Hepatitis B Virus-Associated Focal and Segmental Glomerular Sclerosis: A Rare Case of Tip Variant
* Amel Harzallah;
Karray Rahma;
Hedri Hafedh;
Hajji Mariem;
Goucha Rim;
Ben Hamida Fethi;
Gorsane Imen;
Abderrahim Ezzeddine;
-
* Amel Harzallah: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Karray Rahma: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Hedri Hafedh: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Hajji Mariem: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Goucha Rim: Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Ben Hamida Fethi: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Gorsane Imen: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
Abderrahim Ezzeddine: Department of Medicine A, Charles Nicolle Hospital, Tunis, Tunisia; Laboratory of Renal Pathology LR00SP01, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia.
-
May 13, 2022 |
-
Volume: 3 |
-
Issue: 4 |
-
Views: 2890 |
-
Downloads: 2254 |
Abstract
Introduction: Glomerular involvement is a common renal complication associated with Hepatitis B infection. Although membranous nephropathy is the pathology most frequently encountered, other glomerular diseases, such as focal and segmental glomerulosclerosis (FSGS), are rare. We report a rare case of hepatitis B-associated FSGS.
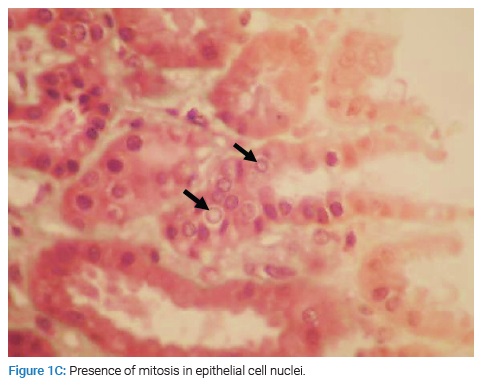
Case Report: A 48-year-old man, an inactive carrier of HBV from 2013, presented a 1-month history of generalized edema. Clinical examination revealed edema of the lower extremities associated with reduced breathing sounds at the base of the lung. The urine dipstick showed hematuria (++) with proteinuria (+++). Laboratory data revealed features of nephrotic syndrome (serum albumin, 18 g/l; proteinuria, 19 g/day) and acute kidney injury (serum creatinine, 124 umol/l). He had a normal hepatic check. Quantitative and qualitative HBV DNA was at 2.84 x 102 UI/ml. The screening for other infections was negative. Renal histology showed an FSGS-type ‘tip lesion’ associated with tubular lesions. Treatment combined a loop diuretic, angiotensin-converting enzyme inhibitor, oral anticoagulation, and antiviral treatment with Entecavir (0.5 mg/day). After two months of antiviral treatment, his biological markers improved with undetectable viral DNA.
Conclusions: FSGS is a podocytopathy that can be rarely associated with an active viral infection such as HBV. His management differs from primary FSGS, which is based on nucleotide analogs with good responses.
Abbreviations
HBV: Hepatitis B Virus; FSGS: Focal and Segmental Glomerulonephritis; HIV: Human Immunodeficiency Virus; BMI: Body Mass Index; STAT: Transcription Factors Located in the Cytoplasm.
Introduction
Chronic Hepatitis B Virus (HBV) infection is the most common chronic viral infection in the world, affecting more than 400 million people, more than double the prevalence of chronic Human Immunodeficiency Virus (HIV) and hepatitis C carriers combined [1]. Renal disease may occur in 3% to 5% of patients with chronic HBV infection [2]. HBV is associated with a broad spectrum of renal diseases such as membranous glomerulonephritis, membranoproliferative glomerulonephritis, polyarteritis nodosa, and direct focal and segmental glomerulonephritis (FSGS). The most common HBV-related renal disease is membranous glomerulonephritis. The association of FSGS with HBV is rare, with only a few cases described in the literature. We report herein a further case of hepatitis B infection associated with FSGS.
Case Presentation
A 48-year-old man investigating nephrotic syndrome presented a 1-month history of progressive generalized edema. He had a history of inactive carriage of HBV for five years. Hepatitis B was discovered following a blood donation. On this date, the hepatitis B markers showed positive Hepatitis B surface antigen (Hbs Ag), positive anti-Hbc antibodies, and undetectable viral DNA.
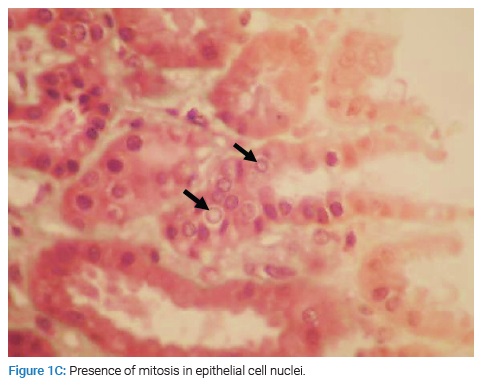
The patient reported no use of medications, no fever or skin lesions, and no family history of nephropathy. Clinical examination revealed lower extremity edema with reduced breath sounds in the bases of the lung. The patient weighed 67 kg, had a height of 1.78 m (BMI 21.1), and was normotensive. The urine dipstick showed hematuria (++) with proteinuria (+++). Laboratory data (Table 1) showed serum creatinine: 124 µmol/L (reference range 54 µmol/l–95 µmol/l); total cholesterol: 7.17 mmol/L (reference range 3.2 mmol/L–5.18 mmol/L) and serum albumin: 1.8 g/dL (reference range 3.5 g/dL–5.0 g/dL). His proteinuria was 19 g/day, and urinalysis had 10,000 leucocytes and 20,000 erythrocytes. Serology revealed HBsAg positivity. HBV DNA analysis showed 2.84 x 102 UI/ml. The screening for other viral infections such as Hepatitis C Virus, HIV, Epstein Barr Virus, and Cytomegalovirus was negative. Serum complement levels were normal.
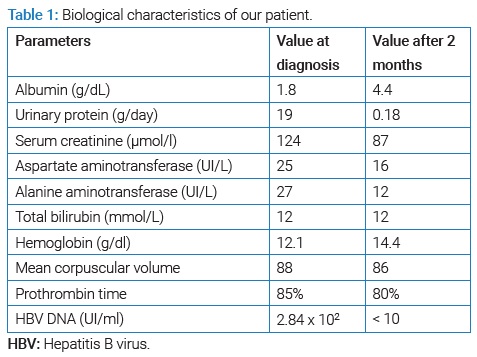
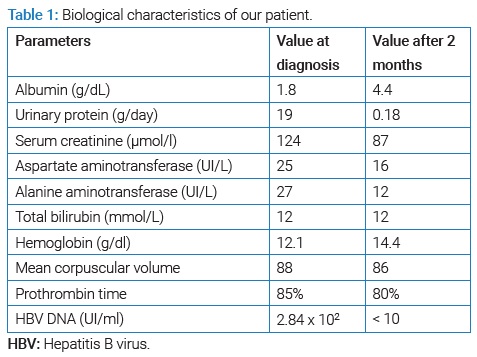
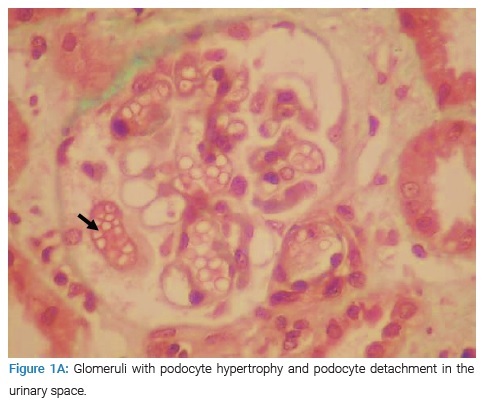
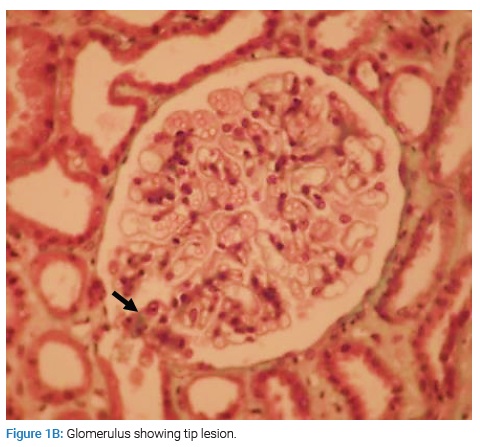
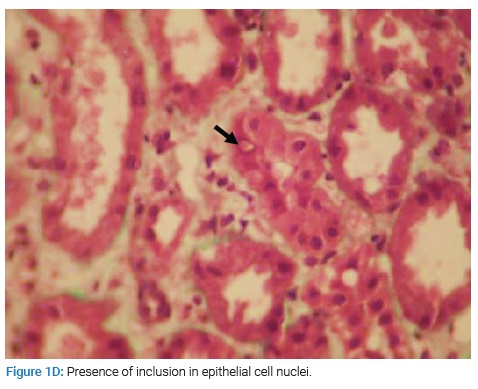
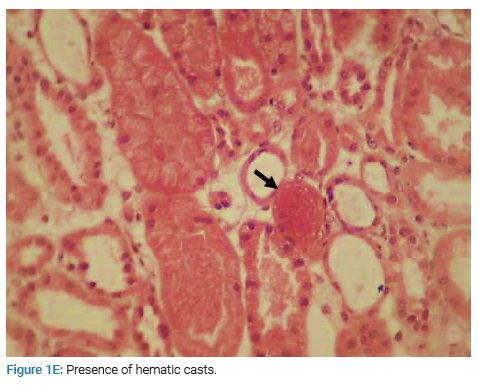
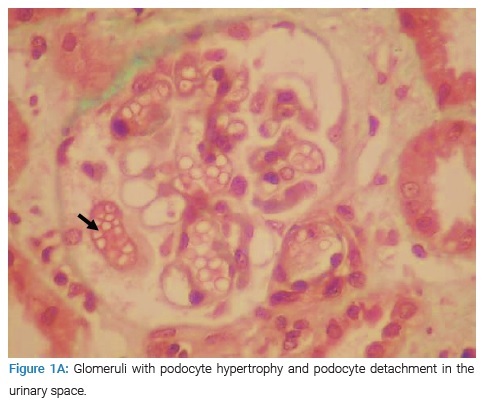
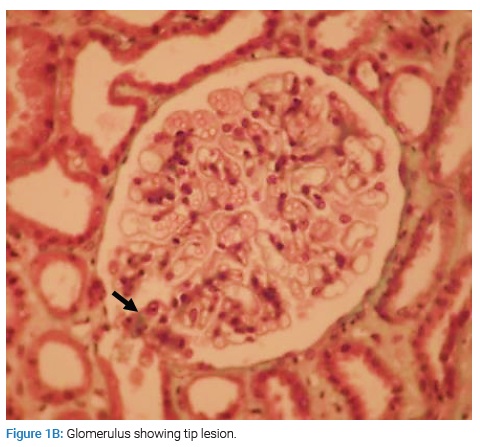
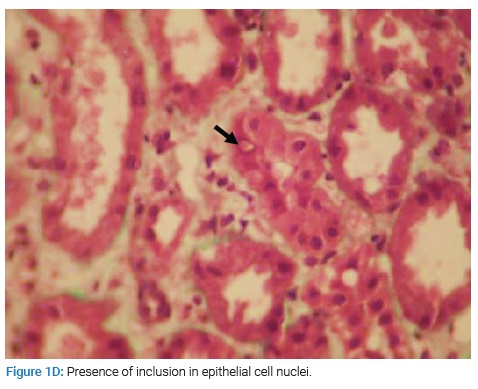
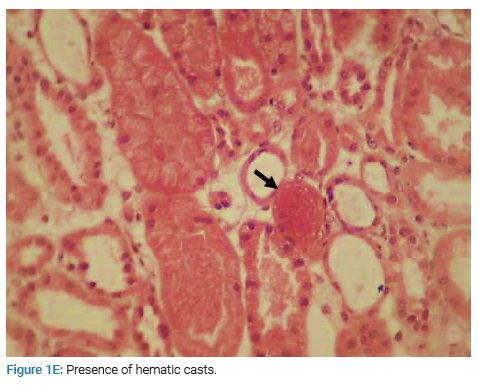
The patient underwent a renal biopsy. There were 21 glomeruli for analysis by light microscopy. The mesangial matrix was mildly increased. Some glomeruli had podocyte hypertrophy and podocyte detachment in the urinary space (Figure 1A), with a glomerulus showing a tip lesion (Figure 1B). Some tubes had a vacuolated or flattened epithelium. In addition, there was the presence of mitosis (Figure 1C) and inclusions in some epithelial cell nuclei (Figure 1D) and the presence of hyaline and hematic casts (Figure 1E). There was no tubular atrophy; neither tubular necrosis nor interstitial fibrosis was present.
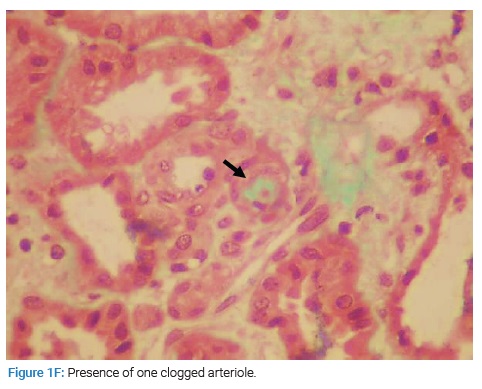
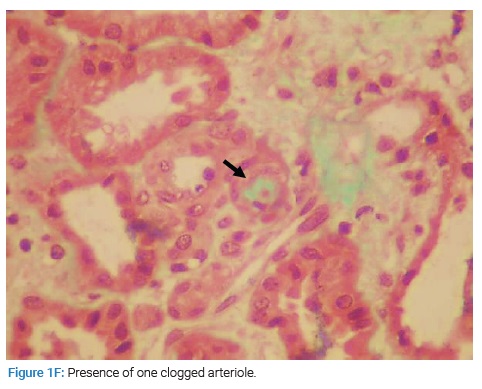
Small-caliber vessels were the seat of parietal hyaline deposits in the vascular compartment with one clogged arteriole, and some vessels of larger calibers presented fibrous parietal thickening (Figure 1F).
Immunofluorescence analysis showed mesangial IgM deposits and was negative for IgA and IgG. Unfortunately, electron microscopy was not performed because it is unavailable in our hospital.
After ruling out other causes of secondary FSGS, he was diagnosed with hepatitis B-associated FSGS.
The patient was started on Captopril, furosemide, and oral anticoagulation with Acenocoumarin. He also received antiviral treatment with Entecavir at a 0.5 mg/day dose. Immunosuppressive therapy was not applied.
After two months, the features of the nephrotic syndrome resolved (Table 1), and proteinuria decreased to 0.18 g/day. Viral DNA was undetectable on analysis. Currently, the patient is well on clinical follow-up. Unfortunately, he is still in remission and continues on Entecavir for two years.
Discussion
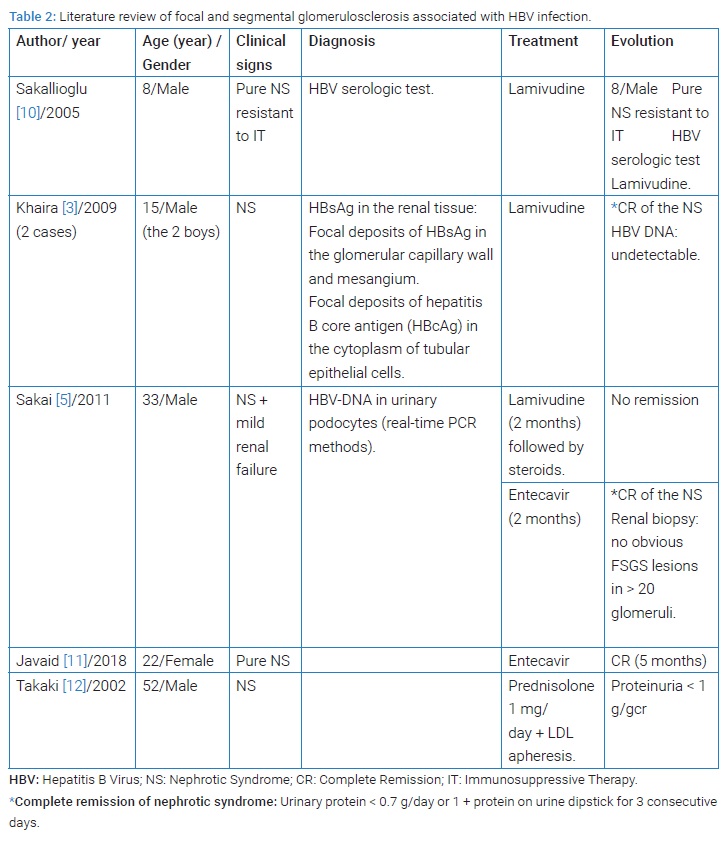
HBV-associated nephropathy is one of the most common extrahepatic manifestations of HBV infection extrahepatic manifestations. Several morphological patterns of renal disease, including membranous nephropathy, membranoproliferative glomerulonephritis, mesangial proliferative glomerulonephritis, minimal change disease, IgA nephropathy, and rarely FSGS, have been described in association with HBV infection [3]. In adults, chronic HBV infection is usually related to membranous nephropathy. Some reports in the literature have described an association between FSGS and HBV (Table 2).
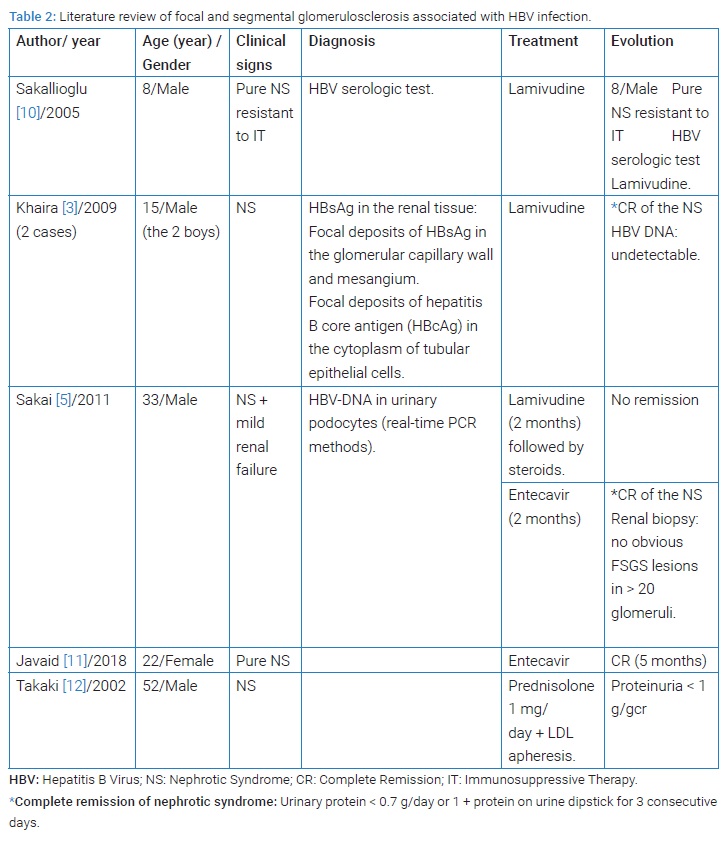
The tip variant FSGS is extremely rare, and, to our knowledge, few cases have been reported in association with chronic HBV infection. The pathogenesis of HBV-related nephropathy is not fully understood. Immune complex-mediated mechanisms are thought to play a central role which could explain the occurrence of membranous nephropathy, membranoproliferative glomerulonephritis, and IgA nephropathy [3]. Immune deposits may be formed from the deposition of an IgG immune complex with one or more viral antigens or with the de novo formation of an immune complex after the deposition of the circulating antigen in the basement membrane first, followed by deposition of the circulating antibody [4].
In addition to immune complex-mediated damage in the HBV-associated FSGS, other pathogenic pathways of podocyte damage and loss are also associated [3]. Some authors thought that HBV injures podocytes like HIV. Sakai et al. supported this hypothesis by identifying HBV DNA in the podocyte (real-time PCR method) [5]. Some research in children indicated that the number and density of podocytes decreased significantly in patients with HBV glomerulonephritis. This was usually accompanied by increases in urinary protein [6]. A recent study suggests that the HBV-produced X protein decreases nephrin expression and induces podocyte apoptosis by activating STAT3 (transcription factor located in the cytoplasm) [7]. Like our patient, all the other cases reported in the literature had active HBV infection [8]. Concerning these data, direct virus infection seems to play an essential role in the occurrence of HBV-FSGS. The criteria to link the acute onset of FSGS to acute viral infections are very complex and difficult.
The diagnosis of virus-related nephropathy is based mainly on detecting specific antigens in blood or any other body sample and the identification of viral antigens in glomerular structures and the clinical and histological picture. In our case, detection of viral antigens was not available. Therefore, the diagnosis of FSGS-HBV was made retrospectively after remission of nephrotic syndrome with viral treatment alone and after exclusion of other differential diagnoses. Epidemiologically, most of the patients in the previous studies were young men (mean age of 18.6 years), while our patient was the oldest one (48 years). They all presented with nephrotic proteinuria (Table 2).
The management of FSGS-HBV is unclear. The recent guidelines do not provide specific recommendations on this entity. However, they recommend that patients with replicative HBV infection (defined by HBV DNA levels > 2000 IU/ml) and glomerulonephritis receive treatment with nucleoside analogs as recommended for the general population by standard clinical practice guidelines for HBV infection [9]. In fact, in the case of glomerulonephritis related to HBV infection, immunosuppressive treatment can be very harmful. It may enhance viral replication and flare-up hepatic disease. Lamivudine has been the most widely used agent in nephrotic patients with an FSGS with good clinical response. However, lamivudine monotherapy can lead to a somatic mutation of HBV that leads to the development of resistance [4]. Entecavir and tenofovir are now preferred as first-line therapy [4], as this was the case in our patient.
Conclusions
Focal and Segmental Glomerulonephritis-Hepatitis B Virus (FSGS-HBV) is a rare disease that complicates an active viral infection. It usually affects young male patients. The clinical feature is nephrotic proteinuria. The management is different from primary FSGS. In case of resistance, it is based on nucleotide analogs, including lamivudine or entecavir. Remission is usually obtained after an average of two months (the time required to inhibit viral replication). For this reason, patients with proteinuria suggesting a glomerular disease should be tested for HBV infection.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Zampino R, Boemio A, Sagnelli C, Alessio L, Adinolfi LE, Sagnelli E, et al. Hepatitis B virus burden in developing countries. World J Gastroenterol. 2015;21(42):11941–11953.
- Gupta A, Quigg RJ. Glomerular Diseases Associated with Hepatitis B and C. Adv Chronic Kidney Dis. 2015;22(5):343–351.
- Khaira A, Upadhyay BK, Sharma A, Das P, Mahajan S, Makhariya G, et al. Hepatitis B virus-associated focal and segmental glomerularsclerosis: report of two cases and review of literature. Clin Exp Nephrol. 2009;13(4):373–377.
- Kupin WL. Viral-Associated GN. Clin J Am Soc Nephrol. 2017;12:1529–1533.
- Sakai K, Morito N, Usui J, Hagiwara M, Hiwatashi A, Fukuda K, et al. Focal segmental glomerulosclerosis as a complication of hepatitis B virus infection. Nephrol Dial Transplant. 2011;26(1):371–373.
- Zhang Y, Zhou J, Wang H. Podocyte depletion in children with hepatitis B virus-associated membranous nephropathy. Zhonghua Er KeZaZhi. 2007;45(5):344–348.
- Lei XY, Chen XX, Sun YH, Gao MD, Hu XX, Suo YH. Hepatitis B virus X protein decreases nephrin expression and induces podocyte apoptosis via activating STAT3. Exp Ther Med. 2019;17(5):4223–4229.
- Khedmat H, Taheri S. Associations of various histological morphologies of renal involvement in hepatitis B infection: Analysis of 118 subjects. Saudi J Kidney Dis Transpl. 2010;21(5):964–966.
- KDIGO. Clinical practice guideline on glomerular diseases [Internet]. New York: KDIGO; 2020.
- Sakallioglu O, Gok F, Kalman S, Kurekci AE, Gunhan O, Gokcay E. Hepatitis B complicated focal segmental glomerulosclerosis. J Nephrol. 2005;18(4):433–435.
- Javaid MM, Khatri P, Subramanian S. Should antiviral monotherapy with nucleotide analogs be the primary treatment option for focal segmental glomerulosclerosis-related nephrotic syndrome in chronic hepatitis B infection? Saudi J Kidney Dis Transpl. 2018;29(3):714–718.
- Takaki A, Nakatsuka A, Satou C, Iwata Y, Ikeda H, Fukushima M. A case of focal segmental glomerulosclerosis (FSGS) complicated with chronic hepatitis B and treated with steroid and LDL apheresis. Nippon Jinzo Gakkai Shi. 2002;44:806–812.
Keywords
Hepatitis B virus; Glomerulonephritis; Focal segmental glomerular sclerosis
Cite this article
Harzallah A, Karray R, Hafedh H, Mariem H, Goucha R, Hamida BF, et al. Hepatitis B virus-associated focal and segmental glomerular sclerosis: a rare case of tip variant. Clin Case Rep J. 2022;3(4):1–5.
Copyright
© 2022 Amel Harzallah. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).