Rare Case of Achalasia in Pregnancy
* Eunjae Lee;
* Sharmeen Mian;
* Stephanie Langsam;
-
* Eunjae Lee: Department of Obstetrics and Gynecology, Lankenau Medical Center, Wynnewood, Pennsylvania, USA.
-
* Sharmeen Mian: Department of Obstetrics and Gynecology, Lankenau Medical Center, Wynnewood, Pennsylvania, USA.
-
* Stephanie Langsam: Department of Obstetrics and Gynecology, Lankenau Medical Center, Wynnewood, Pennsylvania, USA.
-
Apr 28, 2025 |
-
Volume: 6 |
-
Issue: 1 |
-
Views: 1374 |
-
Downloads: 1136 |
Abstract
Background: Achalasia, a rare esophageal motility disorder marked by impaired lower esophageal sphincter relaxation and absent peristalsis, presents unique challenges during pregnancy due to risks of dysphagia, aspiration, and nutritional deficiencies. This report highlights a case of achalasia diagnosed during pregnancy, along with an overview of its management and associated implications.
Case: The patient is a 36-year-old G3P2002 at 35 weeks gestation who presented with worsening shortness of breath, dysphagia, and a Globus sensation. CT imaging revealed a massively dilated esophagus with a significant amount of retained food throughout the entire esophagus. This resulted in a narrowing of the trachea, causing desaturation events. After multidisciplinary consultation, the patient had a successful awake fiber optic intubation and esophagogastroduodenoscopy with the removal of food debris. She was maintained on a clear liquid diet and was induced at 37 weeks. The patient had a successful vaginal delivery.
Conclusion: This case emphasizes the significance of recognizing and addressing achalasia during the third trimester of pregnancy. A collaborative, multidisciplinary approach is crucial for ensuring safe and effective management. Additional research is needed to define the best diagnostic and treatment strategies for this rare condition in pregnant patients.
Introduction
Achalasia, a potential cause of dysphagia, is an esophageal motility disorder resulting from the progressive degeneration of ganglion cells in the myenteric plexus of the esophageal wall.
This degeneration leads to impaired relaxation of the Lower Esophageal Sphincter (LES) and the loss of peristalsis in the distal esophagus [1]. In North America, the treated incidence and prevalence of achalasia are reported at 1.63 per 100,000 and 10.82 per 100,000, respectively.
Notably, achalasia affects males and females equally and can manifest at any age. While its incidence remains stable, prevalence has risen in recent years [2]. Although the precise etiology of achalasia is unclear, it has been associated with various conditions impacting esophageal motility, including cancer, Chagas disease, amyloidosis, sarcoidosis, neurofibromatosis, and eosinophilic esophagitis [1].
Patients with achalasia typically present with dysphagia, initially more pronounced with solids than liquids, and may also experience regurgitation. Its insidious onset often delays diagnosis by several years. Additional symptoms, such as chest pain, dyspnea, and malnutrition, are frequently misdiagnosed as Gastroesophageal Reflux Disease (GERD) [3]. In pregnancy, achalasia is rare but poses unique and complex management challenges requiring a multidisciplinary approach.
Case Presentation
We present the case of a 36-year-old G3P2002 patient who, at 35 weeks of gestation, presented to the emergency room with worsening dyspnea, dysphagia, and globus sensation, culminating in acute respiratory distress. Throughout her current and previous pregnancies, she reported symptoms of early satiety and emesis, accompanied by dyspnea that prompted a cardiological evaluation at 32 weeks. Imaging during this assessment suggested a complex echo density possibly indicative of an ahiatal hernia; however, further diagnostic workup was recommended with a CT scan, which was not done.
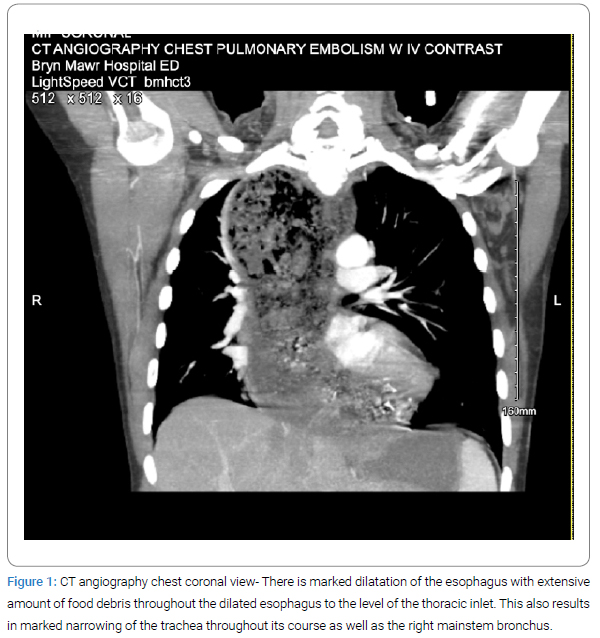
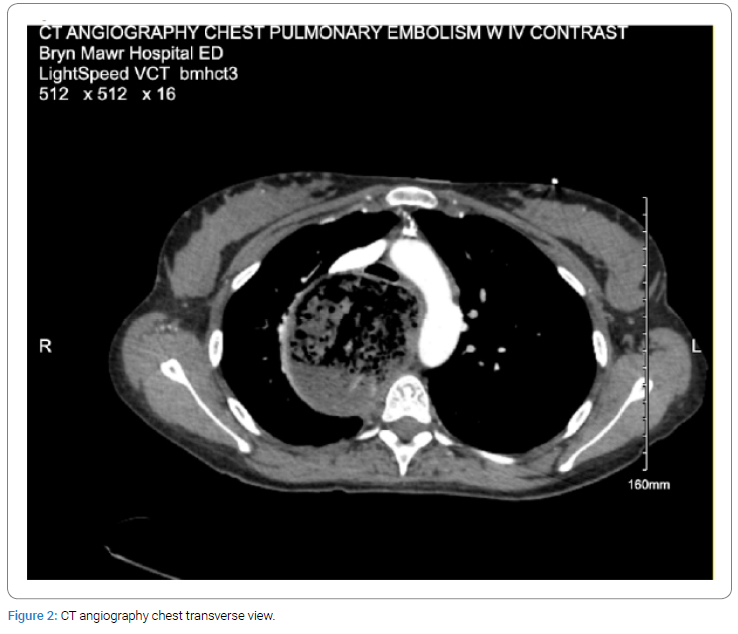
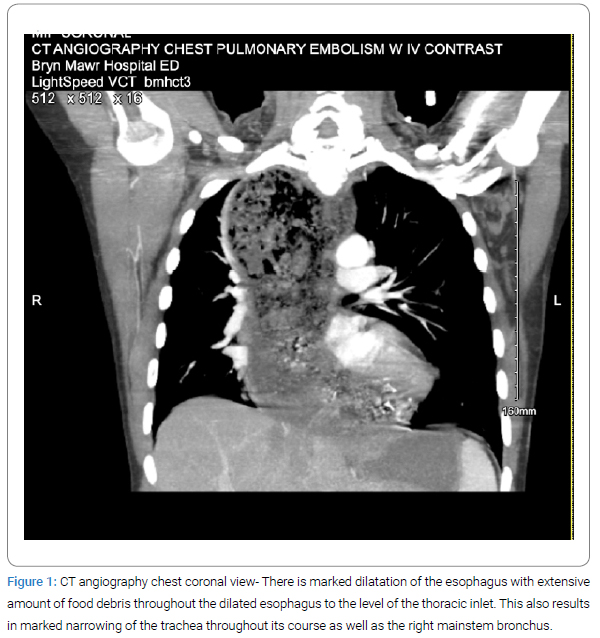
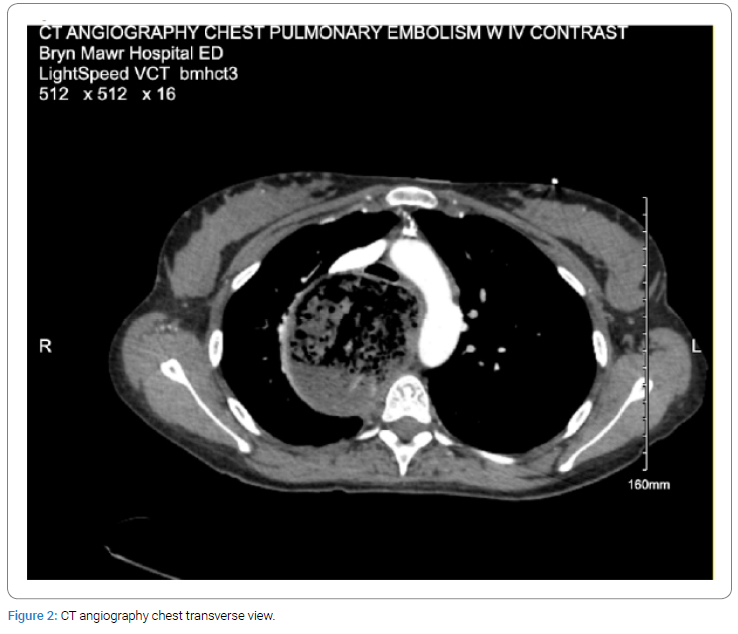
At presentation, the patient exhibited tachypnea and required supplemental oxygen to maintain normal oxygen levels. CT angiography revealed significant esophageal dilation with extensive food debris, leading to tracheal and bronchial compression—findings consistent with achalasia (Figure 1, Figure 2).
A multidisciplinary team, including thoracic and gastroenterology specialists, guided her management. Flexible bronchoscopy and endoscopy were performed, successfully clearing the food debris. After clearance of the food debris, the esophagus was diffusely floppy and dilated. The cardia and gastric fundus appeared normal on retroflexion; however, it was noted that the gastroesophageal junction was tight around the endoscope. No biopsies were taken during the procedure. She was discharged on a postoperative day 4 with recommendations to follow-up with an achalasia specialist with plans for manometry as an outpatient. Throughout this process, antenatal surveillance showed reactive non-stress tests and appropriate fetal growth on ultrasound.
After removing all food debris, the patient’s symptoms improved; however, she remained on a strict liquid diet. Following discussions with her provider, a plan was established for delivery at 37 weeks to facilitate gastroenterology follow-up and treatment initiation. She underwent induction at 37 weeks and had an uncomplicated vaginal delivery. Postpartum, she is recovering under the care of an achalasia specialist and has begun treatment with botulinum toxin (Botox) injections and, ultimately, peroral endoscopic myotomy.
Discussion and Conclusion
This case highlights the rarity of severe achalasia in late pregnancy and its potential fetomaternal complications, including Acute Respiratory Distress Syndrome (ARDS), aspiration pneumonia, maternal malnutrition, preterm delivery, fetal growth restriction, and even fetal demise [3].
Diagnosing achalasia during pregnancy is particularly challenging, as its early symptoms—such as regurgitation, heartburn, and nausea/vomiting—closely resemble common pregnancy-related discomforts caused by increased intra-abdominal pressure, diaphragmatic elevation and progesterone-induced smooth muscle relaxation. As a result, achalasia is often misdiagnosed as hyperemesis gravidarum, leading to delays in diagnosis and treatment [4].
Notably, the patient had experienced similar symptoms, including early satiety and emesis, during a previous pregnancy. However, the severity of her symptoms at that time remains unclear, and an earlier workup may have led to a more timely diagnosis. This case highlights the importance of considering esophageal disorders in pregnant patients with persistent, progressively worsening symptoms, as early recognition and intervention can significantly improve outcomes.
Effective management of achalasia in pregnancy requires a personalized, multidisciplinary approach involving obstetricians, maternal-fetal medicine specialists, thoracic surgeons, gastroenterologists, anesthesiologists, and neonatologists. This collaborative care model ensures optimal outcomes for both mother and baby, from tailored intrapartum management prioritizing maternal and fetal well-being to comprehensive postpartum follow-up for ongoing achalasia treatment [5].
Funding
This original work received no funding
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Spechler SJ, Pandolfino JE; UpToDate. Achalasia: Pathogenesis, clinical manifestations, and diagnosis [Internet].” UpToDate: Wolters Kluwer; 2024.
- Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22(9):e256–e261.
- Azahar ZA, Ab Rahim MF, Ahmad N, Ramli R. Achalasia in pregnancy. BMJ Case Reports CP. 2024;17(5):e257698.
- Vosko S, Cohen DL, Neeman O, Matalon S, Broide E, Shirin H. Achalasia during pregnancy: proposed management algorithm based on a thorough literature review. J Neurogastroenterol Motil. 2021;27(1):8–18.
- Hooft N, Schmidt ES, Bremner RM. Achalasia in pregnancy: botulinum toxin a injection of lower esophageal sphincter. Case Rep Surg. 2015;2015:328970.
Keywords
Achalasia; Pregnancy; Dysphagia; Esophageal motility disorders; Multidisciplinary management
Copyright
© 2025 Stephanie Langsam. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).