Abstract
Crossed aphasia in dextral refers to aphasia following a right hemispheric lesion in right-handed subjects. It is a rare diagnosis with a prevalence of less than 2%. We describe a rare case of a bilingual patient affected by global aphasia following a cerebral hemorrhage in the right hemisphere. This report hopes to raise more awareness of this rare phenomenon. Further research is warranted to understand the pathophysiology and prognosis of this condition.
Introduction
Aphasia is an impairment of language that usually occurs due to brain damage to the language-dominant cerebral hemisphere. It has an estimated 35% incidence in stroke patients [1]. Roughly 90% of the human population is right-hand dominant; of these individuals, up to 7.5% use the right hemisphere for language [2].
Crossed aphasia in dextral refers to aphasia following a right hemispheric lesion in right-handed subjects. It is a rare diagnosis with a prevalence of less than 2% [3] and was previously considered to be non-fluent.
However, it is increasingly accepted that all types of aphasic syndromes can be registered [4]. Numerous case reports have been published, but there are no clearly established diagnostic criteria yet. Purported criteria in the literature for diagnosis include right-handedness without familial history of left-handedness, right hemispheric lesion, structural integrity of left hemisphere, and absence of developmental brain damage [3,5].
To our knowledge, no report of this syndrome has been published locally in Singapore. We describe a rare case of a bilingual patient affected by global aphasia following a cerebral hemorrhage in the right hemisphere.
Case Presentation
Patient M was a 65-year-old Chinese lady who was functionally independent. Prior to the hemorrhagic stroke, she was working as a kitchen assistant and was living with her husband and adult son. She was right-handed and bilingual in English and Chinese. She had a past medical history of hypertension.
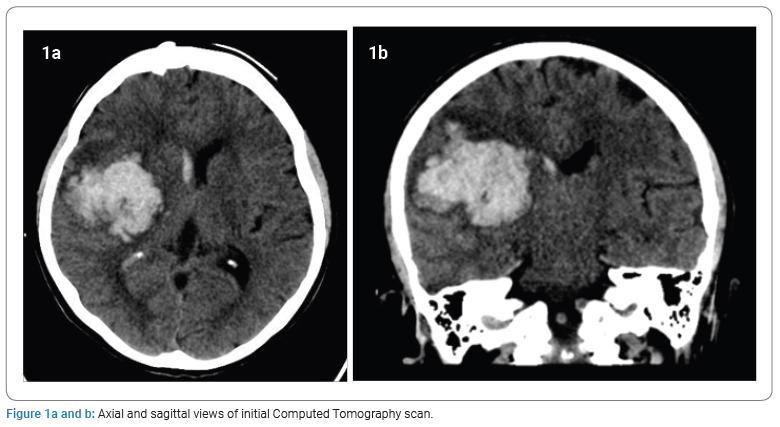
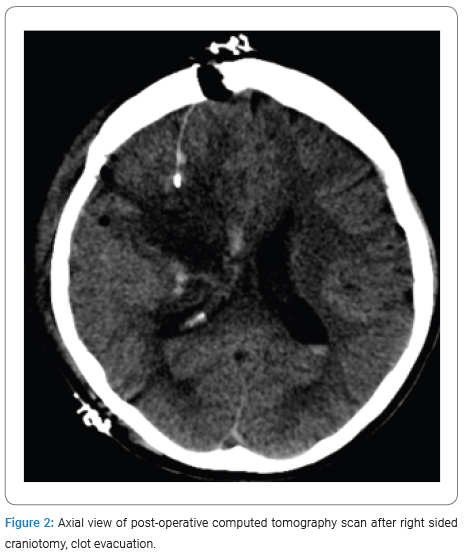
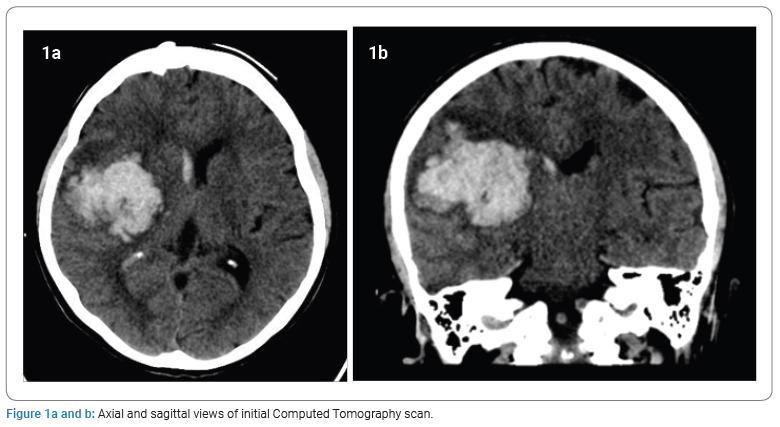
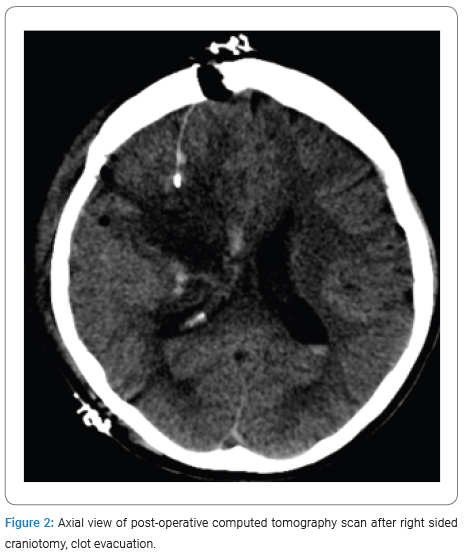
Stroke event and impairments: Patient M was admitted to the hospital for sudden onset of loss of consciousness at home. She was diagnosed with a stroke secondary to a large right external capsule and basal ganglia hemorrhage with extension to the right frontoparietal lobes, which necessitated craniotomy and evacuation of hemorrhage (Figure 1, Figure 2). Twelve days after the stroke, she was transferred to a rehabilitation center.
On initial assessment in the rehabilitation center, she had left upper and lower limb hemiparesis and, cognitive deficits of decreased arousal and attention span and left visuospatial neglect. Her communication was significantly impaired as she was diagnosed with global aphasia secondary to the hemorrhagic stroke. She was unable to follow one-step verbal commands consistently and had minimal verbal output.
Communication Assessment and Progress: Gradual improvements in her attention span and language were noticed over the first few weeks. On day 16, post-stroke, she started vocalizing, but her words were unintelligible. Her responses to yes/no questions by, nodding her head, as well as tasks of matching pictures to words, were inconsistent and unreliable.
At 1 month post-stroke, she was able to say her name and named bedside items correctly when prompted in both English and Mandarin. The speech was non-fluent and had elements of agrammatism, paraphrasing, and difficulty with persistent comprehension.
At 3 months post-stroke, an assessment was conducted in English. She was able to consistently follow 1 step verbal commands, answer yes/no questions, and name simple objects. On attempted picture descriptions obtained from the Western Aphasia Battery, there was reduced production with semantic paraphasia. Her speech was still non-fluent, and she only managed to produce one phrase.
Discussion
Our patient had significant right hemispheric involvement, and although we are unable to comment on precise localization for the crossed aphasia, we postulate that it may be linked to basal ganglia involvement. The basal ganglia may be responsible for grammar [6], and the lentiform nucleus [7] may act as essential components in neural mechanisms of language processing. Furthermore, it is increasingly well established that the right hemisphere may have a significant role in language processing, and impairments to speech comprehension may occur after damage to the right inferior frontal sulcus [8].
It is interesting to note that there are cited differences in recovery of different languages in bilingual patients. Lee et al. found that in their patient fluent in Korean and Japanese, there was more significant improvement in the Korean language over the Japanese language [9]. It remains to be seen if crossed aphasia has any significant associations with the improvement of a particular language. In unilingual Chinese patients, there was a higher incidence of crossed aphasia, which might be due to the nature of the Chinese language and its neural function [10]. Further comparisons of unilingual versus multilingual patients may be useful in evaluating if different languages may have differing recovery trajectories.
Patient M still had severe aphasia at 3 months, thereby suggesting that this phenomenon was chronic and not transient. More information on the prognosis and trajectory of crossed aphasia will be useful to further guide clinicians in managing this rare phenomenon.
Limitations
One limitation of our study is the lack of an assessment of left-handedness using a standardized assessment tool such as the Edinburgh Handedness Inventory. Our patient also did not have a comprehensive, objective measure of aphasia, such as the Western Aphasia Battery, as this was limited by her short attention span during her inpatient rehabilitation stay.
Conclusion
Crossed aphasia in dextral is a rare phenomenon that is still poorly understood. Further research is warranted to understand the pathophysiology and prognosis of this condition.
Conflict of Interest
Crossed aphasia in dextral is a rare phenomenon that is still poorly understood. Further research is warranted to understand the pathophysiology and prognosis of this condition.
Keywords
Stroke; Rehabilitation; Aphasia
Cite this article
Seah JD, Kong KH. Crossed Aphasia in a Bilingual Dextral: A Case Report. Clin Case Rep J. 2025;6(2):1–3.
Copyright
© 2025 Justin Desheng Seah. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).