Abstract
This article reports a case of a 56-year-old male patient with brain metastasis from breast cancer, and analyzes its diagnostic and therapeutic challenges through a literature review. The patient was admitted to the hospital due to headache and vomiting, and an MRI showed multiple lesions in both cerebellar hemispheres. The pathological diagnosis after surgery confirmed brain metastasis from breast cancer. A new lesion was found one month after surgery. The literature review indicates that brain metastasis from male breast cancer is highly concealed, and most patients present with neurological symptoms at the time of diagnosis, with a poor prognosis (average survival period of 7.4 months). Simple surgical resection is prone to recurrence, and a combination of radiotherapy and chemotherapy is needed. However, due to the blood-brain barrier, there is currently no unified treatment plan. We have summarized the existing case reports and proposed possible treatment directions to provide a basis for the treatment of such patients in the future.
Introduction
Breast cancer is a primary breast tumor, and due to its high mortality and incidence rates, it has become an intractable health problem. About 15%–20% of breast cancer patients will develop metastases, with common metastatic organs being the bone or lung [1,2]. In female patients, only 1.5%–6% will develop brain metastasis, and most have a poor prognosis, with a survival period of about 2 years–4 years [3,4]. Male breast cancer accounts for only 1% of all breast cancers. However, the incidence of brain metastasis is higher in males (approximately 8%–10%), and it is most commonly associated with hormone receptor-positive characteristics [5]. Due to the smaller amount of breast tissue in males, the primary tumor is often neglected, and most patients are diagnosed with advanced-stage disease at the time of diagnosis [6]. In our literature review, we found that the longest survival period of male breast cancer patients with brain metastasis that could be follow-up was 2 years, with an average survival period of 7.4 months. This suggests that the survival period and prognosis of male patients are worse than those of female patients. Currently, there are few case reports of male breast cancer with brain metastasis. In this case report, we provide the clinical data of a rare case of male breast cancer metastasis to both cerebellar hemispheres and analyze it in combination with relevant literature, aiming to provide a reference for the treatment of such patients in the future.
Case Presentation
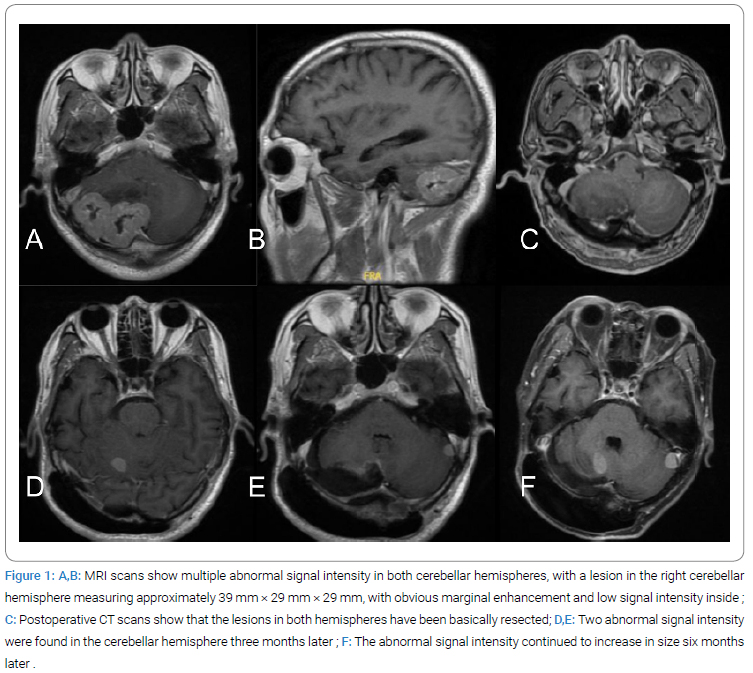
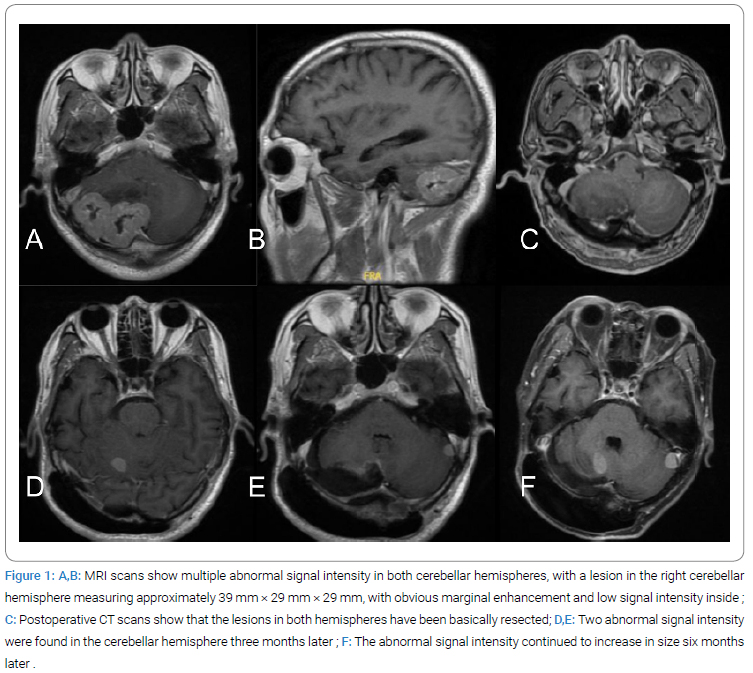
A 56-year-old male patient was admitted to our hospital on December 3, 2023, due to intermittent headaches for 1 year, which worsened with vomiting and blurred vision for half a month. He had a history of a right breast lump for 10 years, which had not attracted attention and had not been treated specifically. At admission, he had cerebellar ataxia: Romberg’s sign was positive, and the finger-to-nose test and heel-to-knee-to-shin test both indicated coordination disorders in the right limbs. Physical examination revealed a right breast lump, about 2 cm in size, of hard texture and poorly mobile. T1-weighted enhanced MRI revealed multiple irregular nodular enhancement lesions in both cerebellar hemispheres (the largest measured 39 mm × 29 mm × 29 mm), accompanied by surrounding edema and mass effect (Figure 1A,Figure 1B). PET-CT showed high-density nodules in the left parieto-occipital junction and both cerebellar hemispheres.
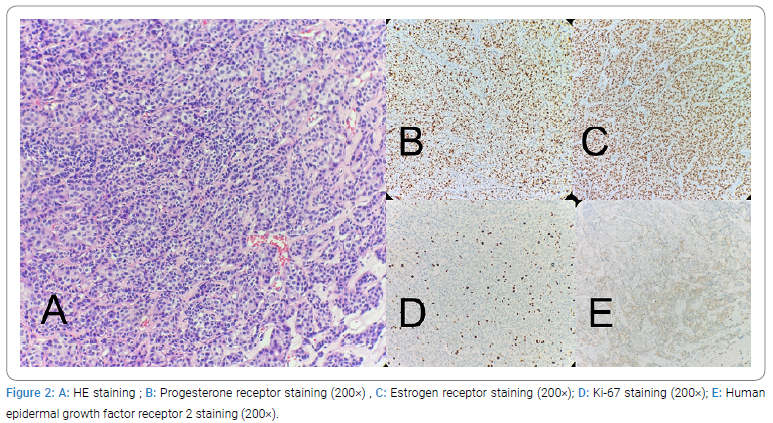
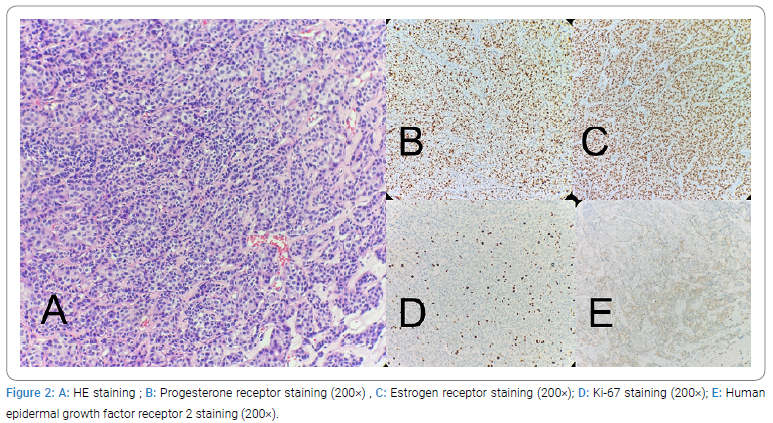
The patient underwent resection of the right cerebellar tumor and excision of the breast lump. The postoperative pathological results were metastatic breast cancer in the cerebellum and breast cancer in the breast. The patient was discharged one week after surgery. One month later, follow-up MRI revealed new multiple brain metastases (Figure 1D,Figure 1E). Six months later, a follow-up MRI (Figure 1F) showed enlargement of the intracranial lesion. The patient received conservative treatment, but his general condition progressively deteriorated. The pathological examination of the cerebellar tumor showed nest-like epithelial cells with small foci of necrosis, consistent with metastatic breast cancer (invasive carcinoma, NOS, histological grade II). Immunohistochemical results showed: Estrogen Receptor (ER,++ in about 80%), Progesterone Receptor (PR,++ in about 60%), Human Epidermal growth factor Receptor 2 (HER2,1+), Epidermal Growth Factor Receptor (EGFR,-), Ki-67 (+ in about 20%) (Figure 2). The pathological diagnosis of the right breast lump was invasive ductal carcinoma (histological grade II), with poor glandular differentiation and rapid proliferation. The immunohistochemical results were consistent between the cerebellar lesion and the breast mass.
Discussion
It has been reported that male Breast Cancer (BC) accounts for about 1% of male cancers and 1% of all breast cancer patients [5]. We searched the PubMed literature database and found a total of 9 case reports of male breast cancer with brain metastasis from 2000 to the present. We summarized and concluded them based on aspects such as age distribution, initial symptoms, recurrence time, immunohistochemical manifestations, pathological features, and prognostic outcomes. The age distribution showed that there was 1 case in the 30 years–50 years age group, 1 case in the over-70 age group, and 7 cases in the 50 years–70 years age group, with the majority concentrated in the 55 years–60 years age range. In terms of clinical manifestations, four patients were first admitted to the hospital due to central nervous system abnormalities, mainly showing dizziness, headache, epileptic seizures, and vomiting, without any previous breast cancer-related symptoms. The remaining 5 cases had a history of breast cancer and had undergone mastectomy, but brain metastasis occurred more than 1 year after treatment (the longest interval could reach 24 years). Among the 9 cases, only 1 case had a single intracranial lesion, and the remaining 8 cases had multiple intracranial lesions. In terms of immunohistochemistry, 5 of the 9 cases were HER2 (-), ER, PR (+); 2 cases were triple-negative HER2 (-), ER, PR (-); 1 case was HER2 (+), ER, PR (+); and 1 case did not report. Five cases reported their pathological types, all of which were invasive ductal carcinoma. It can be seen that most male breast cancer patients with brain metastasis are hormone receptor-positive (ER+/PR+, 77.8%), and most have multiple intracranial metastases (88.9%), indicating a strong tendency for hematogenous dissemination. The analysis of treatment and prognosis found that among the nine patients, only 3 received postoperative radiochemotherapy, of which one was cured, and two died due to poor chemotherapeutic effects and multiple brain metastases. The prognosis of the six patients who did not receive radiochemotherapy was extremely poor, with only one patient surviving for 2 years, and the rest died within 1 year. This suggests that radiochemotherapy may be of significant importance in prolonging overall survival.
A review of the literature reveals that due to the rarity of male breast cancer, research on its brain metastasis is very limited. Therefore, patients with brain metastasis from male breast cancer often do not receive timely diagnosis and comprehensive treatment. In this case, we reported a case of a male patient with brain metastasis from breast cancer who was admitted to the hospital due to central nervous system symptoms. After the resection of the cerebellar tumor, a follow-up cranial CT scan showed no obvious tumor residue (Figure 1C), so we did not adopt radiochemotherapy. Although both the brain metastasis and breast tumor were resected simultaneously, one month later, the cranial CT scan still showed a rapid increase in the size of the brain lesion, which doubled in size after six months (Figure 1F). This indicates that for patients with brain metastasis from male breast cancer, simple surgical resection of the lesion may not achieve good therapeutic effects. Neurosurgery has both diagnostic and therapeutic value in the treatment of brain metastasis, especially for single, large, or space-occupying lesions [7]. In this case, the patient did not receive adjuvant radiochemotherapy after surgery, which may be the main reason for the early recurrence.
Although surgical resection of brain metastases can effectively alleviate central nervous system symptoms, male breast cancer with brain metastasis has a high degree of malignancy and a high probability of recurrence [6]. Therefore, the combined application of postoperative radiochemotherapy is crucial. Studies have shown that the combined treatment of chemotherapy and radiotherapy can significantly delay the recurrence and progression of brain metastasis in breast cancer patients [8]. Chemotherapeutic drugs for breast cancer include alkylating agents (such as cyclophosphamide) and antimetabolites (such as methotrexate and 5-fluorouracil), and later cytotoxic drugs (such as paclitaxel) were introduced [7,9]. For patients with HER 2 positivity, we generally add trastuzumab to the chemotherapy regimen; for patients with ER and PR positivity, we can adopt hormonal therapy [8]. Through the analysis of the collected cases, we found that male patients who only underwent surgical resection all had a very poor prognosis. In contrast, some patients who received radiochemotherapy could be cured, which suggests that we should actively use postoperative chemotherapy. However, at the same time, current chemotherapy regimens are still immature, and a unified treatment plan does not yet exist, which still requires further clinical data research.
Due to the existence of the blood-brain barrier, the therapeutic effect of chemotherapeutic drugs is poor [10]. In recent years, several strategies have been proposed for the Blood-Brain Barrier (BBB), including increasing the dose of chemotherapeutic drugs, applying nanotechnology, and using physical or chemical means to disrupt the blood-brain barrier [11]. For example, by arterial administration or intranasal administration, the concentration of drugs in the brain can be increased, thereby enhancing the therapeutic effect [12]. In addition, intrathecal drug delivery technology has also been used in the treatment of brain metastasis from breast cancer, which can directly deliver drugs into the cerebrospinal fluid, bypassing the blood-brain barrier and significantly increasing the local concentration of drugs. However, the risk of chemical meningitis requires vigilance [10]. Studies have also found that direct intrathecal injection of trastuzumab has a certain therapeutic effect on meningeal metastasis from breast cancer [13]. At the same time, we can use a combination of radiotherapy and chemotherapy. Whole-Brain Radiotherapy (WBRT) can disrupt the blood-brain barrier to a certain extent after treatment, increasing the concentration of chemotherapeutic drugs entering the cranial cavity and thereby enhancing the therapeutic effect of chemotherapy. Studies have confirmed that the application of radiotherapy before chemotherapy for brain metastasis increased the overall response rate by 4%–38% [14,15]. Currently, this field has not yet been fully explored, and a mature diagnostic and treatment plan has not been established [16].
Conclusion
This case provides a case of a male patient with brain metastasis from breast cancer. Due to its low incidence and high concealment, it is often discovered. Coupled with the high recurrence rate of brain metastasis, the prognosis is worse than that of female patients. Simple surgical resection is not sufficient to effectively control the progression of the disease. Surgical resection combined with postoperative Whole-Brain Radiotherapy (WBRT) or SRS is critical in controlling local recurrence. The combination of targeted drugs and intrathecal chemotherapy may be effective for patients with brain metastasis from male breast cancer.”
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Cite this article
Wang Z, Guan C, Wu J, Chen Y, Feng Y, Cui Z, et al. A Case Report of Male Breast Cancer with Brain Metastasis and Literature Review. Clin Case Rep J. 2025;6(2):1–5.
Keywords
Male breast cancer; Brain metastasis; Literature review; Radiochemotherapy
Copyright
© 2025 Pin Guo. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).