
Mancho Kovachev;
* Vihar Kovachev;
Emil Simeonov;
Hristo Gigov;
B Sadursanska;
-
Mancho Kovachev: Clinic of Orthopaedics and Traumatology; UMBAL, Medical University, Pleven, Bulgaria.
-
* Vihar Kovachev: Clinic of Orthopaedics and Traumatology; UMBAL, Medical University, Pleven, Bulgaria.
-
Emil Simeonov: Clinic of Orthopaedics and Traumatology; UMBAL, Medical University, Pleven, Bulgaria.
-
Hristo Gigov: Clinic of Orthopaedics and Traumatology; UMBAL, Medical University, Pleven, Bulgaria.
-
B Sadursanska: Clinic of Orthopaedics and Traumatology; UMBAL, Medical University, Pleven, Bulgaria.
Abstract
Introduction: Loss of active abduction and external rotation of the shoulder, as well as flexion of the elbow, at high lesions C5 C6 present challenges in orthopedic surgery.
Aim: The study aimed to estimate the possibility of recovery of the shoulder girdle and elbow function through a single intrapleural nerve transfer in stated lesions.
Materials and methods: We present a case of a patient with a partial high lesion of C5 and avulsion C6, who was treated through single nerve transfer from the radial nerve and median nerve to the musculocutaneous and axillary nerve.
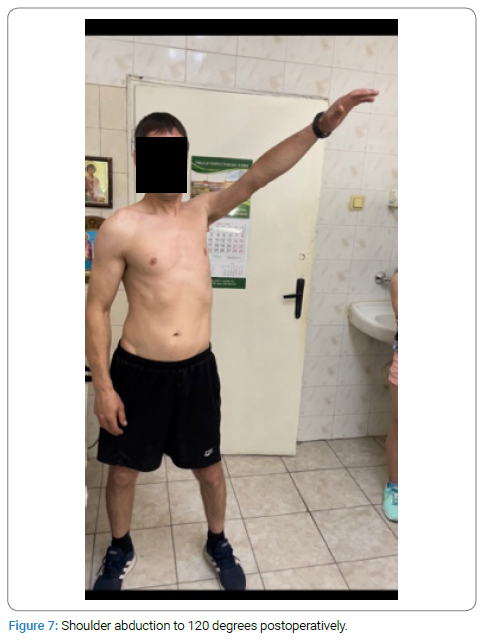
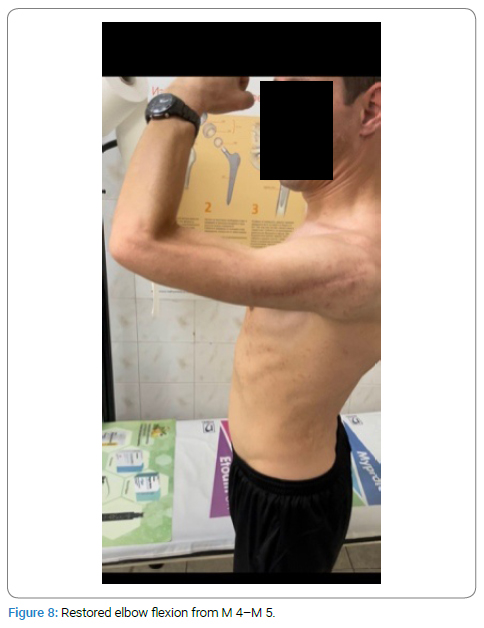
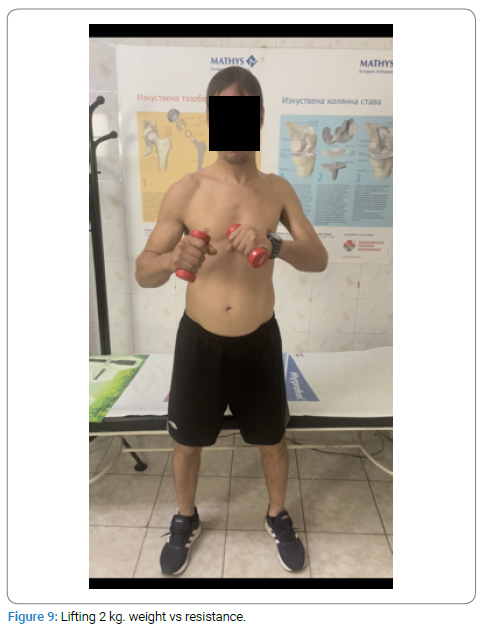
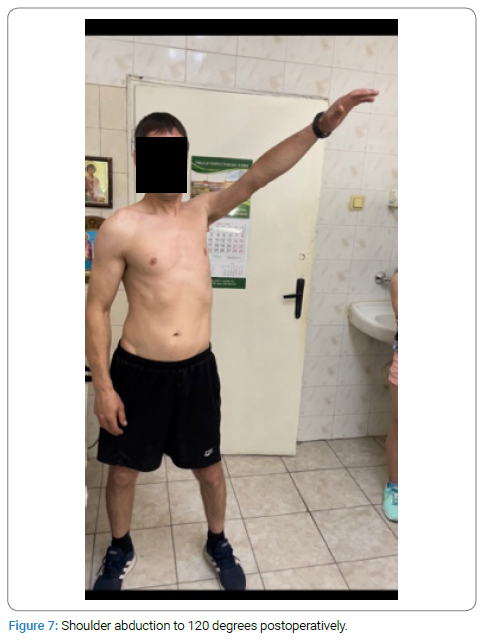
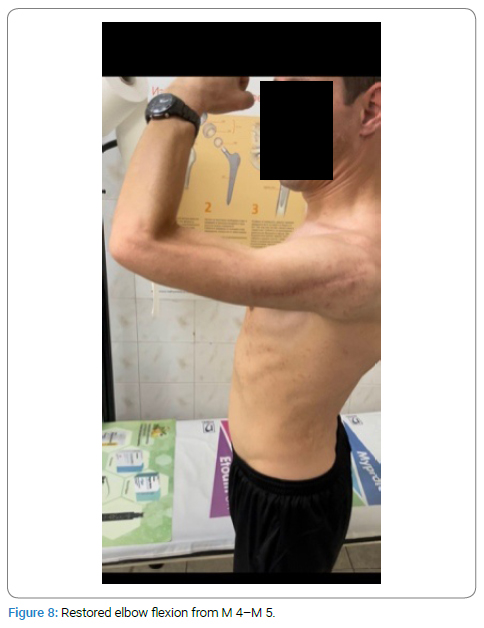
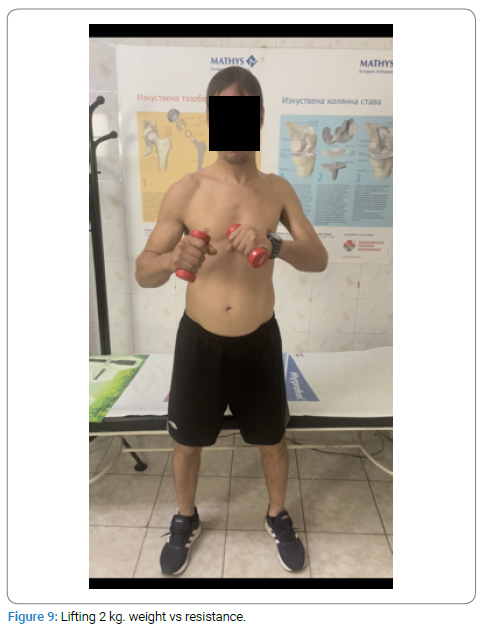
Results: A significant improvement in active shoulder abduction of 120 degrees was achieved by the patient, as well as actively resisted flexion in the elbow (M4, M5, able to move 2 kg against gravitation and resistance).
Paraesthesia in the region of the radial nerve disappeared after three months. After three months, a positive monofilament test of Weinstein and normal flexion of the wrist were observed. The active function of the triceps brachii was not changed. Results were reported 6-, 8-, 12- and 18 months post-operation.
Conclusion: Single nerve transfers are acceptable in case of partial preganglionic C5 lesion and C6 avulsion injury in case of a preserved function of C7-Тh1.
Introduction
Treating Peripheral Nerve Lesions (PNL) presents a constant problem for neurosurgeons, orthopedics, and microsurgeons. It is a still small number of successful outcomes that define the actuality of a problem, which could lead to severe disability, which could be compared to the loss of a limb. Ultimately, it leads to social and psychological problems and resocialization.
Surgical reconstruction of the nerve, nerve transfers, nerve augmentation as well as tendon transfer, and free muscular graft transfer became the choice of treatment instead of conservative treatment. In our opinion, as well as the number of modern authors [1–3], results from nerve transfer are much better compared to neurorrhaphy and nerve graft.
In problematic cases (preganglionic / L1), denervation of longer than six months, nerve transfer has a number of advantages. Decreased distance and quicker nerve regeneration are some of them. According to us, as well as other authors [1–3], intrapleural transfers have advantages over extraplexial transfers.
Aim
Evaluate possible options for restoring shoulder and elbow functions through single intrapleural nerve transfer in stated lesions.
Materials and Methods
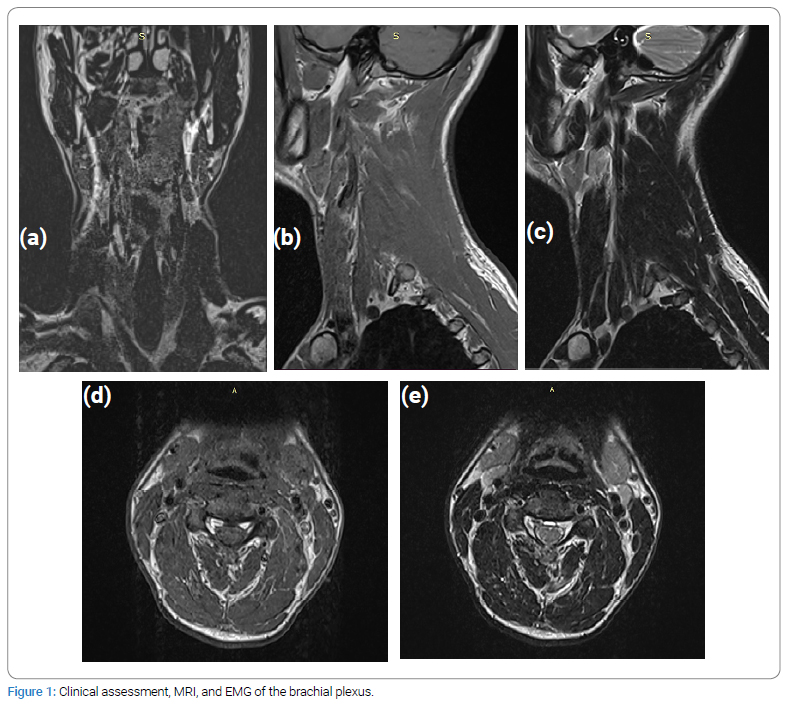
The patient, a 39-year-old male who suffered a motorcycle accident, presented to our medical team 5 months after the accident. In conclusion of, clinical assessment, MRI, and EMG, it was found that the patient has suffered a high lesion of the brachial plexus, with additional data indicating partial injury at C5 and a total lesion at C6 (Figure 1a,b,c,d,e).
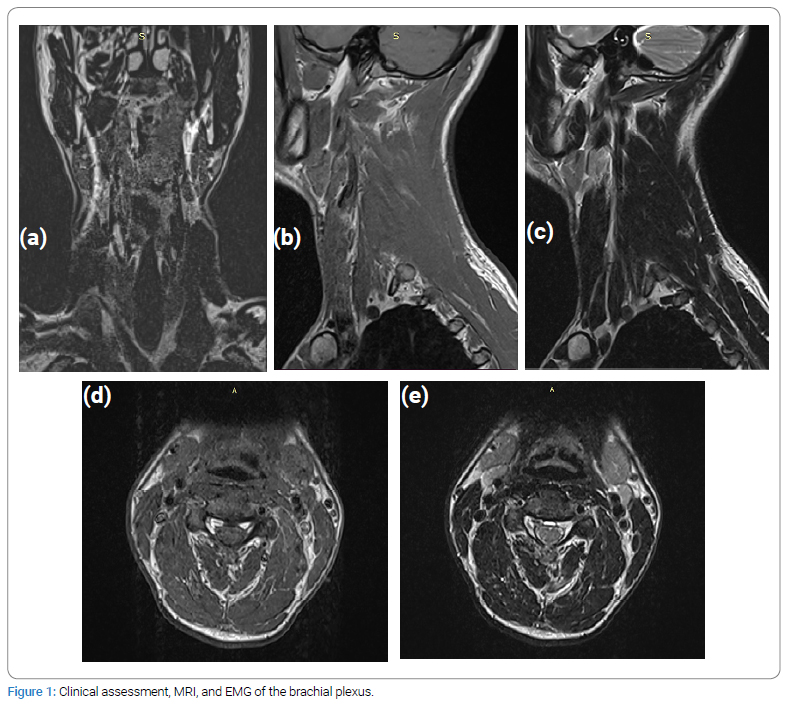
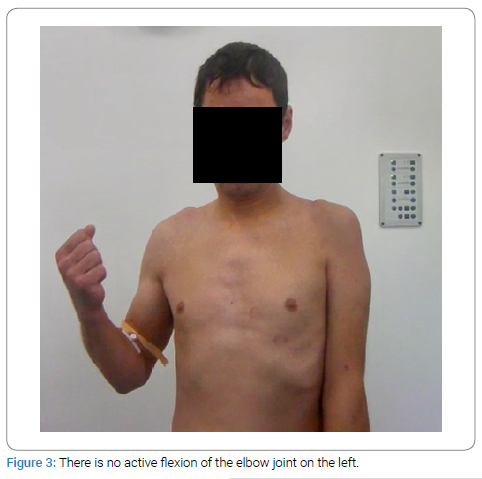
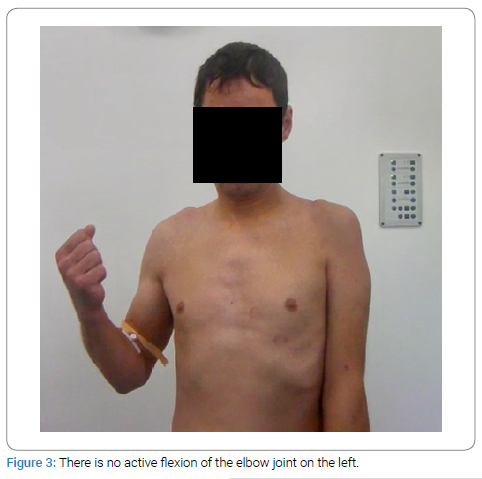
Thus, data from the needle EMG analysis and clinical examination has shown decreased shoulder AROM of 0-5 degrees (Figure 2) and decreased AROM of the elbow with strength M0 (Figure 3). We thus accepted that the patient had a partial injury at the level C5 and an avulsion injury at level of C6.

Electrodiagnostic study: All Electrodiagnostic Nerve Conduction Studies (NCS) and needle Electromyography (EMG) were done using Keypoint EMG equipment (Medtronic v. 5.09). The examinations were performed by the same experienced neurophysiologist, according to the guidelines and practice parameters recommended by the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) [4].
Baseline EMG /20.08.2020/
Electrodiagnostic findings: Motor response from the left suprascapular nerve present with abnormally low 0.5 mV amplitude. The left axillary nerve and musculocutaneous nerve are unobtainable, even with supramaximal stimulation. Sensory nerve conduction from the left lateral cutaneous nerve of the forearm is normal [13–15].
Needle EMG shows spontaneous activity: ++ fibrillations and Positive Sharp Waves (PSW) in the left biceps, deltoid, brachioradial muscle, and paraspinal C6; + fibrillations in the rhomboid muscle. No voluntary activity was recorded from the left biceps, brachioradial, extensor carpi radial, and deltoid muscles [16–18]. Only In the Supraspinal and rhomboid muscles is the presence of 2 Motor Unit Potentials (MUP) with increased discharge frequency.
EMG data for probable partial preganglionic lesion of left C5 root and severe for C6.
Evaluated muscular strength according to BMRC. The range of motion was measured with a goniometer.
The treatment was done according to the Oberlin 1 technique, as well as instead of fasciculi of the ulnar nerve, we took fasciculi from the median nerve, responsible for the flexion of the wrist (flexor carpi radialis) [19–21].
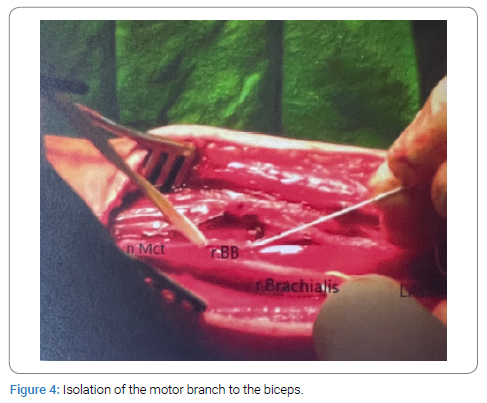
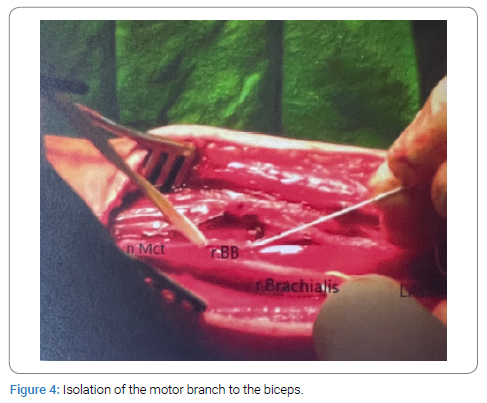
After isolating the motor branch to biceps brachii and after intraneural neurolysis and electrical stimulation, which has confirmed an unreversible lesion of the branch, it was separated from the main branch of the musculocutaneous nerve, around 1 cm from the point of entry to the muscle (Figure 4).
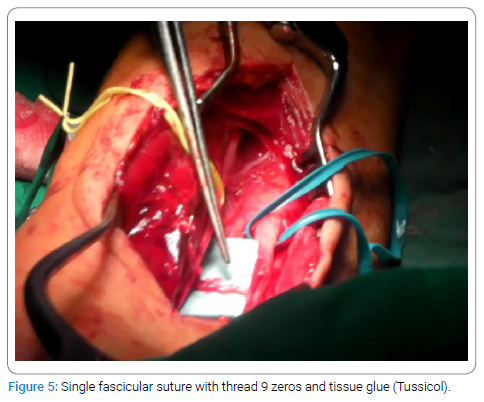
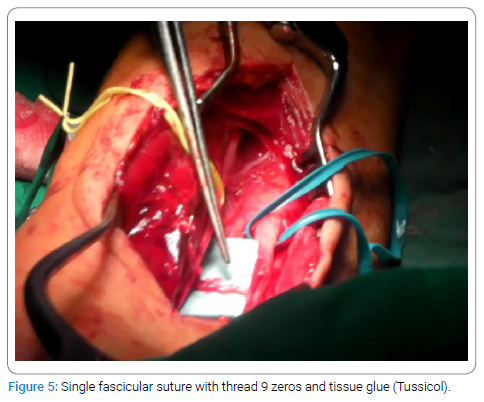
We prepared the opposite part of the medial nerve and medial fasciculi, which is responsible for flexor carpi radialis, which was confirmed by electrical stimulation [22–24]. The same one was isolated and cut distally; afterward, it was turned to recipient fasciculi. Afterward, a single fascicular suture with thread nine zeros was applied and reinforced with fibrin sealant (Tussicol) (Figure 5).
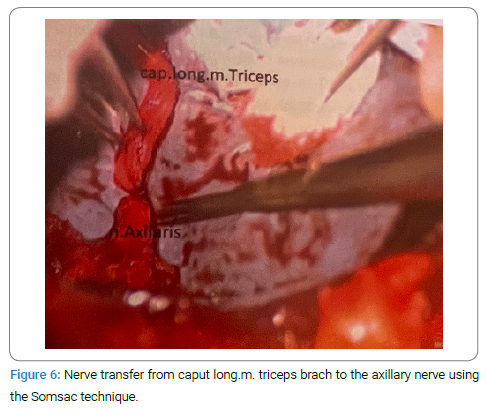
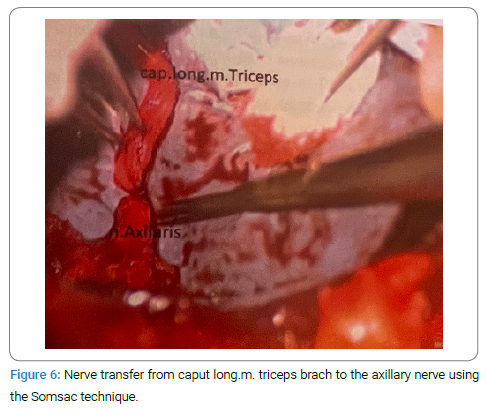
The limb was immobilized for three weeks before early mobilization of the elbow and shoulder joints would begin. One month later, nerve transfer from the long head of the triceps brachii to the axillary nerve was done according to the Somsac technique. After the isolation of the anterior branch of the axillary nerve, it was found and isolated in the most proximal quadrangular space and dissected. The radial nerve is located in the trilateral space and is identified as a branch of the nerve to the long head of the biceps brachii muscle. At the most distal point, it was dissected and turned to the anterior branch of the axillary nerve (Figure 6). A single fascicular suture with thread nine zeros was applied and reinforced with fibrin sealant (Tussicol). A trial of tension of the suture was done by moving adjacent joints. On the 14th day, early pendulum movements began.
Results
The patient has achieved significant improvement in shoulder abduction up to 120 degrees (Figure 7) as well as flexion of the elbow (M4–M5) (Figure 8), with the ability to move 2 kg against gravity (Figure 9).
Paraesthesia, which was found in the region supplied by the radial nerve in the first three months, was later resolved spontaneously. The monofilament test of Weinstein was read positively after 3rd month, and normal wrist flexion was found. The active function of the triceps brachii was not changed.
Regardless of restored function, we observed muscular atrophy, which provoked observable asymmetry of the limbs. The patient returned to work 12th month after surgery. Results were recorded by means of goniometry and dynamometry of the donor’s nerves on the 6th, 8th, 12th, and 18th months post-operatively.
EMG 3 months after surgery January 26, 2021.
Normal CMAP of the suprascapular nerve. The appearance of a motor response from the axillary and musculocutaneous nerve with low amplitude 1.9 mv and 1.1 mv.
Needle EMG- no spontaneous activity from deltoid and biceps muscle. Voluntary activity with three motor units was recorded in the left biceps muscle. 3 MUPs in the anterior part of the deltoid muscle and 4 in the posterior part.
EMG 9 months after surgery September 07, 2001 /1 years/ from trauma later.
Neurography showed significantly increased amplitudes of motor responses from the left axillary 8.1 mV and musculocutaneous nerve 3.1 mV.
Needle EMG - no denervation potentials. Reinnervation potentials are recognized as synchronized MUPs of increased amplitude in the left deltoid and biceps muscle.
Discussion
We have adopted the established method of double intrapleural transfers, restoring abduction and external rotation of the shoulder, as well as flexion of the elbow /17/.
We consider that in partial preganglionic lesions at C5 / preserved suprascapular nerve and intact rotator cuff /, application of single nerve transfer recovers full function of the shoulder joint, the same way as the single nerve transfer from medial nerve recovers full function – M4 – M5.
The patient has achieved abduction above 120 degrees and external rotation of 5 degrees, as well as flexion of the elbow against pressure – M4 – M5 fully fulfill requirements.
Meta-analysis of Garg, Merell GA [5,6] as well as publications of Oberlin, Nath, Leechavengvongs [2,7,8,9], Quantini [4,10] proved the advantages of nerve transfers in such lesions, Garg R.Merrell GA, Nath RK, Sungpet A [5,11,12].
Bad results after nerve graft and suture are usually owned due to slow growth speed and inevitable death of motor axons, distance, and denervation time [25].
Nerve transfer removes factors of distance and time, and the transfer of motor-to-motor branch escapes the neural mish-mash.
We consider that the advantages of the method are:
- Decrease of operative time. Two interventions could be performed during single-day surgery.
- Easier dissection of the medial nerve due to the fact that it lies closer to the motor branch of biceps brachii muscle /mbb/ and the length of donor fasciculi is smaller /24/.
- Drops need exploration of the brachial plexus, which is connected to a wide range of possible complications.
- Drops need of the second incision for acquiring the nerve graft.
- The operative technique is easier to execute.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Mackinnon SE, Novak CB. Nerve transfers. New options for reconstruction following nerve injury. Hand Clin. 1999;15(4):643–666.
- Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: anatomical study and report of four cases. J Hand Surg (Am). 1994;19(2):232–237.
- Terzis JK, Papakonstantinou KC. The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg. 2000;106:1097–1122.
- Al-Qattan MM, Al-Kharfy TM. Median nerve to biceps nerve transfer to restore elbow flexion in obstetric brachial plexus palsy. Biomed Res Int. 2014;2014:854084.
- Garg R, Merrell GA, Hillstrom HJ , Wolfe SW. Comparison of nerve transfers and nerve grafting for traumatic upper plexus palsy: A systematic review and analysis. J Bone Joint Surg Am. 2011;93(9):819–829.
- Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am. 2001;26(2):303–314.
- Rasulic L, Samardzic M, Grujicic D, Bascarevic V. [Nerve transfer in brachial plexus injuries--comparative analysis of surgical procedures]. Acta Chir Iugosl. 2003;50(1):33–46.
- Wehbe J, Maalouf G, Habanbo J, Chidiac RM, Braun E, Merle M. Surgical treatment of traumatic lesions of the axillary nerve. A retrospective study of 33 cases. Acta Orthop Belg. 2004;70(1):11–18.
- Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P, Ketmalasiri W. Nerve transfer to biceps muscle using a part of the ulnar nerve in brachial plexus injury (upper arm type): a report of 32 cases. J Hand Surg. 1998;23(4):711–716.
- Al-Qattan MM. Oberlin’s ulnar nerve transfer to the biceps nerve in Erb’s birth palsy. Plast Reconstr Surg. 2002;109(1):405–407.
- Sungpet A, Suphachatwong C, Kawinwonggowit V. One-fascicle median nerve transfer to biceps muscle in C5 and C6 root avulsions of brachial plexus injury. Microsurgery. 2003;23(1):10–13.
- Nath RK, Lyons AB, Bietz G. Physiological and clinical advantages of median nerve fascicle transfer to the musculocutaneous nerve following brachial plexus root avulsion injury. J Neurosurg. 2006;105(6):830–834.
- Chuang DC, Lee GW, Hashem F, Wei FC. Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg. 1995;96(1):122–128.
- Chim H, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Triceps motor branch transfer for isolated traumatic pediatric axillary nerve injuries. J Neurgosurg Pediatr. 2015;15(1):107–111.
- Kostas-Agnantis I, Korompilias A,Vekris M, Lykissas M, Gkiatas I, Mitsionis G, et al. Shoulder abduction and external rotation restoration with nerve transfer. Injury. 2013;44(33):299–304.
- Sungpet A, Suphachatwong S, Kawinwonggowit V, Patradul A. Transfer of a single fascicle from the ulnar nerve to the biceps muscle after avulsions of upper roots of the brachial plexus. J Hand Surg. 2000;25(4):325–328.
- Nath RK, Mackinnon SE. Nerve transfers in the upper extremity. Hand Clin. 2000;16(1):131–139.
- Witoonchart K, Leechavengvongs S, Uerpairojkit C, Thuvasethakul P, Wongnopsuwan V. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part I: an anatomic feasibility study. J Hand Surg Am. 2003;28(4):628–632.
- Bertelli JA, Ghizoni MF. Reconstruction of C5 and C6 brachial plexus avulsion injury by multiple nerve transfers: spinal accessory to suprascapular, ulnar fascicles to biceps branch, and triceps long or lateral head branch to axillary nerve. J Hand Surg Arm. 2004;29(1):131–139.
- Zhao X, Hung LK, Zhang GM, Lao J. Applied anatomy of the axillary nerve for selective neurotization of the deltoid muscle. Clin Orthop Relar Res. 2001;390:244–251.
- Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P, Malungpaishrope K. Combined nerve transfers for C5 and C6 brachial plexus avulsion injury. J Hand Surg Am. 2006;31:183–189.
- Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: a report of 7 cases. J Hand Surg Am. 2003;28(4):633–638.
- Sungpet A, Suphachatwong C, Kawinwonggowit V, Patradul A. Transfer of a single fascicle from the ulnar nerve to the biceps muscle after avulsions of upper roots of the brachial plexus. J Hand Surg Br. 2000;25(4):325–328.
- Bertelli JA, Ghizoni MF. Nerve root grafting and distal nerve transfers for C5-C6 brachial plexus injuries. J Hand Surg Am. 2010;35(5):769–775.
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Muscle Nerve. 1999;22(suppl):S3–S300.
Keywords
Single nerve transfer; Pre-ganglionic injury; Avulsion injury
Cite this article
Kovachev M, Kovachev V, Simeonov E, Gigov H, Sadursanska B. Single nerve transfer in case of partial pre-ganglionic injury C5 and avulsion injury C6. Clin Case Rep J. 2023;4(4):1–6.
Copyright
© 2023 Vihar Kovachev. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).