A Rare Condition Resembling Breast Cancer: Case Report
Almousa A;
* Alshaia A;
-
Almousa A: Department of Radiology, King Fahad Medical City, Riyadh, Saudi Arabia.
-
* Alshaia A: Department of Radiology, King Fahad Medical City, Riyadh, Saudi Arabia.
-
Mar 17, 2025 |
-
Volume: 6 |
-
Issue: 1 |
-
Views: 1287 |
-
Downloads: 1205 |
Abstract
Introduction: Diabetic Mastopathy (DMP) is an uncommon benign breast condition that affects patients with long-standing type 1 diabetes, presenting a dilemma for clinicians and causing fear for patients due to its resemblance to breast cancer. The interpretation of the imaging results and the attainment of an accurate standard diagnostic remain hypothetical. We reported a case of a woman with Type I Diabetes Mellitus to highlight the radiological findings of this benign breast illness and to enhance awareness.
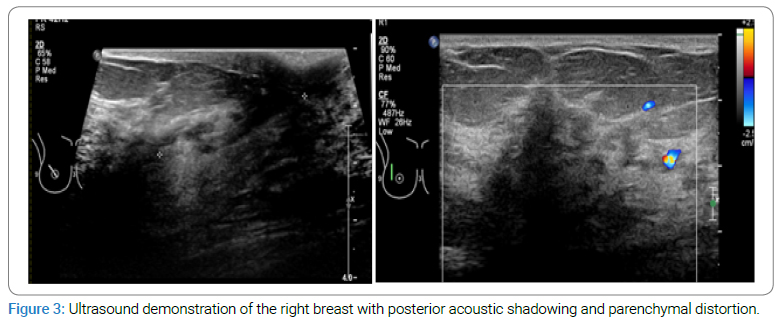
Case presentation: The patient is a 43-year-old, single Saudi lady who presented with a right breast mass for 4 months of duration; she is known to have long-standing type 1 insulin-dependent diabetes mellitus and has been treated for the last 27 years; she also suffers from obesity with BMI of 35.9. The mammogram revealed a dense breast with focal asymmetry in the right outer upper breast with no suspicious microcalcification. Her ultrasound demonstrated a suspicious hypoechoic ill-defined mass in the 10 o’clock position of the right breast with posterior acoustic shadowing and parenchymal distortion, no lymphadenopathy (BIRAD IV), hence a true cut biopsy was needed. Histologically, the lesion showed predominantly stromal fibrosis/elastosis with periductal chronic inflammation and reactive atypia consistent with DMP.
Discussion: The radiographic features observed in our study were nonspecific. In consequence, a core-needle biopsy is essential. Comparable studies also found that DMP is a challenge for doctors, and it needs further studies to emphasize the diagnosis. Recurrence of DMP after surgical excision has been reported. However, our patient didn’t undergo any surgery.
Conclusion: The uncommonness of DMP makes an accurate diagnosis challenging since its imaging features mimic breast cancer. Hence, a tissue biopsy, careful correlation of the patient’s history, and physical examination with the radiology and histology results are required to establish a diagnosis.
Abbreviations
DMP: Diabetic Mastopathy; BI-RADS: Breast Imaging Reporting and Data
Introduction
DMP is a rare benign breast disease that affects diabetic patients (long-standing diabetes type 1); it can be a dilemma for the physician and a source of anxiety for the patients since it mimics breast cancer. Interpreting the imaging result and reaching a precise standard diagnosis is still under hypothesis.
Soler and Khardori [1] were the first to discover the association between diabetes and mastopathy. It was characterized as a breast mass with fibrous tissue and lymphocyte infiltrations in patients with type I Diabetes Mellitus (DM). DMP has been known as a consequence of type I DM. However, some studies have reported that DMP can be associated with type II DM [2,3].
One of the latest studies in 2015 showed that most of the DMP lesions show either negative findings or nonspecific focal asymmetry on mammograms, while the US features are more suspicious, categorizing them as BI-RADS IV and making the biopsy essential to reach a diagnosis [4].
The published research that illustrates this topic is limited and shows nonspecific or absent radiographic and ultrasonographic features [5]. We presented a case of DMP (Type I DM) in a lady to emphasize the radiological findings of such a benign breast condition and increase awareness.
Case Presentation
The patient is a 43-year-old single Saudi woman who presented with a hard right, painless breast lump persisting for four months without any skin changes or nipple discharge. She is a documented instance of chronic type I insulin-dependent DM, having received treatment for the past 27 years. She is also afflicted with obesity, possessing a BMI of 35.9. No more autoimmune diseases were documented.
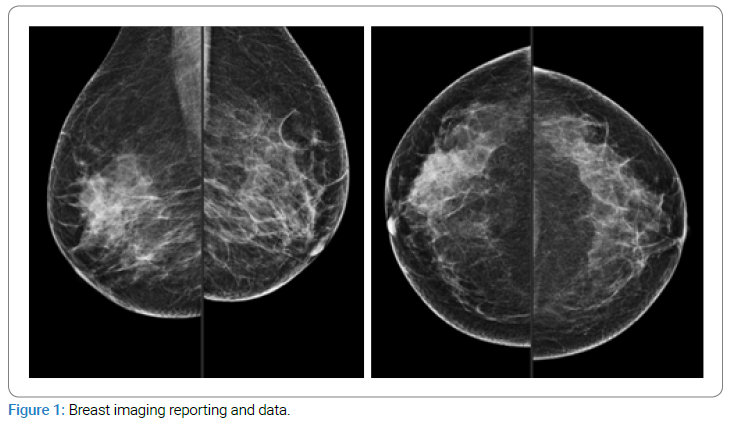
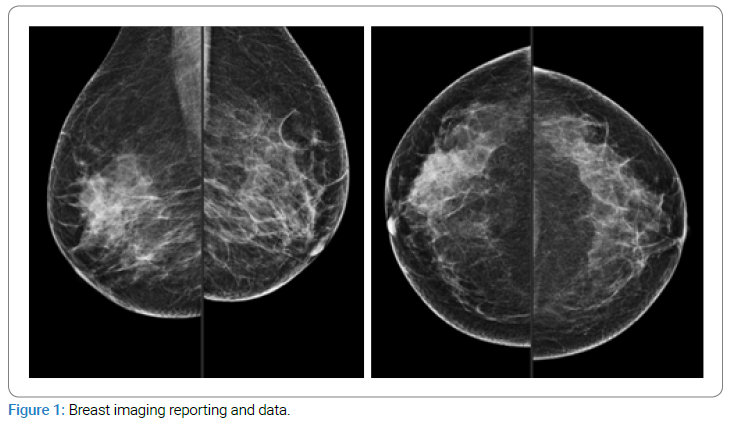
Mammography revealed a dense breast with focal asymmetry in the right outer upper breast with no suspicious microcalcification; BI-RADS 0 (Figure 1) for further investigation by additional views.
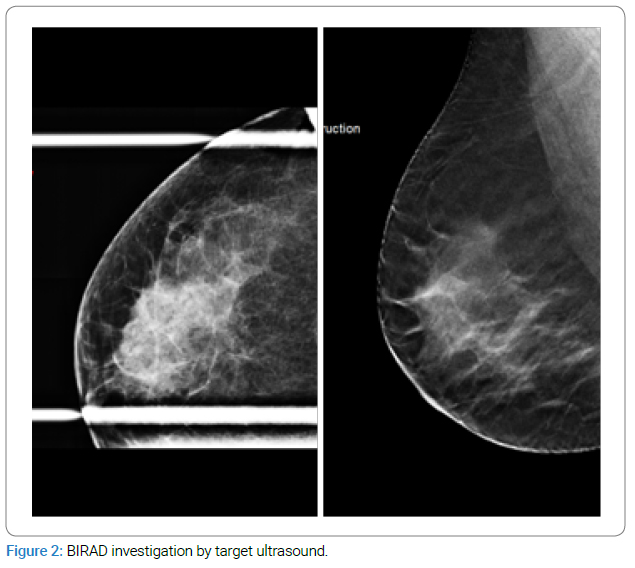
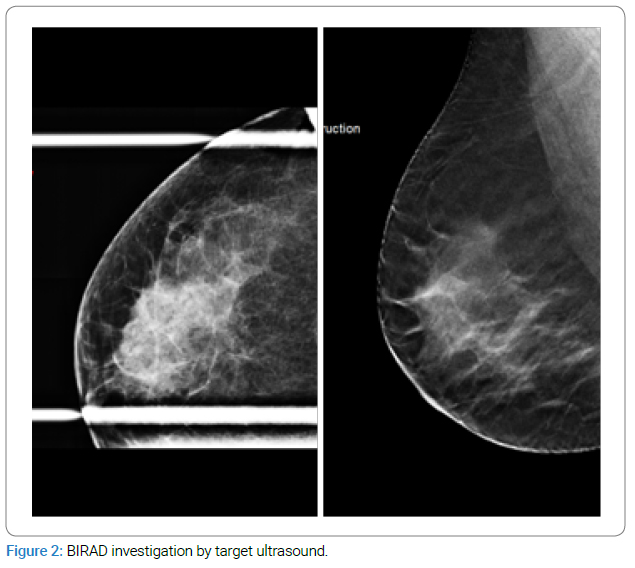
Additional tomosynthesis view revealed a partially obscured and speculated mass in the right outer upper breast associated with mild parenchymal distortion, no suspicious microcalcification or skin thickening. BIRAD 0 (Figure 2) for further investigation by target ultrasound.
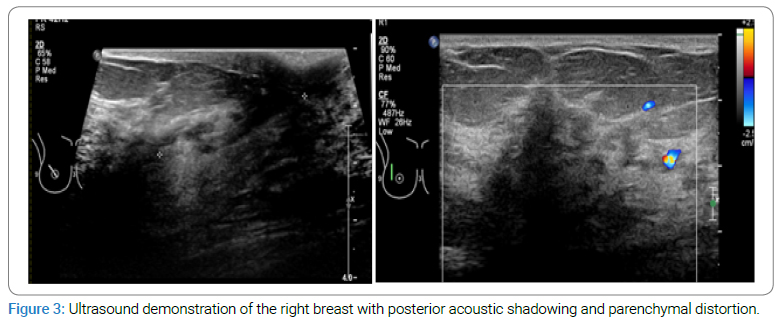
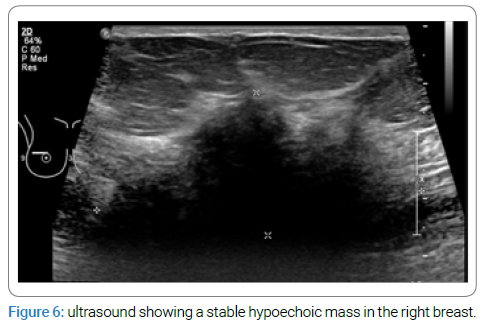
Ultrasound demonstrated a hypoechoic ill-defined mass in the 10 o’clock position of the right breast with posterior acoustic shadowing and parenchymal distortion, measuring around 4.8 cm x 2.1 cm. No lymphadenopathy (Figure 3). BI-RADS categorization was suspicious breast mass (BIRAD IV). Hence, a true cut biopsy was needed.
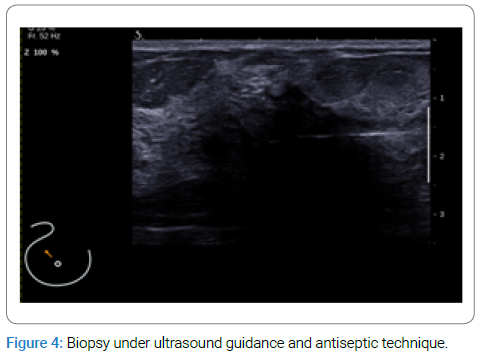
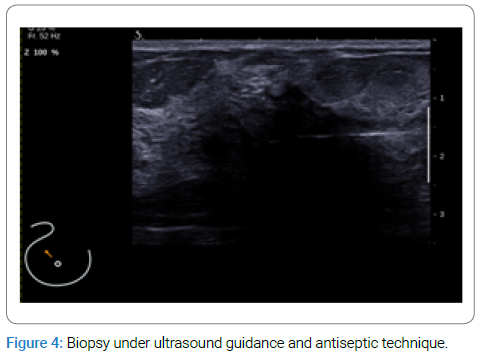
A true cut biopsy was performed under ultrasound guidance and antiseptic technique with no immediate complication (Figure 4).
The gross pathology of the excision specimen consists of three pieces of soft white core tissue measuring the largest 1.6 cm x 0.2 cm x 0.2 cm and the smallest measuring 1.2 cm x 0.2 cm x 0.2 cm. Histologically, the lesion showed predominantly stromal fibrosis/elastosis with periductal chronic inflammation and reactive atypia. Findings are consistent with DMP.
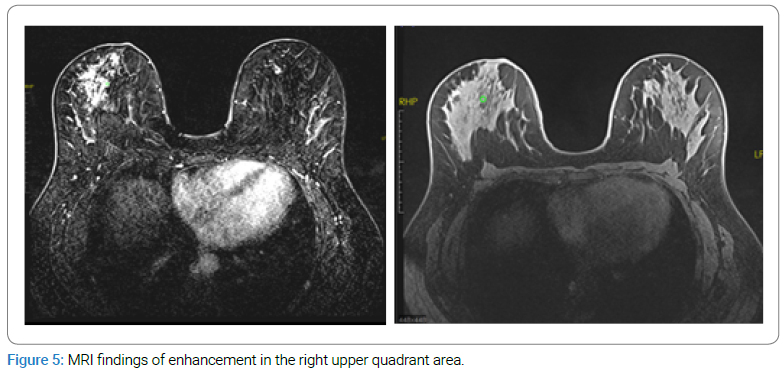
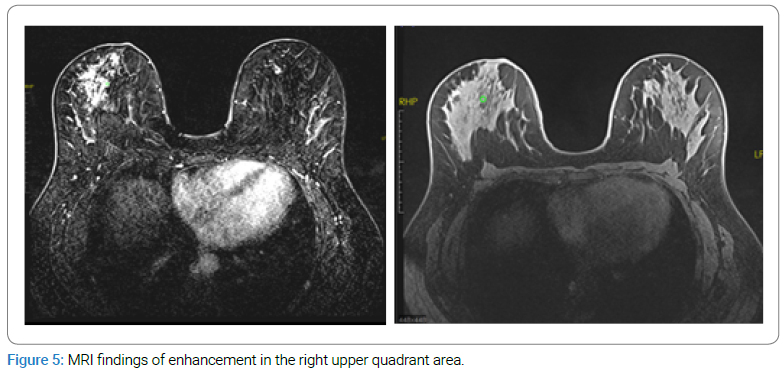
One month later, the MRI showed a non-mass-like enhancement in the right upper quadrant area, which was not associated with parenchymal distortion, and there were no suspicious MRI findings (Figure 5).
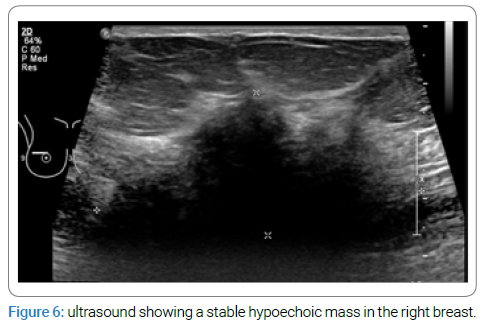
After almost 6 months, a follow-up ultrasound showed a stable hypoechoic mass in the right breast at the 10” o clock position with no new focal breast mass or abnormal acoustic shadowing (Figure 6).
The patient currently remains well and is on follow-up.
Discussion
DMP is an unusual benign breast disease, and it affects long-term insulin-dependent diabetic patients, like in our case. Our patient is known for long-standing type I insulin-dependent diabetes mellitus and has been treated for the last 27 years.
Andrews-Tang D et al. reported that patients who have type I diabetes tend to develop hard breast masses, which mimic cancer [6].
Longman and Hoffman established diagnostic criteria for DMP, stating that DMP should include three conditions: long-standing insulin-dependent diabetes mellitus, painless, hard and irregular breast mass, and some radiographic features such as dense tissue on a mammogram and acoustic shadowing behind the lesion in ultrasound. Our case met all these conditions [7].
Studies showed that most DMPs occur in the upper lateral breast area. Our case is consistent with the literature [11].
The radiographic features observed in our study were nonspecific and demonstrated a hypoechoic ill-defined mass with posterior acoustic shadowing and parenchymal distortion. A comparable study also found that DMP is a challenge for doctors, and further studies are needed to emphasize the diagnosis [5].
The ultrasound findings range between significant acoustic shadowing and questionable hypoechoic areas with no shadowing [6].
In consequence, a core-needle biopsy is still essential for a precise diagnosis [5]. On the other hand, one of the earliest studies of DMP also reported the radiological findings of DMP in 36 patients with type I DM and emphasized some useful imaging findings, like radiodense glandular tissue and significant acoustic shadowing in ultrasound [7].
A study involving 19 female patients reported findings consistent with those related to mammography in cases of heterogeneously dense or extremely dense breasts. A limited number of patients exhibited abnormal findings on mammography, with all identified asymmetry-related abnormalities. All lesions exhibited no distortions or concerning micro-calcifications on the mammogram. The ultrasound findings of DMP revealed an irregular shape, indistinct margin, heterogeneous echo-genicity, posterior acoustic shadowing, and parallel orientation. According to the United States findings, most patients were categorized as BI-RADS category IV [4].
DMP does not elevate the risk of breast cancer. The condition is not associated with malignancy [8–10], which aligns with our case and has been monitored for years with stable findings.
There is no definite treatment in the management of DMP; however, patient education and screening are important to relieve their fear of breast cancer [11].
Surgical excision is an option. However, recurrence of DMP after surgical excision has been reported [8], and re-excision after recurrence must be avoided [13]. Our patient didn’t undergo any surgery.
Conclusion
The uncommonness of DMP makes an accurate diagnosis challenging. It can be a dilemma for the physicians and a source of anxiety for the patients, and since it is imaging features mimic breast cancer, a tissue biopsy and a careful correlation of the patient’s history, physical examination with the radiology and histology results are required to establish a diagnosis. Patients and their physicians must be informed that DMP can recur even after resection, and any new breast masses must be evaluated completely to exclude malignancy.
Acknowledgment
The authors would like to thank the radiologists and staff of the Breast Imaging and Intervention department in KFMC for all the help and support.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Soler NG, Khardori R. Fibrous disease of the breast, thyroiditis, and cheiroarthropathy in type I diabetes mellitus. Lancet. 1984;1(8370):193–195.
- Dorokhova O, Fineberg S, Koenigsberg T, Wang Y. Diabetic mastopathy, a clinicopathological correlation of 34 cases. Pathol Int. 2012;62(10):660–664.
- Pereira MAQF, de Magalhaes AV, da Motta LDC, Santos AM, Segura MEA, Pereira CF, et al. Fibrous mastopathy: clinical, imaging, and histopathologic findings of 31 cases. J Obstet Gynaecol Res. 2010;36(2):326–335.
- Kim J, Kim EK, Kim MJ, Moon HJ, Yoon JH. Diabetic mastopathy: Imaging features and the role of image-guided biopsy in its diagnosis. Ultrasonography. 2015;35(2):140–147.
- Moschetta M, Telegrafo M, Triggiani V, Rella L, Cornacchia I, Serio G, et al. Diabetic mastopathy: a diagnostic challenge in breast sonography. J Clin Ultrasound. 2015;43(2):113–117.
- Andrews-Tang D, Diamond AB, Rogers L, Butler D. Diabetic mastopathy: adjunctive use of ultrasound and utility of core biopsy in diagnosis. Breast J. 2006;6(3):183–188.
- Logan WW, Hoffman NY. Diabetic fibrous breast disease. Radiology.1989;172(3):667–670.
- Camuto PM, Zetrenne E, Ponn T. Diabetic mastopathy: a report of 5 cases and a review of the literature. Arch Surg. 2000;135(10):1190–1193.
- Kudva YC, Reynolds C, O’Brien T, Powell C, Oberg AL, Crotty TB, et al. “Diabetic mastopathy,” or sclerosing lymphocytic lobulitis, is strongly associated with type 1 diabetes. Diabetes Care. 2002;25(1):121–126.
- Thorncroft K, Forsyth L, Desmond S, Audisio RA. The diagnosis and management of diabetic mastopathy. Breast J. 2007;13(6);607–613.
- Xiao XC, Shi JS, Hua W. Diabetic mastopathy in an elderly woman misdiagnosed as breast cancer: A case report and review of the literature. World J Clin Cases. 2021;9(14):3458–3465.
- Sankaye S, Kachewar S. Diabetic mastopathy. Australas Med J. 2012;5(6):296–299.
- Agochukwu NB, Wong L. Diabetic mastopathy: a systematic review of surgical management of a rare breast disease. Ann Plast Surg. 2017;78(4):471–475.
Keywords
Breast cancer; Breast imaging; Diabetes; Radiology; Ultrasound; Biopsy
Cite this article
Alshaia A, Almousa A. A rare condition resembling breast cancer: case report. Clin Case Rep J. 2025;6(1):1–5.
Copyright
© 2025 Alshaia A. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).