Complex Presentation and Management of Upper Gastrointestinal Bleeding from Aberrant Right Subclavian Artery: A Case Report
* Asrar Ageeli;
Joud Bahakeem;
Almoaiad Alhazemi;
-
* Asrar Ageeli: Senior Radiology Registrar, Jazan Health Cluster, Jazan, Saudi Arabia.
-
Joud Bahakeem: Radiology Resident, King Fahd General Hospital, Jeddah, Saudi Arabia.
-
Almoaiad Alhazemi: Consultant Intervention Radiology, Jazan Health Cluster, Jazan, Saudi Arabia.
Abstract
Upper gastrointestinal (GI) bleeding is a serious medical condition with various etiologies, including vascular anomalies like an Aberrant Right Subclavian Artery (ARSA) esophageal fistula.
ARSA is a congenital anomaly that can lead to rare but life-threatening complications such as severe GI bleeding. This case report details the complex presentation and management of a 27-year-old woman with an ARSA esophageal fistula. Initially presenting with a severe headache and subsequent dural sinus thrombosis, her condition rapidly deteriorated, leading to the discovery of the ARSA anomaly and associated fistula. Management included the deployment of a covered balloon-mounted stent to seal the fistula and stop the bleeding. Despite the successful intervention, the patient remained hemodynamically unstable and ultimately succumbed to cardiac arrest on postoperative day 10. This report highlights the importance of early diagnosis and multidisciplinary management in such complex cases.
Introduction
Upper gastrointestinal (GI) bleeding is a serious medical condition that can result from various etiologies, including peptic ulcers, varices, and vascular anomalies. One of the rare but life-threatening causes of upper GI bleeding is an esophageal fistula associated with an Aberrant Right Subclavian Artery (ARSA). The ARSA, also known as arteria lusoria, is a congenital vascular anomaly in which the right subclavian artery arises abnormally from the aortic arch, passing behind the esophagus [1]. Although most individuals with ARSA are asymptomatic, complications such as dysphagia, respiratory issues, and, in rare instances, fistula formation leading to massive GI bleeding can occur [2].
Several studies have documented the incidence and clinical implications of ARSA. ARSA is the most common congenital anomaly of the aortic arch, occurring in approximately 0.5% to 2% of the population [3,4]. While many individuals with ARSA remain asymptomatic throughout their lives, symptomatic cases often present with dysphagia lusoria, a condition characterized by difficulty swallowing due to the compression of the esophagus by the aberrant artery [5]. Other less common symptoms include chronic cough, chest pain, and respiratory distress. In rare cases, ARSA can lead to the development of a fistula between the artery and the esophagus, resulting in severe upper GI bleeding [6].
The literature on ARSA-related esophageal fistulas and their management is limited, with most available information derived from case reports and small case series. Endovascular techniques have emerged as a preferred method for managing complications due to their minimally invasive nature and favorable outcomes [7]. For instance, the deployment of covered stent grafts has effectively sealed the fistula and stopped the bleeding. However, surgical interventions, including open repair and esophagectomy, may still be necessary in cases where endovascular treatment is not feasible or fails to resolve the issue [8]. Despite advancements in these techniques, the mortality rate associated with ARSA esophageal fistulas remains high (64.3%), underscoring the need for early diagnosis and intervention [9].
Existing studies provide insights into ARSA complications but lack comprehensive reviews of complex cases like upper GI bleeding from ARSA esophageal fistulas. Most reports focus on isolated cases, ignoring broader implications and challenges. Due to its rarity, many clinicians may need to familiarize themselves with this condition’s presentation and management. Our case report addresses this by detailing the clinical presentation, diagnosis, and treatment of a life-threatening ARSA esophageal fistula. We aim to enhance knowledge and offer practical insights to aid clinicians in managing similar cases.
Case Presentation
A 27-year-old woman who had recently undergone a cesarean section (C-section) presented to the emergency department with a severe headache. Initial imaging with a CT scan of her brain was unremarkable, but subsequent Magnetic Resonance Venography (MRV) revealed dural sinus thrombosis. The patient remained stable on medication until she suddenly deteriorated, showing a decreased level of consciousness. The ICU team intubated her, and a follow-up CT scan showed diffuse brain edema, tonsillar herniation, and communicating hydrocephalus.
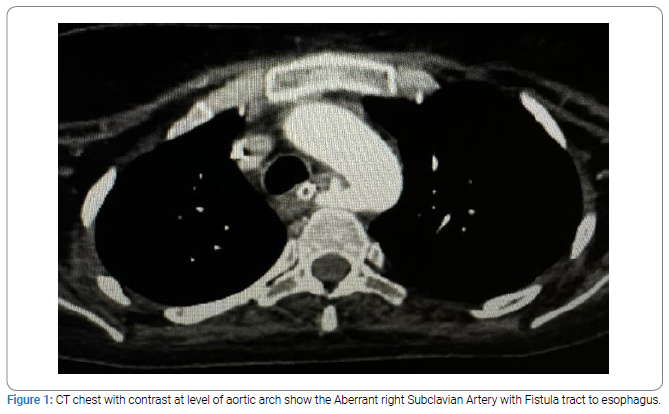
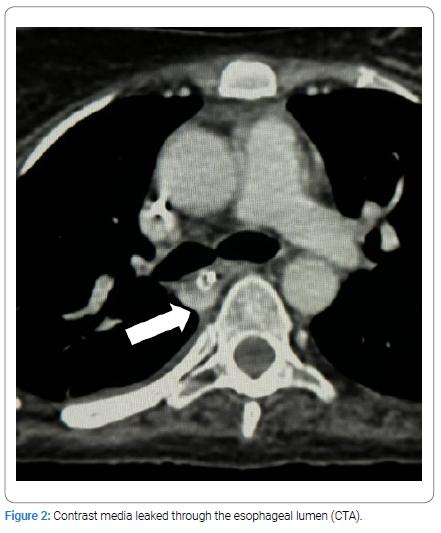
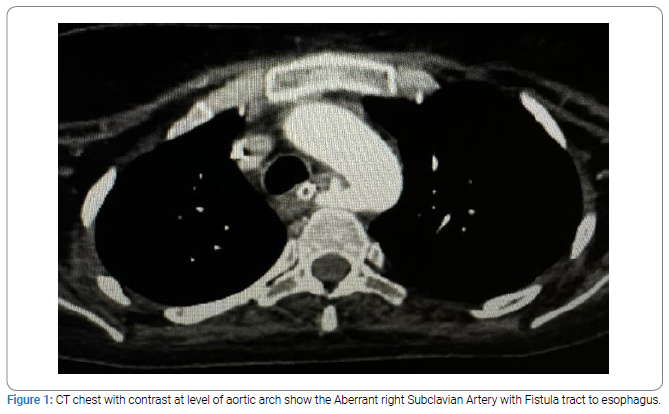
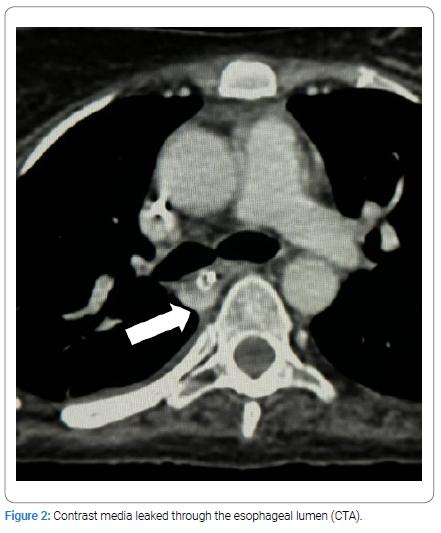
Several days later, the patient became hypotensive, and a CT-Angiography (CTA) revealed an ARSA passing between the trachea and esophagus, with an abnormal fistulous communication between the artery and the esophagus. The fistula, located about 5mm from the ARSA’s origin, had a diameter of approximately 4mm, with active bleeding observed as contrast media leaked through the esophageal lumen (Figure 1,Figure 2). Both an Endotracheal Tube (ETT) and a Nasogastric Tube (NGT) were in situ.
The patient was transferred to King Fahad General Hospital in Jazan City from a private hospital, where she was admitted to the Intensive Care Unit (ICU) for four months following a Cerebrovascular Accident (CVA), during which she developed brain edema and underwent a craniotomy. Upon arrival, she was in a deep coma, with a Glasgow Coma Scale (GCS) score of 3/15 and bilaterally dilated pupils. She had been on a tracheostomy for one and a half months and developed significant oral bleeding on the day of transfer. A CT scan of her neck and chest with contrast confirmed the ARSA anomaly with an esophageal fistula and contrast leakage.
The patient received four units of Packed Red Blood Cells (PRBCs) and an Esomeprazole infusion. She was referred to vascular and interventional radiology for further management. After initial stabilization with fluids, blood products, and hemodynamic monitoring, the patient was transferred to the interventional radiology suite.
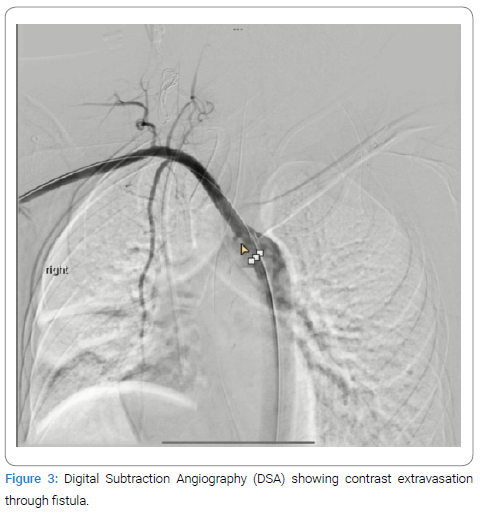
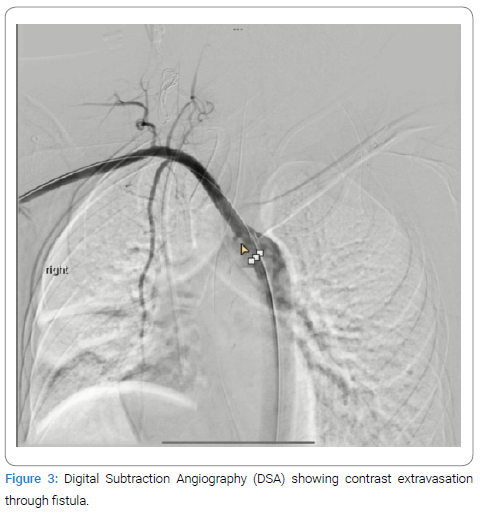
The procedure involved accessing the right common femoral artery and performing diagnostic angiography to confirm the location and morphology of the ARSA and the fistula (Figure 3).
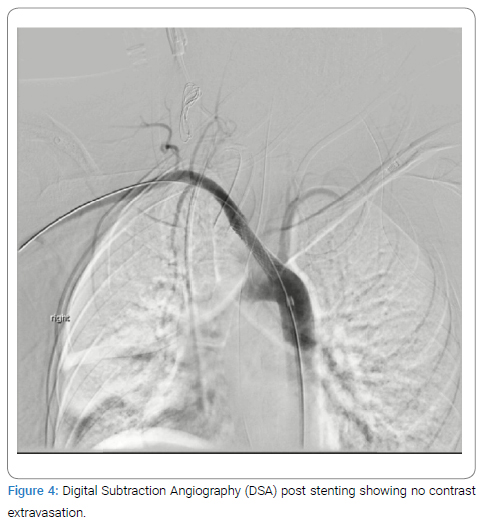
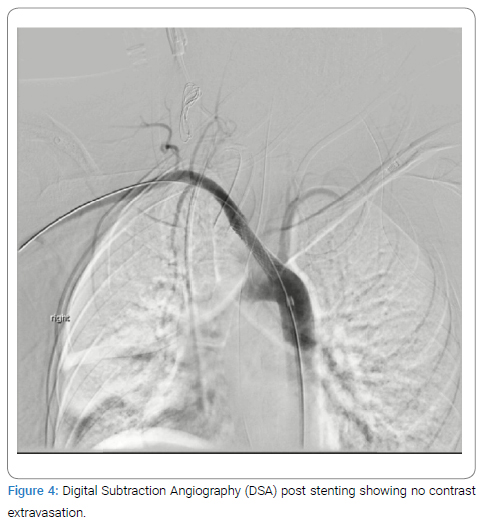
A covered balloon-mounted stent, designed to accommodate the ARSA’s size, was deployed. The stent graft was positioned to cover the ARSA’s origin from the aorta, extending distally beyond the fistula. Care was taken to ensure precise deployment, avoiding the coverage of vital branches and effectively sealing the fistula. Post-deployment angiography confirmed the exclusion of the ARSA and cessation of bleeding (Figure 4).
Postoperatively, the patient was monitored in the intensive care unit. Despite being hemodynamically unstable and requiring Levophed, she had two days of melena and clotted blood in the NGT, but no groin hematoma was observed. After two days, melena ceased, and only a small amount of secretion was sucked from the NGT. The patient remained under close monitoring in the ICU. Unfortunately, on postoperative day 10, the patient experienced cardiac arrest and died in the ICU.
Discussion
The case of upper gastrointestinal bleeding due to ARSA esophageal fistula presented here is a rare but critical condition that underscores the importance of early diagnosis and intervention. ARSA is a congenital anomaly where the right subclavian artery arises abnormally from the aortic arch and passes behind the esophagus. Most individuals with ARSA are asymptomatic, but complications can arise, such as dysphagia lusoria, respiratory issues, and, in rare cases, fistula formation leading to severe GI bleeding. Our patient’s initial presentation with severe headache and subsequent finding of dural sinus thrombosis is unusual and not typically associated with ARSA. This initial complication, followed by severe brain edema and tonsillar herniation, added complexity to the clinical picture. Similar cases reported in the literature emphasize that while ARSA-related complications are rare, they can present with diverse and severe symptoms [10,11].
The discovery of the ARSA and the fistulous communication via CTA was critical in diagnosing the source of the GI bleeding. As corroborated by several studies, CTA is highly effective in identifying vascular anomalies and active bleeding sites. For instance, Erno et al. demonstrated that CTA has a high sensitivity and specificity for detecting GI bleeding sources, making it a valuable tool in emergency settings [12]. Our case aligns with these findings, as CTA promptly identified the ARSA anomaly and the esophageal fistula, facilitating immediate intervention [13].
The endovascular approach to managing the ARSA esophageal fistula in our patient involved the deployment of a covered balloon-mounted stent. This minimally invasive technique is increasingly preferred for its efficacy and reduced morbidity compared to open surgical methods. According to Toit et al., endovascular stent-grafting is an effective method for treating ARSA-related complications, providing good short—and long-term outcomes [14]. In our case, the precise placement of the stent graft successfully excluded the ARSA and stopped the bleeding, confirming the efficacy of this approach.
Post-procedure, the patient remained hemodynamically unstable, requiring vasopressor support with Levophed. This instability can be attributed to the severe preoperative condition, including significant blood loss and underlying critical illness. Studies by Moll et al. highlight that post-intervention hemodynamic instability is uncommon, especially in patients with complex comorbidities [15]. Despite the cessation of GI bleeding, the patient’s poor neurological status and prolonged ICU stay with complications such as brain edema and tracheostomy further complicated recovery.
The high mortality rate associated with ARSA esophageal fistulas, as observed in our patient, underscores the severity of this condition. Literature reports a significant risk of mortality, particularly when diagnosis and intervention are delayed. A study by Chiesa et al. noted that early recognition and prompt endovascular treatment are crucial in improving outcomes for patients with vascular esophageal fistulas [16]. However, even with timely intervention, the prognosis can be poor if the patient has severe comorbid conditions, as seen in our case.
Thus, the management of upper gastrointestinal bleeding due to an ARSA esophageal fistula requires a multidisciplinary approach involving prompt diagnostic imaging, endovascular intervention, and intensive postoperative care. The high mortality rate associated with this condition highlights the need for early detection and comprehensive management strategies. Further studies are needed to explore the best practices in managing ARSA complications, particularly in patients with complex comorbidities.
Conclusions
This case report underscores the critical nature of upper gastrointestinal bleeding due to ARSA esophageal fistula. Early CTA diagnosis and prompt endovascular intervention with a covered stent graft can effectively manage the bleeding. However, the presence of severe comorbid conditions, such as brain edema and prolonged ICU stay, complicates recovery and significantly impacts prognosis. It highlights the need for a multidisciplinary approach to managing rare and life-threatening conditions and emphasizes the importance of prompt, coordinated care to improve patient outcomes.
References
- Polguj M, Chrzanowski Ł, Kasprzak JD, Stefańczyk L, Topol M, Majos A. The aberrant right subclavian artery (arteria lusoria): the morphological and clinical aspects of one of the most important variations--a systematic study of 141 reports. ScientificWorldJournal. 2014;2014:292734.
- Peress S, Tuqan W, Thomas A. Upper gastrointestinal bleeding from aberrant right subclavian artery-esophageal fistula. Ochsner J. 2021;21(4):406–412.
- Türkvatan A, Büyükbayraktar FG, Olçer T, Cumhur T: Congenital anomalies of the aortic arch: evaluation with the use of multidetector computed tomography. Korean J Radiol. 2009;10(2):176–184.
- Goldmuntz E. The genetic contribution to congenital heart disease. Pediatric Clinics of North America. 2004;51(6):1721–1737.
- Mansour MM, Darweesh M, Mahfouz R, Obeidat AE, Das K. Aberrant right subclavian artery causing dysphagia: a case report of dysphagia lusoria. Cureus. 2022;14(6):e25980.
- Jain KK, Braze AJ, Shapiro MA, Perez-Tamayo RA. Aberrant right subclavian artery-esophageal fistula and severe gastrointestinal bleeding after surgical correction of scimitar syndrome. Tex Heart Inst J. 2012;39(4):571–574.
- Ahmed SB, Settembre N, Touma J, Brouat A, Favre JP, Baptiste EJ, et al. Outcomes in the treatment of aberrant subclavian arteries using the hybrid approach. Interact Cardiovasc Thorac Surg. 2022;35(5):ivac230.
- Atay Y, Engin C, Posacioglu H, Ozyurek R, Ozcan C, Yagdi T, et al. Surgical approaches to the aberrant right subclavian artery. Tex Heart Inst J. 2006;33(4):477–481.
- Kudose S, Pineda J, Saito JM, Dehner LP. Aberrant right subclavian artery-esophageal fistula in 20-year-old with vater association. J Pediatr Intensive Care. 2017;6(2):127–131.
- Epstein DA, De Bord JR. Abnormalities associated with aberrant right subclavian arteries-a case report. Vasc Endovascular Surg. 2002;36(4):297–303.
- Heye T, Greiten L, Story-Hefta L, Reemtsen B, Moursi M. Aberrant right subclavian artery: a novel approach and an overview of operative techniques. J Vasc Surg Cases Innov Tech. 2023;9(4):101327.
- Erno J, Gregoski MJ, Rockey DC. Diagnostic utility of CT angiography compared with endoscopy in patients with acute GI hemorrhage. Gastrointest Endosc. 2024;99(2):257–261.e5.
- Mirande MH, Durhman MR, Smith HF. Anatomic investigation of two cases of aberrant right subclavian artery syndrome, including the effects on external vascular dimensions. Diagnostics. 2020;10:592.
- du Toit DF, Lambrechts AV, Stark H, Warren BL. Long-term results of stent graft treatment of subclavian artery injuries: management of choice for stable patients? J Vasc Surg. 2008;47(4):739–743.
- Scott MJ, APSF Hemodynamic Instability Writing Group. Perioperative patients with hemodynamic instability: consensus recommendations of the anesthesia patient safety foundation. Anesth Analg. 2024;138(4):713–724.
- Chiesa R, Melissano G, Marone EM, Kahlberg A, Marrocco-Trischitta MM, Tshomba Y. Endovascular treatment of aortoesophageal and aortobronchial fistulae. J Vasc Surg. 2010;51(5):1195–1202.
Keywords
Aberrant subclavian artery; Endovascular procedures; Esophageal fistula; Gastrointestinal hemorrhage; Vascular anomalies
Cite this article
Ageeli A Bahakeem J, Alhazemi A. Complex presentation and management of upper gastrointestinal bleeding from aberrant right subclavian artery: A case report. Clin Case Rep J. 2024;5(3):1–5.
Copyright
© 2024 Asrar Ageeli. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).