18-Year-Old Girl with Altered Sensorium and Brain Lesion
* A. Shobhana;
-
* A. Shobhana: Consultant In Critical Care, Stroke Medicine, Tropical Neurology, Institute of Neurosciences, Kolkata, India.
-
Apr 14, 2025 |
-
Volume: 6 |
-
Issue: 1 |
-
Views: 1394 |
-
Downloads: 1067 |
Abstract
CNS fungal infections are a rarity and difficult to diagnose. However, with the advancement of technology, fungal brain abscesses are being increasingly diagnosed, especially in immunocompetent patients. Moreover, radiologically, conglomerate abscesses, whether tubercular fungal or parasitic, may look alike. Hence, a multidisciplinary approach involving neurologists, infectious disease experts, neurosurgeons, microbiologists, radiologists, and pathologists increases the chances of a correct diagnosis and treatment. Dual infection of the brain with tuberculosis and fungus is once again very rare in people with no known immunosuppression, although such pulmonary infections are very well reported. We report a case of dual infection with tuberculosis and Cladophialophora species in a young girl with no known immunosuppressive disorder or therapy. An 18-year-old girl presented with headache-altered sensorium at the end of July 2016. She had had low-grade fever and occasional headaches for the last two months. Her initial work, including an MRI of the brain, revealed a large conglomerate ring-enhancing lesion in the left cerebellar hemisphere. She was started on a four-drug antitubercular regime as tuberculosis seemed to be the most common infection epidemiologically. However, she deteriorated and developed hydrocephalus. After a temporary external ventricular drain, she underwent craniotomy and biopsy of the lesion. It grew fungus of the Cladophialophora species and later Mycobacterium tuberculosis, which was resistant to pyrazinamide. She is doing well on the modified antitubercular and antifungal regimes. This is a rare case of dual infection with Mycobacterium and Cladophialophora. Cladophialophora infections are difficult to treat and are associated with significant mortality and recurrence. She is back to normal life after extensive therapy and has been on regular follow-ups for all these years.
Introduction
Cerebral phaeohyphomycosis is very well known. Cladophialophora is one of the most common organisms causing this condition. This case is rare because of dual infection by Mycobacterium tuberculosis and fungus of Cladophialophora species with no known immunosuppression. However, dual pulmonary infections with tuberculosis and fungi are well known. As far as our search goes, such dual infections in the brain have rarely been identified and reported. Hence, we report this case for its rarity as well as a learning curve to demonstrate the need for confirmatory histopathological and microbiological diagnosis, which again involves a multidisciplinary approach to its management.
Case Presentation
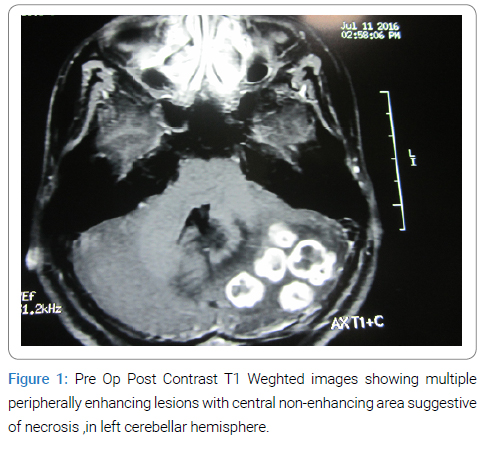
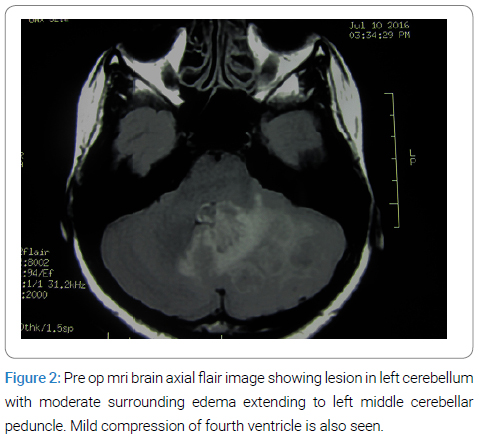
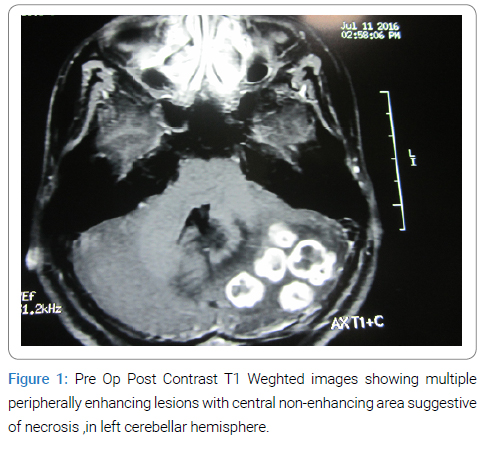
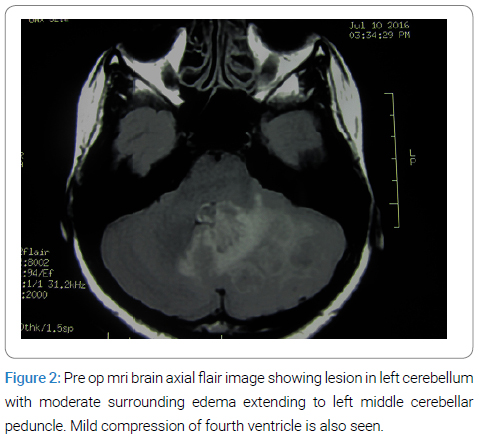
NT, an 18-year-old girl, presented with a headache and altered sensorium on 20th July 2016. She had had low-grade fever and occasional headaches for the last two months. She also complained of vertigo, loss of appetite, and weight loss. In her home town, an MRI of her brain was done (Figure 1,Figure 2), and she was started on four drug antitubercular (ATT) regimes as per Indian guidelines (Rifampicin, Isoniazid, Ethambutol, Pyrazinamide, i.e., RHEZ).
On admission to our hospital, she was a bit drowsy but arousable and obeyed commands. Whether it was only tuberculoma or any other etiology was uppermost in mind. Her initial investigations included a CT Scan of the brain and CECT of the thorax and abdomen. The serology for HIV was negative.
CT Scan of the brain revealed hydrocephalus.
CECT thorax revealed mediastinal lymphadenopathy and “tree in bud” opacities in the right upper and middle lobe along with both lower lobes.
CT Abdomen- enlarged peri-portal and peri-pancreatic lymph nodes.
Ancillary history: This girl had been suffering from some itchy skin lesions, and her serum IgE was 1486 IU/ L in March 2016, a few months prior to the current hospitalization. A dermatologist had treated her.
At Our Hospital: An External Ventricular Drain (EVD) was inserted on July 21, 2016. Since the posterior fossa lesion caused a significant mass effect, a decompressive craniotomy and excision of Mass in total were performed on the same day. The sensorium improved remarkably after this.
Cerebrospinal fluid analysis from EVD: 2 cells, all lymphocytes. Glucose-80 mg/dl (CBG-114 mg/dl), Protein-34 mg/dl, ADA- 5.9 U/L. Gram stain, AFB stain–negative. MTB Gene pert RIF- negative.
A repeat CT head showed a decrease in the size of the ventricles. EVD was removed on July 26, 2016. Meanwhile, ATD (RHEZ) was continued along with i.v. Inj. Dexamethasone. On July 29, her serum Alanin transaminase (ALT) rose to 191 IU/L; hence, her ATT was modified to Inj. Streptomycin, Ethambutol, and Moxifloxacin.
Further course: She was continued on modified ATT and steroids. She had a generalized tonic-clonic seizure later, and levetiracetam was added.
She was discharged from the hospital on 01.08.2016 on this regime, along with oral dexamethasone.
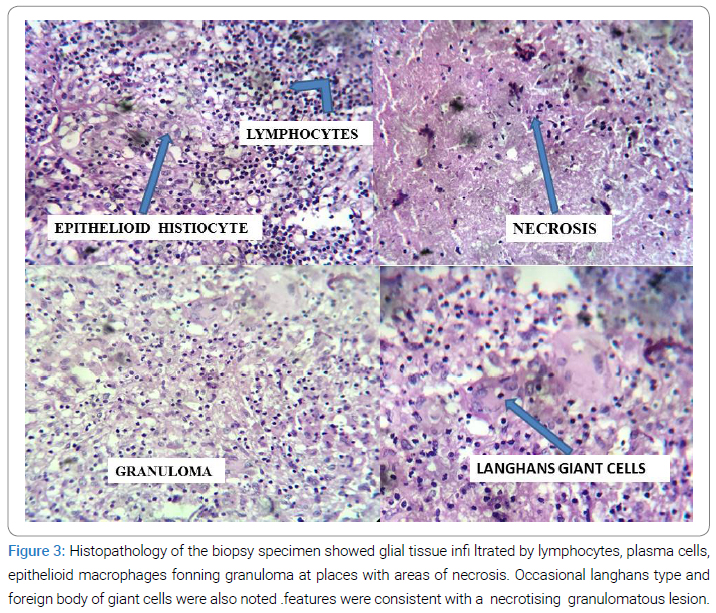
Pathological Diagnosis
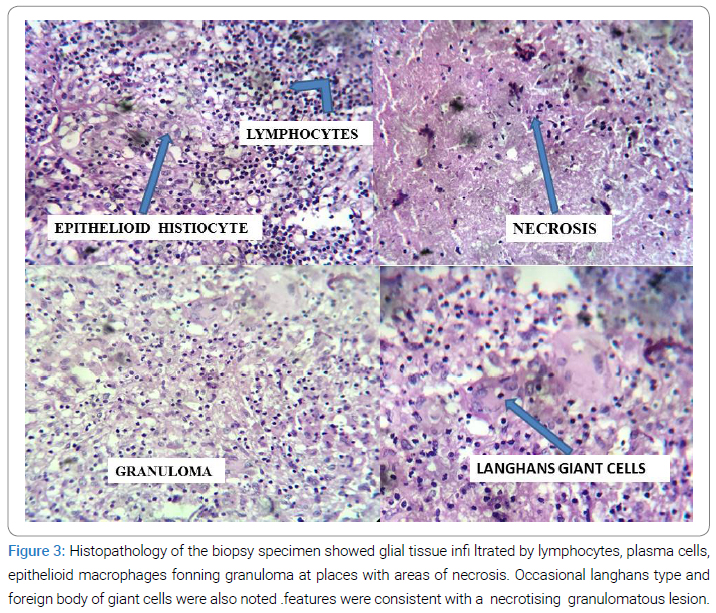
Histopathology of the biopsy specimen (Figure 3) showed glial tissue infiltrated by lymphocytes, plasma cells, and epithelioid macrophages forming granuloma at places with areas of necrosis. Occasional Langhans type and foreign body of giant cells were also noted. Features were consistent with a necrotizing granulomatous lesion.
Microbiological Diagnosis
Tissue Smear: The smear was negative for AFB on the ZN stain, and no fungal elements were seen on the KOH preparation. Gene pert RIF was negative.
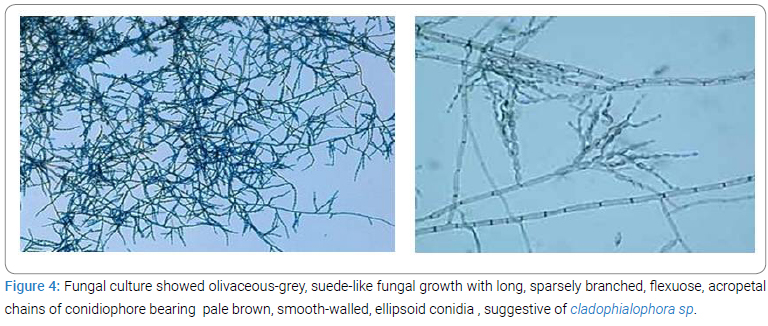
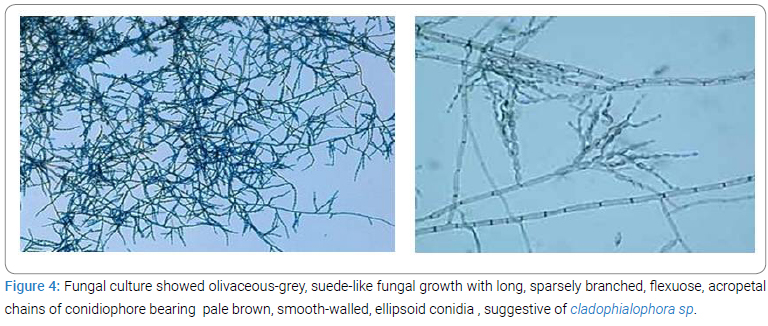
Culture: Fungal culture (Figure 4) on Sabourad’s Dextrose Agar grew within two weeks olivaceous-grey, suede-like fungal growth with long, sparsely branched, flexuose, acropetal chains of conidiophore bearing pale brown, smooth-walled, ellipsoid conidia, suggestive of Cladophialophora sp.
Meanwhile, an AFB culture was awaited. At three weeks, it grew AFB of the Mycobacterium tuberculosis complex. Drug susceptibility testing for five drugs was done, which revealed resistance to only pyrazinamide.
Final Diagnosis
Cladophialophora brain abscess in an individual with disseminated tuberculosis involving CNS, abdomen, and lung in a young girl with no known immunosuppression.
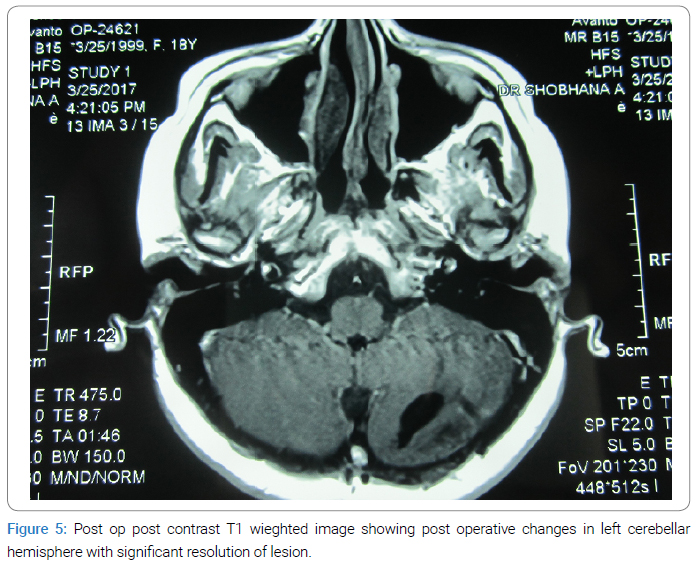
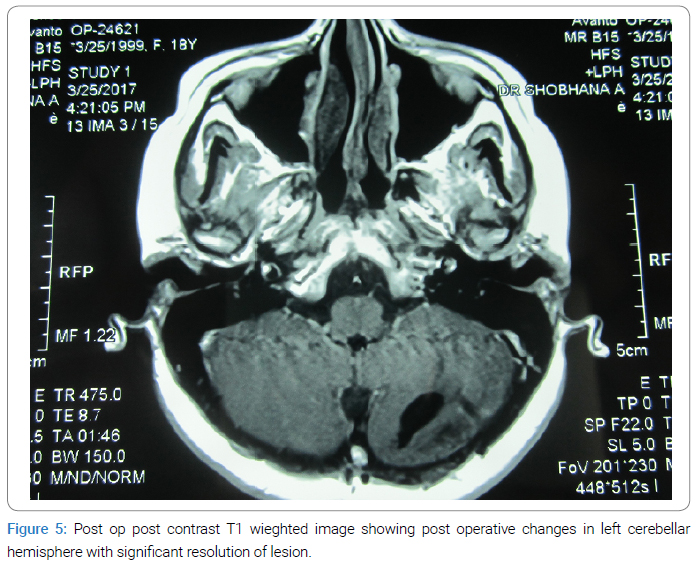
Follow-up: After her culture reports, she was started on oral voriconazole (loading 12 mg/kg stat followed by 6 mg/kg). In mid-August 2016 and continued till the end of April 2017. Rifampicin and isoniazide were added. Ethambutol was stopped in August 2016 due to visual blurring, which subsequently improved. Steroids were tapered and stopped in October 2016. A repeat MRI of the Brain with contrast in March 2017 (Figure 5) revealed gliosis and encephalomalacia in the inferior aspect of the left cerebellar hemisphere. Moxifloxacin was stopped in June 2017. The maintenance phase of ATT was continued with RH to complete eighteen months of total therapy. She is doing well in her studies and has been on regular follow up for the last eight years.
Discussion
CNS fungal infections are being more often diagnosed nowadays, thanks to the availability of better diagnostic facilities. Dual infections with mycobacteria and fungi are rare.
Fungus of Cladophialophora species are the commonest cause of non-traumatic CNS infection, namely cerebral phaeohyphomycosis, with their ability to cause infection in immunocompetent young hosts [1,2]. Mortality is as high as 70%, even in treated cases [1–3]. Primarily, it affects the lung and is hematogenous disseminated to the CNS as it is a highly neurotropic fungus [1]. Skin infections are rare due to traumatic inoculation [1]. These fungi can cause serious disease in immunocompetent as well as immunocompromised hosts. In most series, CNS phaeohyphomycosis was not associated with any underlying immune deficiency. Immune dysfunction was seen in only 37% of subjects in a series, mostly related to neutropenia or hematological malignancies [1–3]. This patient’s skin infection and high serum IgE levels may be coincidental. A local dermatologist saw her; she had no lesions when she presented to us. Apart from CNS tuberculosis, which itself is an immune-suppressed state, any other cause of immunosuppression, namely malignancies or HIV infection, was ruled out.
CNS lesions may present as well-defined abscesses such as cerebritis with necrotic lesions or meningitis, encephalitis, or myelitis [1–3]. Diagnosis is difficult, and a multidisciplinary approach involving neurosurgeons, microbiologists, and infectious disease experts is necessary to clinch it [4]. Radiologically, fungal brain abscesses cannot be distinguished from bacterial abscesses, primary brain tumors, and metastasis [2,4]. That histopathological and microbiological examinations, including studies for bacteria, mycobacteria, and fungi, are mandatory in evolving intracerebral mass lesions needs no emphasis, as exemplified by our patient, who ultimately was found to have dual infection. The growth of unusual fungi should not be routinely considered contaminants [2]. The infection provokes a granulomatous reaction containing giant cells [1]. Complete excision of the lesion along with antifungals helps in good recovery [1–5]. This was precisely done in our patient. The choice of antifungals is varied [1–4]. Voriconazole is fungicidal with good oral bioavailability and adequate CNS penetration [1–4]. The duration of therapy is uncertain, although few studies recommend it for the radiological resolution of lesions [1]. We got a complete radiological resolution of the lesion and then stopped Voriconazole. However, these patients require long-term follow-up for relapse, which we will be doing.
As far as treating extrapulmonary tuberculosis is concerned, it has to be patient-centered, and where accessible, a tissue-based diagnosis is recommended [6]. Pyrazinamide mono resistance has also been described [7]. Pyrazinamide (PZA) is an important anti-tuberculosis drug, active against dormant and slow-growing bacilli, and used as a component of first-line drugs and drug-resistant tuberculosis regimens. Its inclusion has decreased the duration of TB treatment [8]. Prior TB treatment could be a risk for its resistance prevalence of this resistance is 6.95% and 8.77%, respectively, among new and previously treated TB patients in India [9]. Pyrazinamide is a prodrug which is converted to an active form. It acts on various sites and is bactericidal [10]. Mutations in pncA and its promoter region are the main cause of PZA resistance. However, this may not be found in all PZA-resistant cases; there could also be other mechanisms. Resistance to PZA may portend unfavorable outcomes, especially in retreatment cases. Treatment with Isoniazid, Rifampicin, and Ethambutol for a longer duration or the addition of other susceptible drugs is usually practiced. In the developing world, drug susceptibility testing is the main challenge. Our patient had no history of TB treatment before this episode. Moxifloxacin, which was sensitive, was added instead of Pyrazinamide. She responded well and is now back to normal life.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Ajantha GS, Kulkarni RD. Cladophialophorabantiana, the Neurotropic Fungus – A Mini Review. J Clin of Diagn Res. 5(6):1301–1306.
- Revankar SG, Sutton DA, Rinald MG. Primary central nervous system phaeohyphomycosis: a review of 101 Cases. Clin Infect Dis. 2004;38(2):206–216.
- Huang WM, Fan YM, Li W, Yang WW. Brain abscess caused by Cladophialophorabantiana in China. J Med Microbiol. 2011;60(Pt 12):1872–1874.
- Garzon C, Markham L, Bijlenga P, Garbino J. Cladophialophorabantiana: a rare cause of fungal brain abscess. Clinical aspects and new therapeutic options. Med Mycol. 2008;46(5):481–486.
- Raut A, Mazumdar D, Nalnwar R, Nagar A, Ahmed N, Hira P. Cerebral Abscess Caused By Cladosporiumbantianum infection. Naturol Med Chir (Tokyo). 2003; 43: 413-415.
- Sharma SK, Ryan H, Khaparde S, Sachdeva KS, Singh AD, Mohan A, et al. Index-Tb Guidelines - Guidelines on extra-pulmonary tuberculosis for India. Indian J Med Res. 2017;145(4):448–463.
- Kurbatova EV, Cavanaugh JS, Dalton T, Click ES, Cegielski JP. Epidemiology of Pyrazinamide-Resistant Tuberculosis in the United States, 1999–2009. Clin Infect Dis. 2013;57(8):1081–1093.
- Balay G, Abdella K, Kebede W, Tadesse M , Bonsa Z, Mekonnen M, et al. Resistance to pyrazinamide in Mycobacterium tuberculosis complex isolates from previously treated tuberculosis cases in Southwestern Oromia, Ethiopia. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases. 2024; 34:100411.
- Mishra GP, Mulani JD. First National Anti-Tuberculosis Drug Resistance Survey (NDRS) from India- An Eye Opener. J Infectiology. 2018;1(2): 26–29.
- Zhang Y, Shi1 W, Zhang W, Mitchison D. Mechanisms of Pyrazinamide Action and Resistance. Microbiol Spectr. 2013;2(4):1–12.
Keywords
Brain Lesion; CNS fungal infections; Cladophialophora
Cite this article
Shobhana A. 18-year-old girl with altered sensorium and brain lesion. Clin Case Rep J. 2025;6(1):1–5.
Copyright
© 2025 A. Shobhana. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).