Abstract
The distinction between congenital teratoma, lymphatic malformation, and choristoma is difficult in cross-sectional studies in patients with heterogeneous multi-compartmental pharyngeal mass.
We presented with a 1-month-old - male baby with an antenatal diagnosis of oropharyngeal mass who presented with difficulty breathing and feeding. Radiological studies showed a large multi-compartmental heterogenous pedunculated pharyngeal mass, obliterating the airways and occupying the oral cavity with severe mass effect and intracranial extension. Histopathologic examination showed neuroglial heterotopia confirming choristoma. In conclusion, choristoma should be a differential diagnosis of a newborn patient with oropharyngeal mass.
Introduction
In the pediatric population, the head and neck region is a common location for benign abnormal tissue proliferations, including ectopias, heterotopias, choristomas, and hamartomas. The term choristoma applies to a cohesive tumor-like mass consisting of normal cells in an abnormal location. Choristomas of the head and neck can occur in the tongue (lingual choristoma), the floor of the mouth, pharynx, and hypopharynx and are clinically important lesions because they can be a cause of neonatal airway obstruction and significant feeding difficulties. Choristomas of the oral cavity can be classified according to the various types of tissues they constitute (salivary gland choristoma, cartilaginous, osseous, lingual thyroid, lingual sebaceous, glial, and gastric/respiratory mucosal). Glial choristomas of the oral cavity are considered brain heterotopias composed of ectopic central nervous tissue arising as a developmental malformation with a tumor-like growth [1,2]. The authors report a case of glial choristomas, which was initially misdiagnosed. We present a 1-month-old male baby presented with a large multicompartmental pharyngeal mass mimicking congenital teratoma/ lymphatic malformation but diagnosed as oropharyngeal choristoma by histopathological examination.
Case Presentation
A case of a 1-month-old male baby delivered by exit procedure due to an antenatal diagnosis of oropharyngeal mass transferred by the age of 4 weeks for further management of large oropharyngeal, which was diagnosed antenatally; no further detailed history available.
Upon admission, a visible oral lesion measuring around 8 x 6 centimeters, likely arising from the soft palate, was found on physical examination. The patient was not fed by mouth and was on TPN feeding.
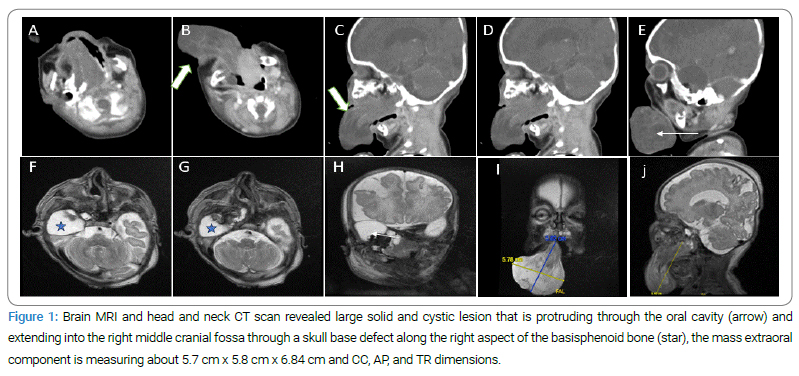
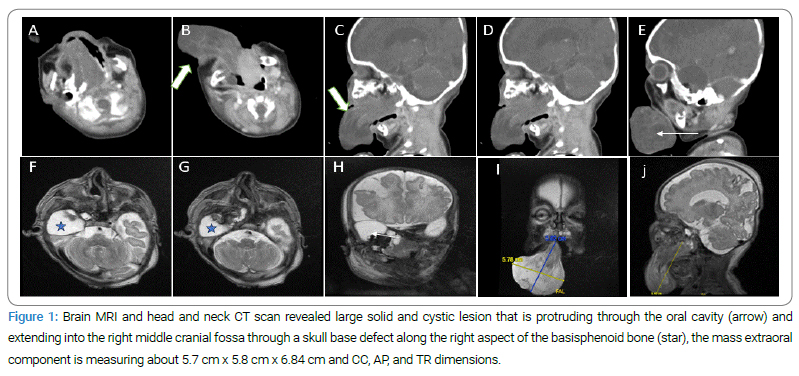
Brain MRI and head and neck CT scan revealed a large solid and cystic lesion that is protruding through the oral cavity and extending into the right middle cranial fossa through a skull base defect along the right aspect of the basisphenoid bone. Exerting a mass effect results in posterior displacement of the oral tongue and narrowing of the oropharyngeal recess (Figure 1).
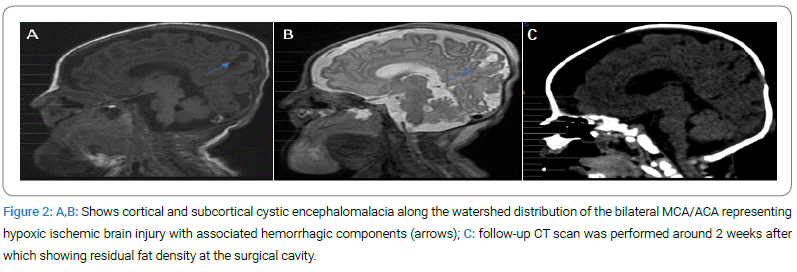
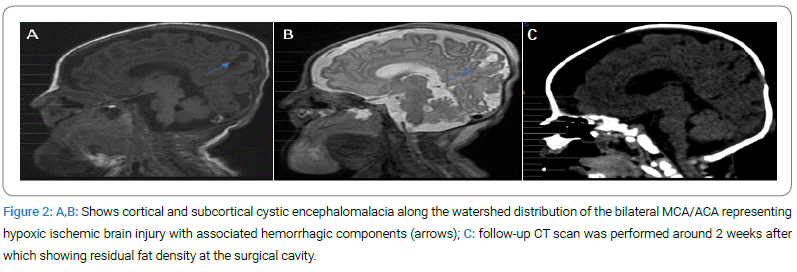
In addition to cortical and subcortical cystic encephalomalacia along the watershed distribution of the bilateral MCA/ACA representing hypoxic-ischemic brain injury with associated hemorrhagic components (Figure 2A,Figure 2B).
The temporal cystic lesion was resectioned when the patient was six weeks old, after which the patient was transferred to the NICU. Five days later, another operation was performed for oropharyngeal mass resection and skull base repair with inferiorly based phalangeal flap insertion for the palatal defect.
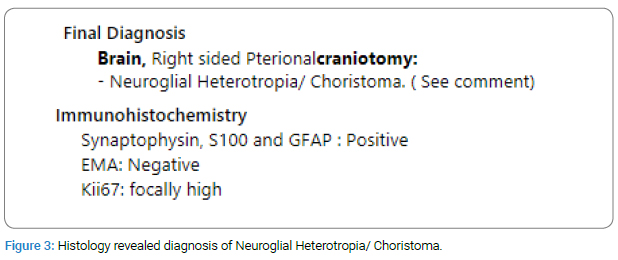
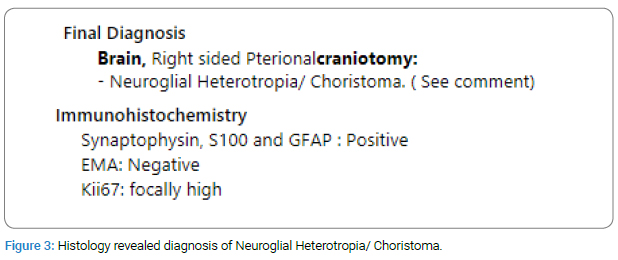
On day 5, post-surgery histology revealed a diagnosis of Neuroglial Heterotropia/Choristoma. No signs of malignancy were observed (Figure 3).
A follow-up CT scan was performed around two weeks after that, showing residual fat density in the surgical cavity (Figure 2C).
Discussion
The presented case report highlights the rare occurrence of a choristoma in the oropharynx, shedding light on the diagnostic challenges and management options associated with this condition. Choristomas are uncommon developmental anomalies characterized by the presence of ectopic tissue in an organ or location where it is not normally found. In this particular case, the oropharyngeal choristoma was identified as a benign mass composed of adipose tissue and salivary gland tissue [2,4–6].
Diagnosing oropharyngeal choristoma can be challenging due to its rarity and nonspecific clinical presentation. In this case, the patient presented with an antenatally diagnosed oropharyngeal mass, which prompted further investigation. Clinical examination alone may not be sufficient for a definitive diagnosis. Thus, imaging studies such as CT scans or MRIs can provide valuable insights into the location, size, and characteristics of the choristoma. Histopathological analysis of a biopsy specimen remains the gold standard for confirmation [2,4].
Treatment options for oropharyngeal choristoma depend on various factors, including the size, location, and symptomatic impact of the lesion.
In some cases, conservative management with regular monitoring may be appropriate, especially if the choristoma is small and asymptomatic. However, in cases where the choristoma causes significant symptoms or functional impairment, surgical excision is often recommended. The surgical approach should be tailored to the individual patient, considering factors such as the size and location of the choristoma, as well as the potential risks and benefits of the procedure [2,3].
The prognosis for oropharyngeal choristoma is generally favorable. Most cases resolve completely or show minimal recurrence after appropriate treatment. Long-term follow-up is essential to monitor for any potential recurrence or complications [3].
In conclusion, the presented case report on oropharyngeal choristoma emphasizes the importance of considering this rare developmental anomaly in the differential diagnosis of oropharyngeal masses. The case highlights the challenges in diagnosis and the importance of a multidisciplinary approach involving clinical examination, imaging studies, and histopathological analysis. Furthermore, it underscores the significance of individualized treatment plans based on the specific characteristics and impact of the choristoma. Continued research and reporting of such cases will contribute to a better understanding of this rare condition and guide the development of optimal management strategies.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Oropharyngeal choristoma; Histopathological analysis; Tissue proliferations
Cite this article
Aldraihem AI, Aljaber AA, Almoabid ZA, Aljudaie AA, Alamoudi RH, Alshammari LK, et al. Large oropharyngeal choristoma: Case Report. Clin Case Rep J. 2024;5(2):1–3.
Copyright
© 2024 Aldraihem AI. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).