Delayed Visual Sequelae and Hemodialysis Challenges in Severe Methanol Poisoning: A Case Report of Reconsumed Contaminated Chinese Baijiu
* Ting Zhao;
* Xinxin Wang;
* Liting Duan;
Ping Li;
* Saisai Sun;
Fengling Hao;
* Dongdong Wang;
-
* Ting Zhao: Department of Encephalopathy, Weifang Traditional Chinese Hospital, Shandong Second Medical University, Weifang 261041, China.
-
* Xinxin Wang: Department of Ophthalmology, Affiliated Hospital of Shandong Second Medical University, Weifang 261031, China.
-
* Liting Duan: Department of Encephalopathy, Weifang Traditional Chinese Hospital, Shandong Second Medical University, Weifang 261041, China.
-
Ping Li: Department of Encephalopathy, Weifang Traditional Chinese Hospital, Shandong Second Medical University, Weifang 261041, China.
-
* Saisai Sun: Department of Emergency Surgery, Weifang Traditional Chinese Hospital, Shandong Second Medical University, Weifang 261041, China.
-
Fengling Hao: Department of Encephalopathy, Weifang Traditional Chinese Hospital, Shandong Second Medical University, Weifang 261041, China.
-
* Dongdong Wang: Department of Encephalopathy, Weifang Traditional Chinese Hospital, Shandong Second Medical University, Weifang 261041, China.
-
Jun 20, 2025 |
-
Volume: 6 |
-
Issue: 2 |
-
Views: 6884 |
-
Downloads: 2650 |
Abstract
Methanol toxicity arises from metabolites (formaldehyde/formic acid), causing blindness, coma, or death. Severity correlates with formic acid accumulation, with symptoms delayed up to 72 hours–96 hours if ethanol is co-ingested. Diagnosis relies on elevated anion gap metabolic acidosis, altered mental status, and visual impairment. A 55-year-old man consumed 500 mL–600 mL of Chinese Baijiu (a colorless Chinese distilled wine with grain as the main raw material) from a jug opened 3 years prior. He presented with dizziness and metabolic acidosis (pH 7.09, anion gap 27.1 mmol/L), unresponsive to bicarbonate. Hemodialysis normalized acidosis, but irreversible bilateral vision loss and optic neuropathy occurred. Brain CT revealed occipital/frontal hypodense lesions. Despite 66 hours of intermittent hemodialysis, visual deficits persisted, underscoring methanol’s neurotoxic potential and the critical need for early intervention to prevent permanent damage.
Introduction
Methanol itself is non-toxic, but its metabolites (formaldehyde and formic acid) exhibit high toxicity, potentially leading to blindness, coma, metabolic disturbances, and even death [1]. The severity of poisoning primarily depends on formic acid accumulation. Clinical symptoms typically manifest within 6 hours–24 hours but may be delayed up to 72 hours–96 hours when ethanol is co-ingested [2]. Methanol’s toxic dose varies significantly, particularly with concurrent ethanol consumption. The diagnostic triad of methanol poisoning includes metabolic acidosis with an elevated anion gap, acute mental status changes, and visual impairment [3]. Despite advancements in treatment, delayed diagnosis, and late hospital admission contribute to its high mortality [1], and survivors often experience permanent vision loss [4]. We present a rare case of severe methanol poisoning from re-consuming a previously opened jug of Chinese Baijiu (CB), highlighting delayed recognition despite active hemodialysis and incomplete visual recovery [5].
Case Presentation
A 55-year-old man presented with 14 hours of dizziness, drowsiness, and nausea. Initial brain Computed Tomography (CT) or Magnetic Resonance Image (MRI) at 10 hours post-onset showed no abnormalities. Notably, he had consumed 500 mL–600 mL of CB from a plastic jug 25 hours before symptom onset. The same jug had been opened and shared by ≥2 individuals 3 years prior without adverse effects. Vital signs were initially stable, but venous blood gas revealed critical metabolic acidosis (pH 7.09, PCO2 10 mmHg, HCO3- 3.2 mmol/L, anion gap 27.1 mmol/L). He had no other medical history to add. In addition, there were no obvious abnormalities in liver and kidney function, blood lipid analysis, urine routine, stool routine, coagulation routine, blood routine, and C-reactive protein. Despite 4 hours of sodium bicarbonate infusion and fluid resuscitation, acidosis persisted, prompting transfer to the intensive care unit for hemodialysis.
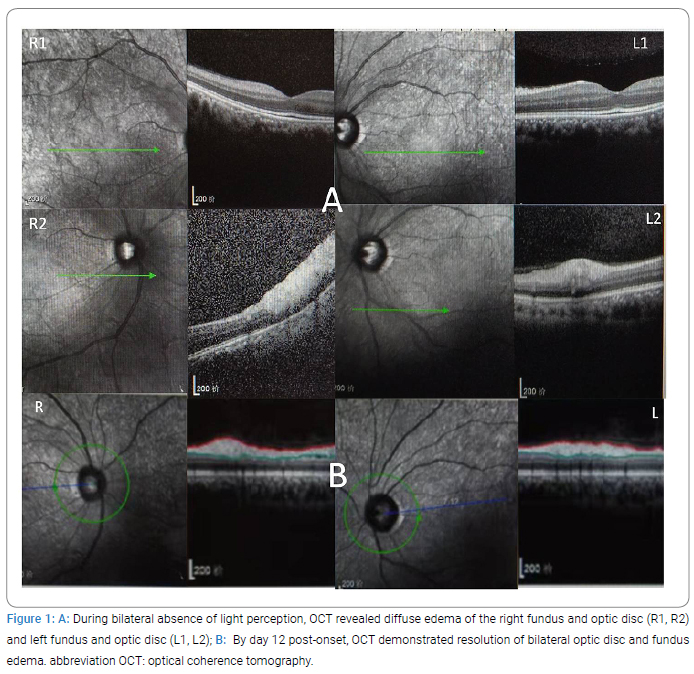
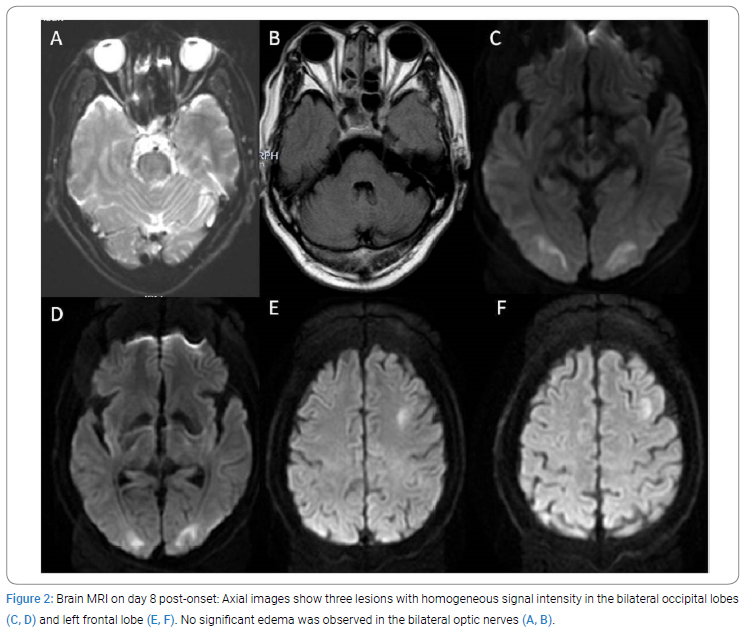
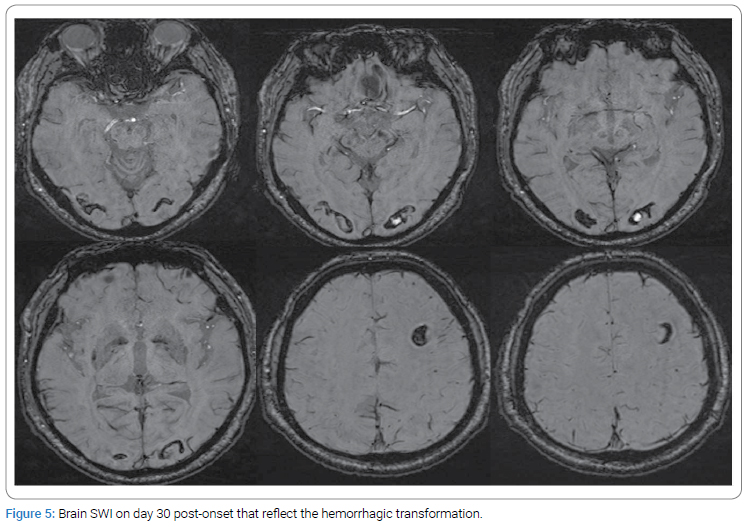
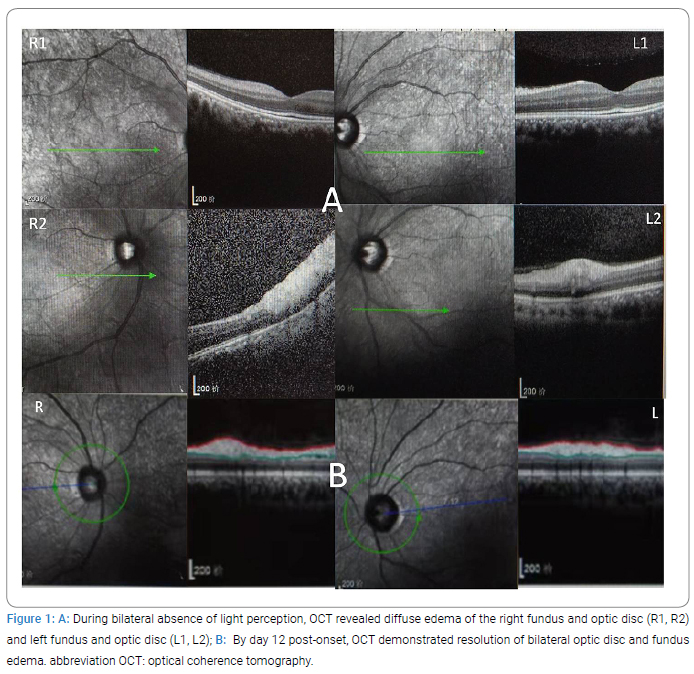
After 7 hours of hemodialysis, blood gas normalized, but bilateral vision loss (no light perception) and toxic optic neuropathy with disc swelling were observed (Figure 1A). Over 7 days, he received 66 hours of intermittent hemodialysis. Brain CT on day 3 revealed symmetric hypodense lesions in the occipital and left frontal lobes. By day 8, consciousness returned, with vision improving to counting fingers at 30 cm (right eye) and 50 cm (left eye); MRI showed resolving optic nerve edema (Figure 2).
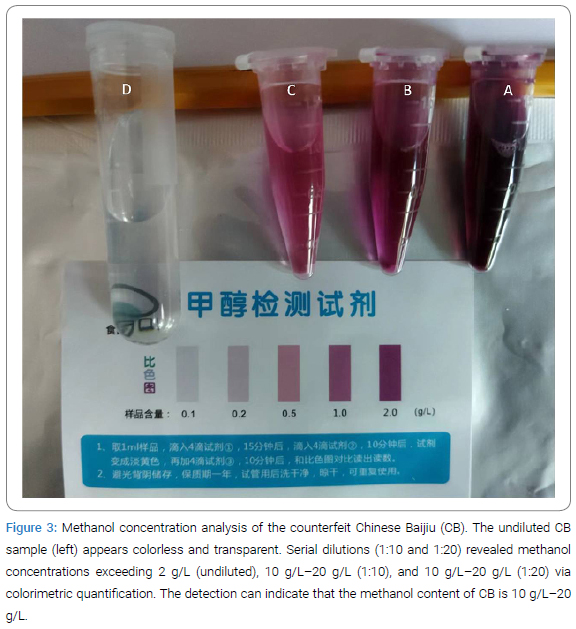
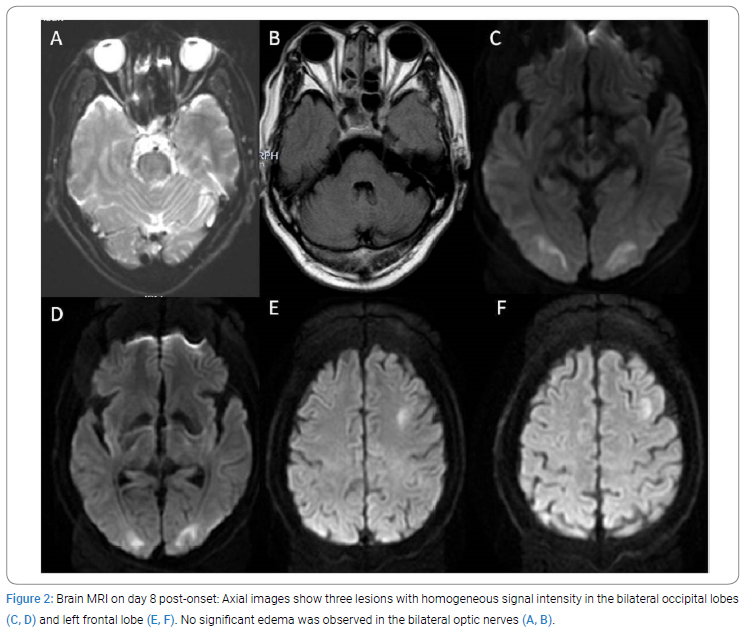
On day 12, optic disc swelling resolved (Figure 1B), but vision remained impaired. Suspecting methanol poisoning, we tested the residual CB using a household reagent, detecting methanol at 10 g/L–20 g/L (Figure 3). Treatment was adjusted to daily intramuscular mouse Nerve Growth Factor (NGF) (20 µg), weekly intravenous mecobalamin (0.5 mg), and oral thiamine (20 mg three times per day) for 21 days. Folate was omitted due to prolonged hemodialysis-induced formate clearance.
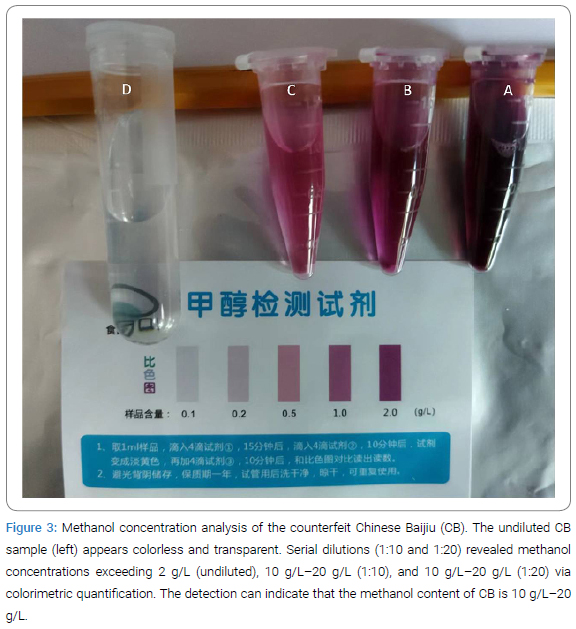
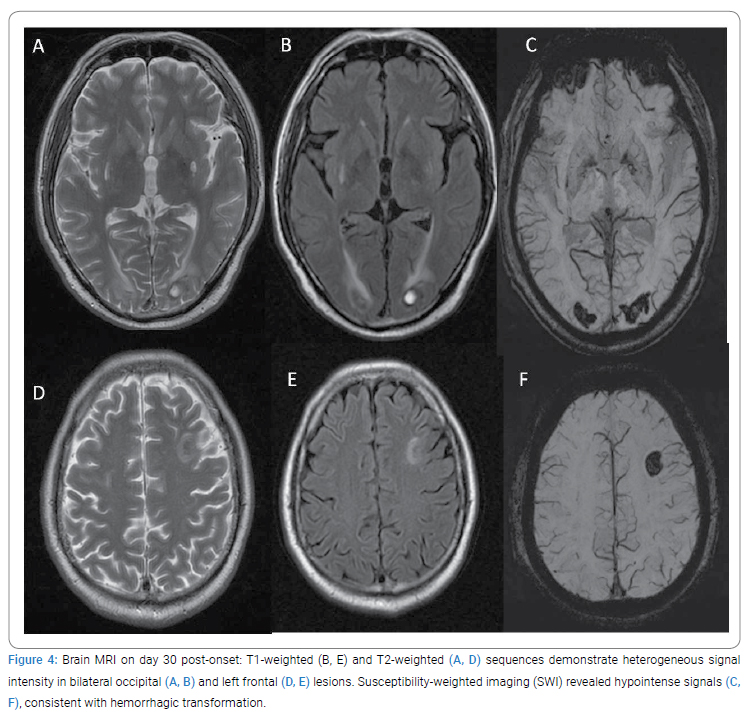
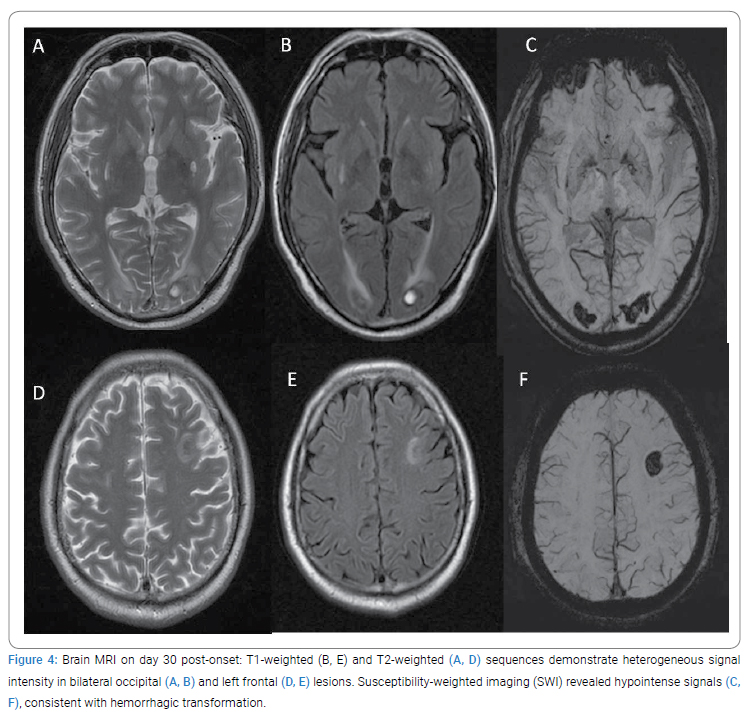
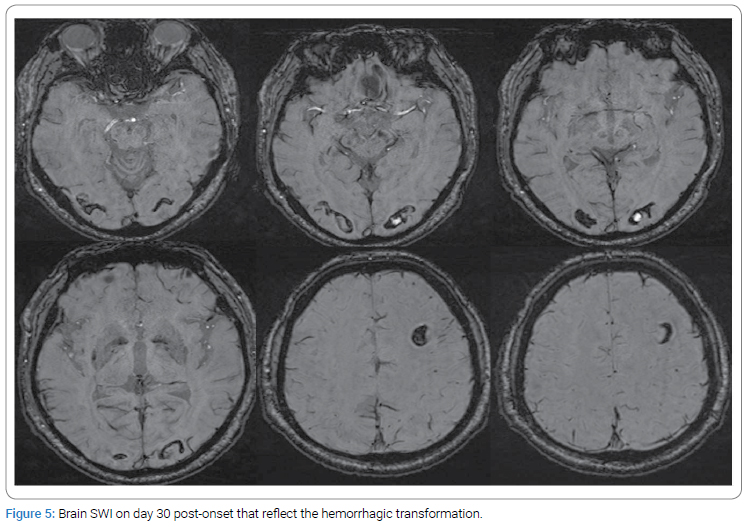
By day 28, he was discharged with hemorrhagic transformations on MRI (Figure 4, Figure 5), and he was able to recognize faces at 3 meters. One month post-discharge, he regained smartphone use capability. At a 6-month follow-up, he navigated stairs independently despite persistent visual fatigue and abstained from alcohol.
Discussion`
Oral ingestion is the primary route of methanol poisoning, which can lead to severe organ dysfunction or death [1,6]. A history of consuming methanol-containing beverages serves as a critical diagnostic clue. Due to methanol’s toxicity, symptoms often manifest shortly after initial exposure. In this case, the patient initially ingested about 1 g–2 g methanol, which was below the toxic threshold. However, the subsequent 5 g–10 g methanol intake reached a toxic, explaining the observed clinical progression.
The absence of symptoms in other individuals who consumed smaller quantities of the same CB initially prompted consideration of alternative diagnoses, such as acute ethanol intoxication, pancreatitis, or metabolic acidosis. While clinical suspicion favored methanol poisoning, local limitations precluded direct measurement of methanol or formate levels. Definitive confirmation was achieved through analysis of the remaining CB using the colorimetric method with a commercially available household methanol test kit: Methanol is oxidized to formaldehyde in an acidic potassium permanganate solution, followed by a reaction with chromotropic acid to form a purple compound. The kit demonstrated shelf stability of 1 year under recommended cool and dark conditions, enabling direct sample analysis within 35 minutes without requiring specialized equipment. In contrast, our optimized sample dilution assay achieves enhanced sensitivity and analytical reliability. This enhanced protocol provides a practical first-line screening solution for potential methanol poisoning cases, potentially accelerating critical clinical decisions.
Previous studies have highlighted the key therapeutic priorities for methanol poisoning. Current guidelines recommend hemodialysis for severe acidosis (pH <7.15–7.25), methanol levels >16 mmol/L, deteriorating clinical status, visual impairment, or renal injury [4,7]. Dialysis should continue until methanol levels fall below 6 mmol/L –9 mmol/L. Clinical improvement (e.g., visual recovery) may guide cessation in settings lacking laboratory confirmation.
In this case, NGF for injection was administered to promote visual recovery, which has demonstrated efficacy in treating toxic peripheral neuropathy induced by n-hexane, particularly optic nerve injury. Despite the absence of clearly identified neurotoxic agents, adjunctive therapy with NGF resulted in rapid improvement of optic nerve dysfunction and significant visual restoration. The residual visual impairment was attributed primarily to lesions in the visual cortex. The patient’s initial pH was 7.09, with improved visual impairment, which was inconsistent with evidence correlating admission pH >7.2 with favorable visual outcomes [8]. While our findings suggest that NGF may be a viable therapeutic option for mitigating methanol-induced visual damage, further research is warranted to validate its efficacy.
The patient’s brain MRI revealed three distinct neuroimaging signatures of methanol toxicity: 1. Dynamic white matter involvement: Acute-phase DWI hyperintensity in the bilateral external capsules resolved completely by day 7 follow-up, accompanied by symmetric occipital subcortical infarctions and an isolated left frontal lesion. 2. Mild optic nerve edema with significantly reduced after hemodialysis. 3. Delayed hemorrhagic transformation: Characterized by SWI hypointensity cores, demonstrating temporal dissociation from hemodialysis. No credible correlation with hemodialysis was observed, as MRI on day 11 (3 days post-dialysis) showed unchanged hemorrhagic signals. Retrospective analysis of the day 30 MRI suggested hemorrhagic transformation likely occurred around day 23 (15 days post-dialysis). This spatiotemporal pattern contrasts with classical methanol complications [9,10]: Absence of bilateral persistent basal segment lesions—a hallmark of methanol toxicity [11,12], and no intraventricular hemorrhage.
These findings emphasize the need for heightened suspicion of methanol poisoning in unexplained high anion-gap acidosis, particularly with ocular symptoms, and advocate for early fomepizole administration alongside dialysis to mitigate irreversible damage, particularly when supported by recent reviews [5].
Finally, the CB was privately provided by a winery worker. It is hypothesized that the excessive methanol levels stem from the initial phase of the distillation process, which is commonly known to contain higher methanol concentrations. This understanding is of significant importance in preventing public health incidents.
Acknowledgments
The authors thank the patient and their family for providing informed consent and supporting this publication.
Data availability statement: The datasets generated and/or analyzed during this study are available from the corresponding author upon reasonable request.
Ethics statement: Ethical approval was not required for this case report per institutional guidelines.
Author contributions: T Zhao, XX Wang, LT Duan, FL Hao, and DD Wang: Conceptualization, methodology, investigation. T Zhao, XX Wang, SS Sun, and P Li: Writing—original draft, visualization. T Zhao, XX Wang, and DD Wang: Writing—review & editing, supervision. All authors reviewed and approved the final manuscript.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Jr Bennett IL, Cary FH, Jr Mitchell GL, Cooper MN. Acute methyl alcohol poisoning: a review based on experiences in an outbreak of 323 cases. Medicine (Baltimore). 1953;32(4):431–463.
- Haviv YS, Rubinger D, Zamir E, Safadi R. Pseudo-normal osmolal and anion gaps following simultaneous ethanol and methanol ingestion. Am J Nephrol. 1998;18(5):436–438.
- Marc G, Robert SH, James BM, Valery L. Trends in toxic alcohol exposures in the United States from 2000 to 2013: a focus on the use of antidotes and extracorporeal treatments. Semin Dial. 2014;27(4):395–401.
- Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA; American Academy of Clinical Toxicology Ad Hoc Committee on the Treatment Guidelines for Methanol Poisoning. American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol. 2002;40(4):415–446.
- Ali J, Mostafa M, Leila M, Hesam K, Shreeshivadasan C, Sultan A, et al. Awareness raising and dealing with methanol poisoning based on effective strategies. Environ Res. 2023:228:115886.
- Chan-Seok M. Estimations of the lethal and exposure doses for representative methanol symptoms in humans. Ann Occup Environ Med. 2017;29:44.
- Darren MR, Christopher Y, Bruno M, James FW, Robert M, Sophie G, et al. Recommendations for the role of extracorporeal treatments in the management of acute methanol poisoning: a systematic review and consensus statement. Crit Care Med. 2015;43(2):461–472.
- Tejas D, Aditya S, Usha V, Bakulesh K. Methanol poisoning: predictors of visual outcomes. JAMA Ophthalmol. 2013;131(3):358–364.
- Juha H, Leena V, Kirsi S. Neuroimaging supports the clinical diagnosis of methanol poisoning. Neuroradiology. 2002;44(11):924–928.
- Gaul HP, Wallace CJ, Auer RN, Fong TC. MR findings in methanol intoxication. AJNR Am J Neuroradiol. 1995;16(9):1783–1786.
- Sofie VC, Mariasavina S, Rosamaria A, Brecht VB, Hrvoje V, Luc vdH, et al. Bilateral lesions of the basal ganglia and thalami (central grey matter)-pictorial review. Neuroradiology. 2020;62(12):1565–1605.
- Nirdesh J, Dandu H, Shailendra Prasad V, Anit P. Methanol poisoning: characteristic MRI findings. Ann Saudi Med. 2013;33(1):68–69.
Keywords
Methanol poisoning; Metabolic acidosis; Hemodialysis; Toxic optic neuropathy; Delayed neurotoxicity
Cite this article
Zhao T, Wang XX, Duan L, Li P, Sun S, Hao F, et al. Delayed Visual Sequelae and Hemodialysis Challenges in Severe Methanol Poisoning: A Case Report of Reconsumed Contaminated Chinese Baijiu. Clin Case Rep J. 2025;6(2):1–6.
Copyright
© 2025 Dongdong Wang. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).