Abstract
Crohn’s Disease (CD) is a complex inflammatory disease of the gastrointestinal tract, which is often associated with Extra-Intestinal Manifestations (EIMs). The estimated prevalence of ocular manifestations in patients with CD is 3.5%–6.8%, with uveitis, episcleritis, and scleritis comprising most of these cases. Orbital Myositis (OM) is an exceedingly rare ocular EIM which has also been reported. We present a case of a 22-year-old female patient with CD on ustekinumab monotherapy in clinical remission, which was found to have bilateral orbital myositis as an EIM of her CD.
Abbreviations
CT: Computed Tomography; CD: Crohn’s Disease; EIM: Extra-Intestinal Manifestation; OM: Orbital Myositis; c-ANCA: Cytoplasmic Antineutrophil Cytoplasmic Antibodies; p-ANCA: Perinuclear Antineutrophil Cytoplasmic Antibodies; IgG-4: Immunoglobulin-4; ACE: Angiotensin Converting Enzyme
Introduction
Crohn’s Disease (CD) is a complex inflammatory disease of the gastrointestinal tract, which can be associated with extra-intestinal manifestations (EIMs). The estimated prevalence of EIMs in patients with CD is 25%–70% [1–3]. EIMs are commonly musculoskeletal but also include dermatologic, hepatobiliary, and ocular manifestations [2]. The estimated prevalence of ocular manifestations in patients with CD is 3.5%–6.8%, with uveitis, episcleritis, and scleritis comprising the majority of these cases [3]. Orbital myositis (OM)—characterized by inflammation of the extra-ocular muscles resulting in periorbital pain worse with eye movement, eyelid swelling, conjunctival chemosis, and ophthalmoplegia—is a rare ocular EIM associated with CD [4–7]. We describe a case of a patient with CD believed to be in clinical remission on ustekinumab who was diagnosed with bilateral, sequential OM without any evidence of gastrointestinal luminal disease activity. Management implications of CD in a patient with OM, which is not historically known to mirror disease activity, are unclear.
Case Presentation
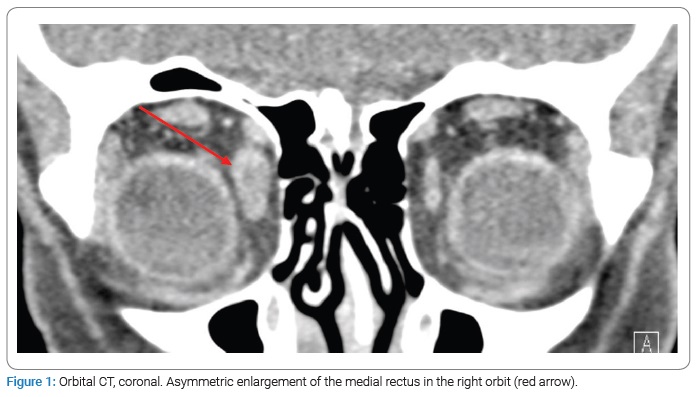
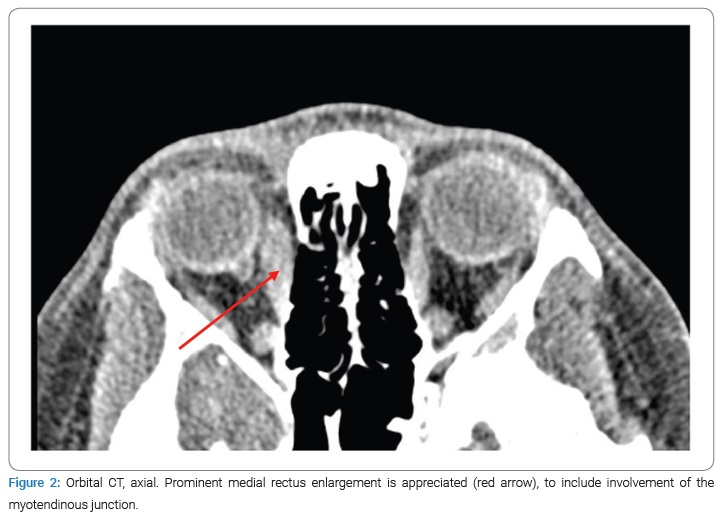
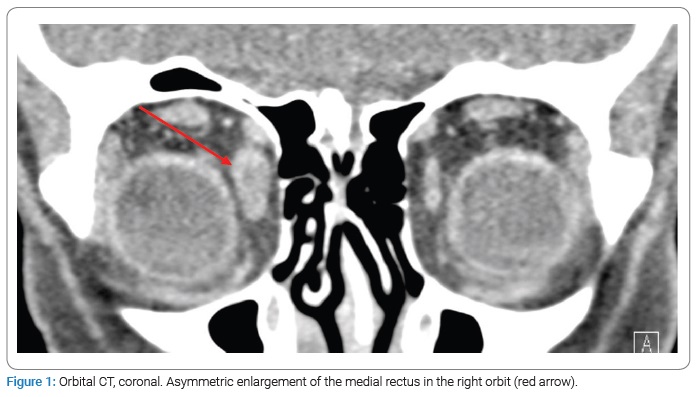
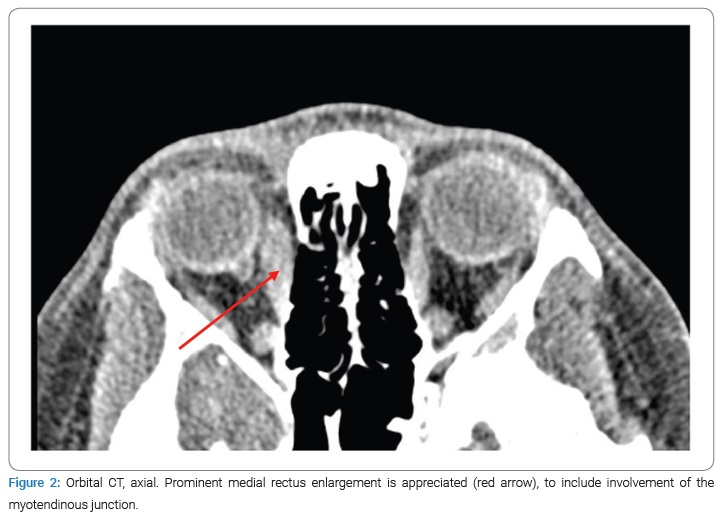
A 22-year-old female with colonic Crohn’s Disease (CD) on ustekinumab monotherapy every eight weeks for maintenance of remission presented to the emergency department with three days of right eye swelling and pain with eye movement. She had been diagnosed with CD four years prior. She was initially treated with infliximab as well as azathioprine, which was added to reduce immunogenicity. Her azathioprine was eventually discontinued after one year. After about two years of therapy and one year prior to this presentation, she was transitioned to ustekinumab due to infusion reactions with infliximab. While in the emergency department, a Computed Tomography (CT) of the orbits was performed. Minimal pre-septal tissue swelling of the right orbit without evidence of orbital cellulitis was reported. She was started on Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and sent home from the ED without an ophthalmology consultation. Two weeks later, the patient presented to the ophthalmology clinic with a resolution of her right eye symptoms but new, similar symptoms in her left eye. Exam findings demonstrated mild restriction of lateral and medial gazes, painful eye movement, and chemosis of the lateral conjunctiva. She denied gastrointestinal symptoms concerning a Crohn’s flare or other EIMs. The oculoplastic surgeon reviewed the initial orbital CT images, and subtle enlargements of multiple extra-ocular muscles in the right orbit were noted (Figure 1,Figure 2). At this time, the diagnosis of bilateral, sequential OM was made. After a discussion with her gastroenterologist, she was started on prednisone 40 mg daily, resulting in a complete resolution of her symptoms at her one-week follow-up visit.
Further work-up for her OM revealed a positive Antinuclear Antibody (ANA) with an elevated erythrocyte sedimentation rate. Complete blood count, complete metabolic panel, stimulating thyroid hormone, and free T4, Cytoplasmic Antineutrophil Cytoplasmic Antibodies (c-ANCA), Perinuclear Antineutrophil Cytoplasmic Antibodies (p-ANCA), Immunoglobulin G-4 (IgG-4), and an Angiotensin-Converting Enzyme (ACE) level were normal. She continued ustekinumab maintenance therapy as she remained in clinical remission without evidence of other EIMs. She completed the steroid taper and was informed of the high recurrence rate of CD-associated OM.
Discussion
Orbital myositis is an inflammatory condition that is most commonly idiopathic but can occur in the setting of autoimmunity, neoplasm, trauma, or infection [5,9]. Acute, idiopathic OM usually has a quick onset and similarly rapid response to oral steroids without clinical, laboratory, or radiographic evidence of other causes. Contrast-enhanced imaging will show involvement of the myotendinous junction in most cases. Autoimmune conditions associated with OM include Thyroid Eye Disease (TED), Inflammatory Bowel Disease (IBD), IgG4-related disease, sarcoidosis, Systemic Lupus Erythematosus (SLE), rheumatoid arthritis, and ANCA-associated vasculitides [9]. Several drugs have been implicated in causing OM, including immune checkpoint inhibitors, alemtuzumab, bisphosphonates, and statins [9]. Paraneoplastic OM has been reported in breast cancer patients seminoma, non-Hodgkin lymphoma, as well as lung and gastric malignancies [9]. The most common infectious etiology for OM is herpes zoster ophthalmicus [9]. Lyme disease, Whipple disease, Coxsackie virus, COVID-19, and cysticercosis have also been implicated [9].
Distinguishing between IBD-associated OM and OM due to other causes requires careful attention and investigation. A literature review revealed that most patients with IBD-associated OM have bilateral eye involvement [9]. Our patient had bilateral, sequential orbital involvement and a negative laboratory evaluation for thyroid disease, vasculitides, sarcoidosis, and IgG4-related disease. The positive ANA, which in itself is a highly non-specific finding, is believed to be most likely a consequence of the patient’s inflammatory bowel disease, as over 20% of females with IBD may have positive antinuclear antibodies. History of treatment with anti-TNF therapy, in particular, has also been shown to increase the probability of seroconversion to ANA positivity [21]. Given our ultimate findings, we strongly suspect that our patient’s OM is an EIM of her CD.
CD-associated OM is believed to arise from immune complex-mediated cross-reactivity between colonic mucoproteins and orbital muscles [8,10]. The muscle most commonly affected is the medial rectus muscle [9]. A literature review revealed that OM occurs independently of gastrointestinal luminal disease activity, with multiple case reports of OM occurring in active disease but also during clinical remission, as well as years before any reported gastrointestinal symptoms [8,11,12].
Systemic corticosteroids are the mainstay of treatment for acute OM [13]. Typically, 1 mg/kg/day of oral prednisone for 1 week–2 weeks is recommended, followed by a slow taper over 6 weeks–12 weeks [13]. Our patient was already on immunomodulatory therapy, so she received a lower prednisone dose. Taper duration is based on the initial severity of the disease and clinical response [14]. In most cases, there is recovery and remission within days to weeks after initiating steroid therapy [13]. In severe cases of compromised vision, pulse-dosing with intravenous methylprednisolone is recommended [15]. Despite successful clinical response to steroids in at least 60%–70% of cases [16], there is a disease recurrence in over a third of patients [17]. Resistance to steroids is common in patients with IBD-associated OM [9]. In both steroids, non-responsive and recurrent diseases and alternative therapies include antimetabolites, alkylating agents, rituximab, and tumor necrosis factor-alpha inhibitors [9,18–20]. Our patient’s symptoms resolved immediately after starting corticosteroids, and escalation of therapy was not required.
In summary, this case illustrates orbital myositis, a rare CD EIM that occurred bilaterally and sequentially in a patient whose CD was in clinical remission. The list of potential causes of OM is long, and a multidisciplinary effort is crucial to complete a thorough evaluation and determine the proper treatment. Because OM does not mirror gastrointestinal luminal disease activity and the patient was still in clinical remission, therapy adjustment was not pursued. This case reiterates the importance of establishing a timely diagnosis, completing a comprehensive evaluation with assistance from other subspecialty providers, and coordinating close follow-up to ensure continued clinical remission and prevention of recurrence.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Inflammatory bowel disease; Crohn’s disease; Extra-intestinal manifestation; Autoimmune
Cite this article
Robertson IR, Pak KC, Harvey MM, Topping KL, Wilkerson RC, Cheatham JG. A Rare case of bilateral, sequential orbital myositis as an extra-intestinal manifestation of crohn’s disease. Clin Case Rep J. 2022;3(8):1–4.
Copyright
© 2022 Robertson IR. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).