Abstract
Solid Pseudopapillary Neoplasm (SPEN) is a rare tumor found primarily in the pancreas but can occasionally occur extrapancreatic. We present an unusual case of SPN that arose in the ovaries and subsequently metastasized to the peritoneum in a 13-year-old girl. Histopathological examination showed similarities between the characteristics of ovarian neoplasms and those of pancreatic SPNs.
The patient complained of abdominal pain, and imaging studies revealed a well-circumscribed heterogeneous mass in the ovary, initially suspected to be ovarian torsion. The lesion was excised, and the sample was sent to be examined and diagnosed as SPEN through histopathological examination. Immunohistochemistry was positive for beta-catenin, CD10, and vimentin, confirming the diagnosis. Five years later, on an annual follow-up ultrasound, the patient developed a left ovarian lesion; a complementary MRI and diagnostic laparoscopy with tissue sampling confirmed disease recurrence.
Extra pancreatic SPEN is difficult to diagnose due to its rarity and variable clinical presentation. Although imaging studies such as CT and MRI can be helpful in localization and characterization, the final diagnosis depends on histopathological examination and often requires surgical resection. Treatment usually involves complete surgical resection with negative margins, which leads to favorable outcomes. This case highlights the importance of considering SPEN in the differential diagnosis of retroperitoneal masses, especially in younger patients. It also emphasizes the importance of interdisciplinary collaboration involving radiologists, pathologists, and surgeons to diagnose and treat this rare disease accurately. Additional studies are needed to elucidate the molecular mechanisms underlying extrapancreatic SPEN and optimize treatment strategies to improve patient outcomes.
Introduction and Importance
Solid Pseudopapillary Epithelial Neoplasm (SPEN) of the pancreas is a rare cystic exocrine tumor of the pancreas, most commonly occurring in early-age group females. It is a type of neoplasm that arises in the pancreas; it forms 0.3% to 2.7% of all pancreatic exocrine tumors. It is extremely rare to occur outside pancreatic tissues. Several papers have described SPNs arising from ectopic pancreatic tissues such as the ovary, mesocolon, and omentum. We present an unusual case of SPN arising in the ovary of a 13-year-old girl with subsequent peritoneal metastases. Histopathological examination showed properties similar to those of the ovarian neoplasm to those of SPN in the pancreas.
Patient Information
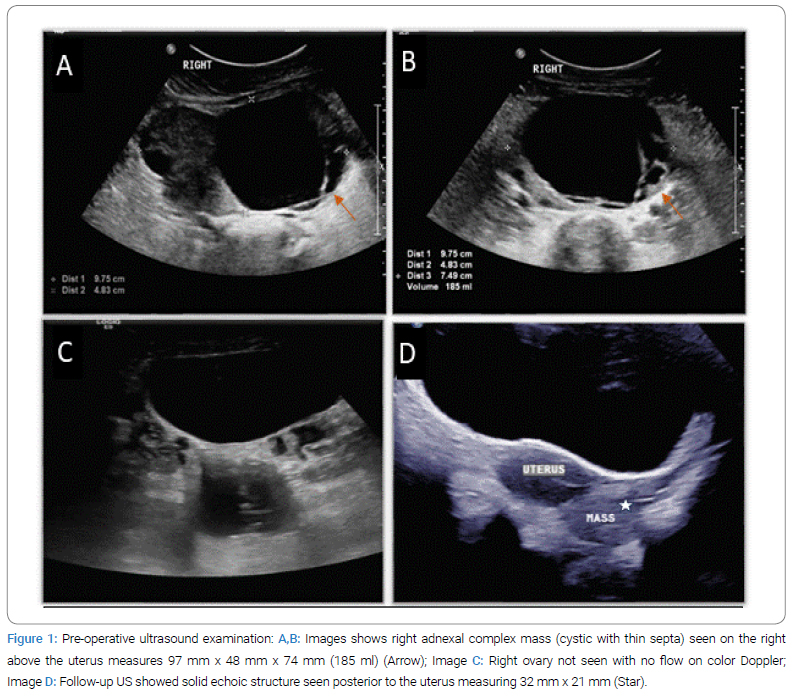
The 13-year-old girl, previously healthy, presented to the emergency department at the hospital with acute lower abdominal pain, which was sudden in onset and gradually progressive; the patient underwent pelvic ultrasound and showed a right adnexal complex mass above the uterus measuring 97 mm x 48 mm x 74 mm (185 ml) with few sepatations (Figure 1), Finding were concerning for ovarian torsion, so laparoscopic detorsion was planned. During the procedure, the surgeon found a right ovarian mass, so the right ovary and right salpingo-oophorectomy were performed, and the right ovarian mass was resected. The gross macroscopic appearance was mainly cystic lesions, which were well-defined in appearance without adjacent organ infiltration.
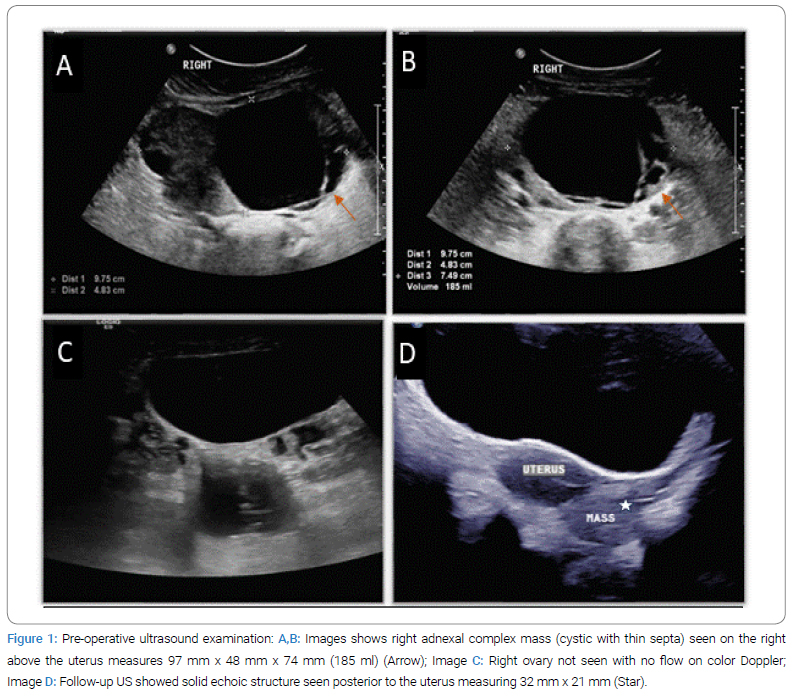
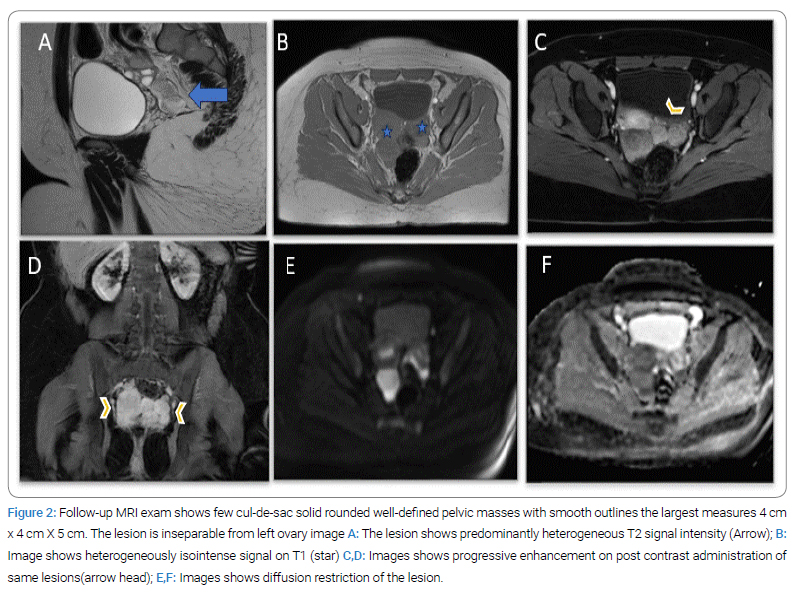
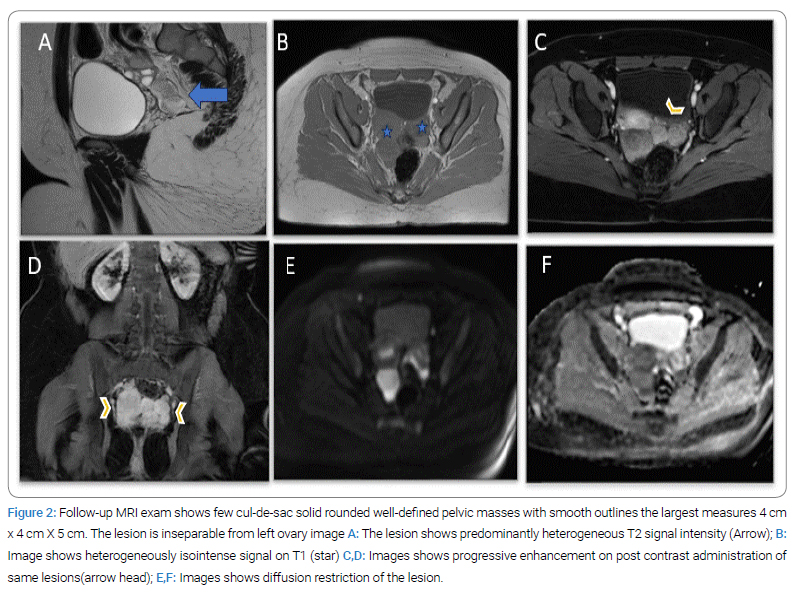
After evaluating the samples, the result came with SPN. 5 years later, the ultrasonography examination follow-up found a left ovarian simple cyst measuring 42 mm x 25 mm x 35 mm, with a positive flow. A complementary MRI was performed (Figure 2) and demonstrated a few culde-sac-enhancing solid masses, most likely representing disease recurrence. The patient again underwent diagnostic laparoscopy and intraoperatively saw multiple peritoneal lesions in the pelvis, bilateral paracolic gutters, right hemidiaphragm, and omentum lobulated masses adherent to the peritoneal cavity. The left ovary is enlarged.
So, an omental biopsy, peritoneal biopsy, and a left ovarian partial oophorectomy were performed. Histopathology shows features consistent with metastatic foci of solid pseudopapillary tumor in omentum excision, with multiple microscopic foci, the largest of which is 9 mm in diameter. The left ovary shows multiple follicular cysts. The biopsy was negative for malignancy.
The right hemidiaphragm peritoneal excision shows fibrosis and mesothelial hyperplasia. Negative for malignancy.
Pathological Findings
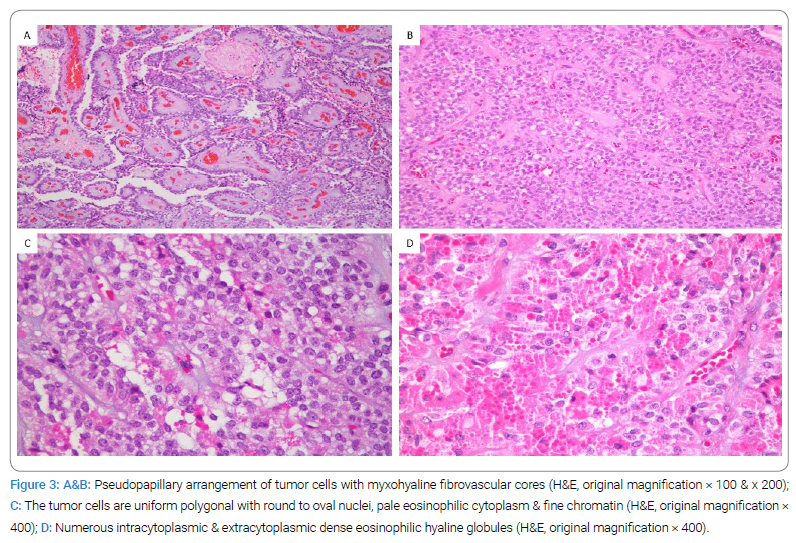
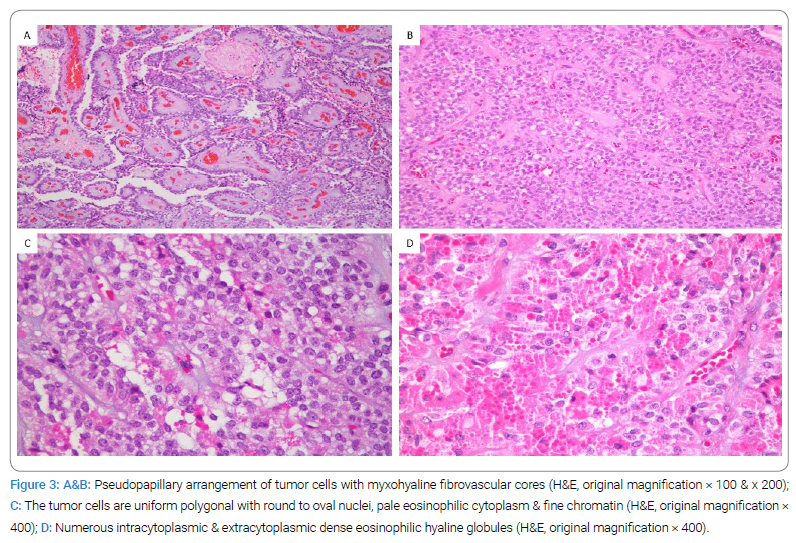
Histopathological examination demonstrated a well-circumscribed tumor with a nodular growth pattern. The tumor cells are arranged in pseudopapillae, nests, and sheets with irregular cystic spaces in between (Figure 1A,Figure 1B). The pseudopapillary consisted of the central fibrovascular core with thin-wall blood vessels and myxo hyaline stroma (Figure 1A). They were covered with one to multiple layers of tumor cells with the antipodal arrangement of nuclei. The tumor cells are uniform medium-sized polygonal with round to oval nuclei, nuclear groves, pale eosinophilic cytoplasm, and fine chromatin (Figure 1C). Abundant intracytoplasmic and extracytoplasmic dense eosinophilic hyaline globules were present (Figure 1D). No mitosis, necrosis, or pleomorphism was identified. Furthermore, there were metastatic tumor deposits on the omentum, peritoneal wall, appendix, large bowel, and small bowel.
Special stain Periodic Acid-Schiff (PAS) was performed to highlight the eosinophilic hyaline globules.
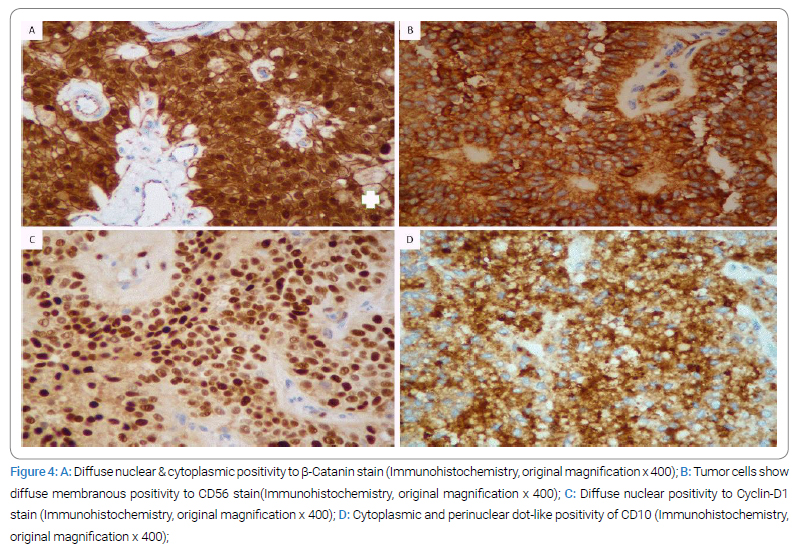
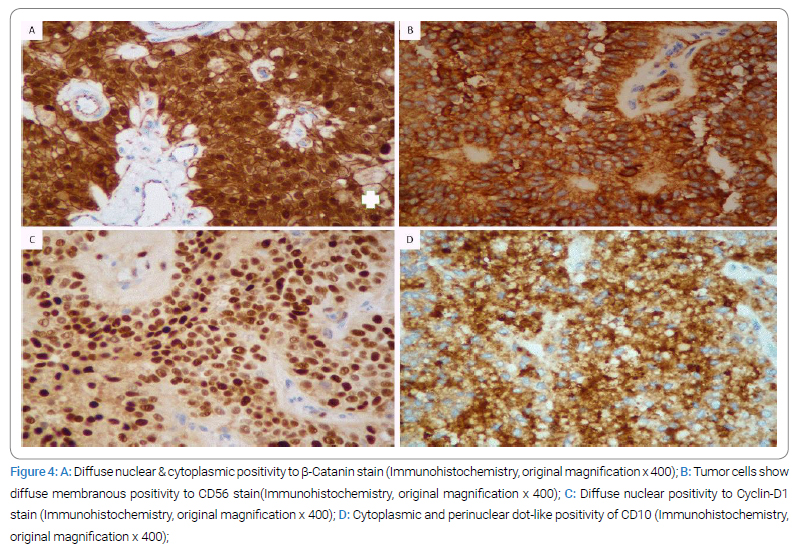
By Immunohistochemistry, the tumor cells exhibited positivity for Beta-catenin (nuclear and cytoplasmic staining) (Figure 2A), CD56 (membranous staining) (Figure 2B), CAM 5.2 (focally), cyclin D1 (nuclear staining) (Figure 2C), PR (nuclear), vimentin (nuclear and cytoplasmic) and CD10 (cytoplasmic and perinuclear dot-like staining) (Figure 2D). They were negative for PLAP, inhibin, chromogranin, synaptophysin, WT-1, Pan-Cytokeratin, TTF1, AFP, CD 99, ER, and calretinin. In addition, there was the loss of membranous staining of E-cadherin. Ki-67 proliferative index was low, < 5%. The overall histological and immunophenotypical features were consistent with diagnosing an Extra pancreatic ovarian solid pseudopapillary tumor.
Discussion
Solid pseudopapillary tumor is a rare, low-grade malignancy that primarily affects women in their 20s or 30s and most commonly occurs in the pancreas. However, cases of SPEN occurring as a primary tumor other than the pancreas have been reported in the literature, but this phenomenon is extremely rare worldwide. Most SPEN tumors show benign behavior. However, approximately 15% of SPENs display aggressive features such as ill-defined borders, metastases, or invasion of adjacent structures.
The liver is reported to be the most common site of distant metastases. For SPEN, surgical resection is the treatment of choice regardless of tumor recurrence or metastasis, and the prognosis after surgery is generally good. Extra pancreatic SPEN is unusual; however, we report a case of a primary ovarian lesion with metastases to the peritoneum in a 13-year-old girl. Ultrasound and magnetic resonance imaging were done before the surgery. Because the patient was in pain and suspicious of ovarian torsion is present, a diagnostic laparoscopy was performed to confirm right ovarian torsion due to an underlying ovarian lesion. Accordingly, the patient subsequently underwent right salpingeo-oophorectomy after fixation of the right ovary, no primary pancreatic mass detected. Immunohistochemical data showed similarities between the characteristics of pancreatic SPEN and those of ovarian neoplasms. Five years later, the patient returned to the hospital with abdominal pain. MRI scan revealed tumor recurrence with multiple peritoneal lesions. Additionally, diagnostic laparoscopy and biopsy were performed on these tumors, and the diagnosis of extrapancreatic recurrent solid papillary tumor of the ovary was confirmed through histopathological examination. In this age group, the major differential diagnoses of ovarian SPN include sex cord [1]. According to one piece of literature we reviewed, the ovaries are the most common site for extrapancreatic SPEN, and the main clinical symptoms of SPEN are abdominal pain, bloating, and discomfort caused by the tumor compressing surrounding structures. Only 15% develop metastases, 21% have tumor recurrence, and long-term survival is observed in more than 95% of cases.
Immunohistochemical staining of biopsy or surgical resection specimens is the mainstay of diagnosis and differential diagnosis, and the most distinctive immunohistochemical signature is abnormal nuclear β-catenin staining. The best treatment for extrapancreatic SPN is radical surgical resection. In addition to surgery, traditional adjuvant treatments such as Hyperthermic Intraperitoneal Chemotherapy (HIPEC), Radiofrequency Ablation (RFA), percutaneous arterial embolization, radiotherapy, and chemotherapy in advanced cases can also be used to treat SPEN [2]. In a previous clinical study, a 40-year-old Chinese man underwent abdominal computed tomography after complaining of abdominal pain, which revealed a large mesenteric solid and mixed cystic lesion. The patient underwent exploratory laparotomy, and the tumor was removed. It protrudes from the mesentery without invasion or attachment to surrounding organs. Therefore, the tumor was completely removed, and a mixture of solid and pseudopapillary areas was observed in the mesenteric tumor specimen. Additionally, the patient continued to complain of abdominal distension, and an abdominal CT scan confirmed recurrent disease [3]. Another case report of a 61-year-old woman diagnosed with extrapancreatic SPEN with aggressive features described as follows: mass with indistinct margins, involvement of adjacent abdominal organs with multiple seeded masses, scalloped liver surface, extensive Peritoneal dissemination, and liver.
Another case reported a 25-year-old unmarried female presented with lower abdominal pain. Abdominal CT showed a well-defined right adnexal mass with solid and cystic components, cancer antigen-125 (CA-125), beta-human chorionic gonadotropin, α-fetoprotein, CA19-9, and carcinoembryonic antigen was within normal limits. The patient underwent right salpingo-oophorectomy, total omentectomy, macroscopic clearance of the tumor, and pelvic lymph node dissection.
Microscopic examination revealed a neoplasm composed of pseudopapillae lined by polyhedral cells. Omentum, parametria, and pelvic lymph nodes showed tumor metastases. The pancreatic and extrapancreatic solid pseudopapillary tumors have identical histological and immunohistochemical features in which the tumor cells are arranged in pseudopapillae, solid nests, and sheets. The pseudopapillae consisted of central fibrovascular core with myxohyaline stroma. The tumor cells are uniform medium-sized polygonal with round to oval nuclei, nuclear groves, fine chromatin, and pale eosinophilic cytoplasm with abundant intracytoplasmic and extracytoplasmic dense eosinophilic hyaline globules (Figure 1,Figure 3).
Solid pseudopapillary tumors are pancreatic and ovarian versions that are commonly positive for Beta-catenin, CD56, vimentin, and CD10 immunohistochemical stains. And negative to E-Cadherin, similar to our case.
However, regarding ovarian solid pseudopapillary tumors, a certain number of differential diagnoses should be excluded before making this diagnosis, such as sex cord-stromal tumor, germ cell tumor, struma ovarii, and high-grade epithelial neoplasms (Figure 4). Immunohistochemical stains play an important role in differential diagnosis exclusion. The negativity of Calretinin, inhibin, PLAP, and AFP IHC stains exclude sex cord-stromal tumors and germ cell tumors. The presence of immunoreactivity of TTF1 help to distingue struma ovarii from an ovarian solid pseudopapillary tumor. The absence of positivity to cytokeratin and low percentage of Ki67 proliferative index go more with ovarian solid pseudopapillary tumors than high-grade epithelial tumors [1,4]. In summary, we presented a unique report of recurrent primary ovarian SPEN with typical histologic and immunohistochemical features. Additionally, our patient only underwent surgery and did not receive any other treatment, such as chemotherapy or radiation therapy. SPN generally has a good prognosis after surgery, but in 21% of cases, the tumor recurs. Surgery is curative and should be attempted for localized disease, and a prolonged survival rate has been reported after complete excision in patients with metastasis. The role of chemotherapy is limited in unresected tumors.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
SPEN; Ovarian neoplasm; Tumor; Beta-catenin; CD10; Extra pancreatic SPEN
Cite this article
Zakri AK, Alkhelaiwi FS, Mashhor YM, Alzahrani AH, Alkhunaizi ZF, Elhassan MA. Extra- pancreatic solid pseudopapillary epithelial neoplasm (SPEN) – case study. Clin Case Rep J. 2024;5(1):1–5.
Copyright
© 2024 Zakri AK. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).